- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Managing Rare Thrombotic Events Following COVID-19 Vaccination
A single-center, retrospective study examined the management of thrombotic events in patients presenting with thrombocytopenia following vaccination against COVID-19.
The early identification of thrombocytopenia and thrombosis (VITT) and immune thrombocytopenia (ITP) after vaccination against COVID-19 were crucial for successfully caring for patients presenting with thrombocytopenia, according to a recent study published in Research and Practice in Thrombosis and Haemostasis.1
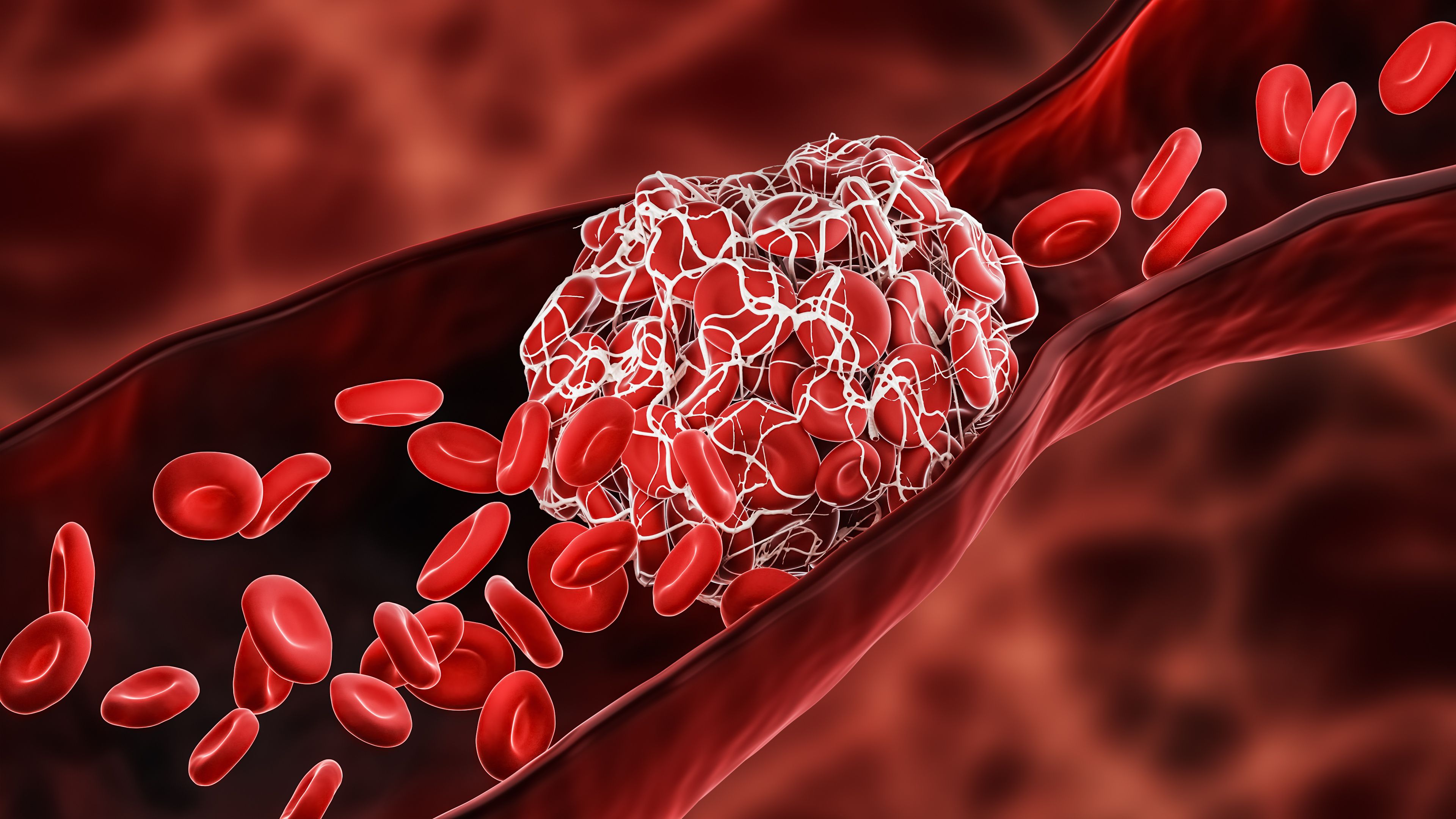
Blood Clot Model | image credit: Matthieu - stock.adobe.com
The study authors reflected on emerging evidence of thrombocytopenic and thrombotic events in some patients after receiving a COVID-19 vaccination. While rare, VITT and ITP following vaccination require urgent evaluation and therapy initiation.2
Despite emerging data on the occurrence of VITT and ITP following vaccination, there is insufficient information available pertaining to the long-term management of these events, the authors explained.1
To better understand these adverse hemolytic events, treatment approaches, the diagnostic process, and to address the shortcomings in literature, the researchers reported on patients at a tertiary care center in Canada who presented with thrombocytopenia following their COVID-19 vaccine.
