- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Mailed FIT Outreach Boosts CRC Screening in Medicaid Patients, Study Finds
Patient navigation and mailed outreach improved colorectal cancer screening rates in rural clinics, but follow-up colonoscopy participation remains low.
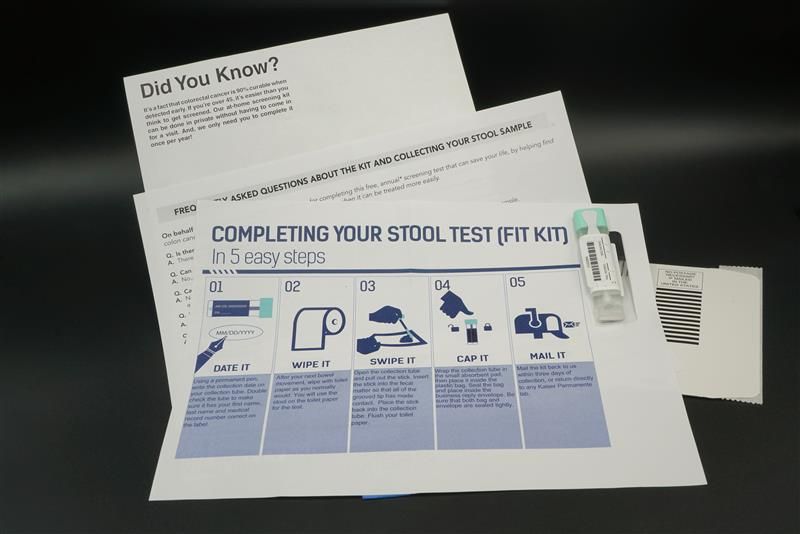
Combining mailed fecal immunochemical test (FIT) outreach with patient navigation significantly increased colorectal cancer (CRC) screening rates among Medicaid enrollees in rural clinics, according to one study. Despite the improvement, overall participation, especially follow-up colonoscopy after abnormal results, remained a critical gap in care.
This cluster randomized trial is published in JAMA Network Open.
“Our findings add to a growing body of literature on the effectiveness of mailed FIT outreach and underscore the continued need to address low participation in follow-up colonoscopy among individuals with abnormal stool-test results,” wrote the researchers of the study.
FITs have become highly popular screening tools for CRC, since they are more accessible to patients who aren’t local to a clinic that can perform colonoscopies or who are at lower risk of CRC.2 One analysis found that commercial FITs could achieve similar diagnostic results compared with the new stool DNA test, which is in line with the first generation of stool DNA and multitarget stool RNA testing.2
In this study, the researchers aimed to evaluate the effectiveness and real-world implementation of a collaborative program between Medicaid health plans and rural clinics that combined mailed FIT outreach with patient navigation to colonoscopy after an abnormal FIT result, delivered as part of routine care.1
This trial was conducted across 28 rural clinic units in Oregon, affiliated with 3 Medicaid health plans. Clinics were randomized to either the intervention group (n = 14) or usual care (n = 14). The study population included Medicaid enrollees aged 50 to 75 years who were due for CRC screening. From May 11, 2021, to June 4, 2022, the intervention group received a stepwise program consisting of mailed FIT outreach followed by patient navigation to colonoscopy for those with abnormal FIT results. Implementation support for clinics included practice facilitation, training, collaborative learning, and patient tracking tools.
The primary outcome was completion of any CRC screening within 6 months of eligibility determination, with follow-up colonoscopy completion after an abnormal FIT result as a secondary outcome. Implementation outcomes included the proportion of eligible enrollees who were mailed a FIT and received advance notification or a reminder, as well as the proportion with an abnormal FIT who were offered navigation services.
The study included 5614 Medicaid enrollees, with 2613 in intervention clinics and 3001 in usual care clinics. The mean (SD) age was 58.2 (5.5) years, and the majority were aged 50 to 64 years (88.0%), female (52.5%), White (67.2%), and residing in rural areas (79.4%). The intervention group demonstrated a significantly higher adjusted 6-month CRC screening completion rate compared with usual care (11.8% vs 4.5%; difference, 7.3 [95% CI, 5.3-9.2] percentage points).
As for implementation, all 1489 eligible enrollees received mailed FIT outreach, 88.5% received advance notification, 78.1% received reminders, and 57.9% of those with abnormal FIT results were