Nine adult patients with new-onset thrombocytopenia at The Ottawa Hospital between April 1, 2021, and May 31, 2021, were retrospectively reported on. These presentations of thrombocytopenia began between 4 and 42 days after receiving a COVID-19 vaccine, which included the Pfizer-BioNTech mRNA, Moderna mRNA, and Astra Zeneca adenovirus vector-based vaccines.
The treatment regimens for VITT and ITP included a corticosteroid approach with daily prednisone at a dose of 1 mg/kg over the initial few days before tapering over the next 2-3 months. For VITT, it was also recommended to administer non-heparin anticoagulation; some cases can necessitate intravenous immunoglobulin (IVIG).
Additionally, 4-42 days prior to patients’ symptom onset, heparin-induced thrombocytopenia (HIT) testing was sent for individuals with a COVID-19 vaccination record and a platelet count under 150. This testing utilized the Immucor PF4 Enhanced enzyme-linked immunosorbent assay (ELISA) to assess for anti-PF4 autoantibodies. If a patient registered a positive PF4 binding assay, the serotonin release assay (SRA) was performed as a confirmation test for VITT.
The 9 included patients had an average age of 55 years, with a close-to-equal gender distribution. The majority of patients received the Astra Zeneca vaccine (n = 7) while the others received Pfizer (n = 2). No one had been exposed to heparin and all patients were negative for COVID-19 infection.
Positive results from the HIT ELISA tests came back for 3 patients and further testing with SRA diagnosed VITT in a 4th patient. There were 5 patients who went on to develop ITP—4 of whom did not have an associated thrombosis. The fifth patient had a history of ITP and was diagnosed with deep vein thrombosis.
All patients who developed VITT stayed oral anticoagulation treatment following 9 months of treatment. Three of the 4 patients with VITT were admitted to the hospital and subsequently treated with corticosteroids, non-heparin parenteral anticoagulation, and IVIG. The authors observed that patient 1 had a good response to treatment; however, this was not the case in patients 2 or 3. Patient 2 endured recurrent thrombocytopenia throughout their steroid taper and needed to be readmitted for steroids and IVIG. The third patient experienced 2 incidences of cerebral venous sinus thrombosis (CVST) progression and refractory thrombocytopenia. Their hospital stay lasted 15 days and their complications required 7 treatments of plasma exchange. While patient 4 was not admitted to the hospital, they did receive outpatient treatment with a DOAC for pulmonary emboli, to which they responded well.
Of the 5 patients who went on to develop ITP, 1 experienced success treating their condition with eltrombopag and apixaban as an outpatient, but the remaining 4 were admitted to the hospital.
Patients with VITT all continued to get their next round of the COVID-19 mRNA vaccine, whereas all patients except for 2 who had ITP continued with the next vaccine round. Of the 2 who did not have their next dose, 1 declined because of their experience with adverse hematologic events and the other was not recommended to continue because of their history of thrombocytopenia following their previous vaccine doses.
“Early identification was key to the successful management of VITT and ITP events following COVID-19 vaccination. The patient cases described in our study add to the currently limited literature on long-term management of VITT and ITP, particularly in refractory cases, and provides guidance around future COVID-19 vaccinations,” the authors concluded.
Reference
1. Ge M, Ladha D, Lymer J, et al. Thrombocytopenia with and without thrombosis following covid-19 vaccination: long-term management. Res Pract Thromb Haemost. Published online February 29, 2024. doi: 10.1016/j.rpth.2024.102357
2. Vaccine-induced immune thrombotic thrombocytopenia. American Society of Hematology. Updated May 9, 2022. Accessed March 12, 2024. https://www.hematology.org/covid-19/vaccine-induced-immune-thrombotic-thrombocytopenia
First Subcutaneous Prophylaxis for Hemophilia A and B With Inhibitors Approved by FDA
December 23rd 2024The approval of concizumab-mtci (Alhemo) injection marks a significant milestone in managing hemophilia A and B with inhibitors by preventing or reducing bleeding episodes in adults and children 12 years and older.
Read More
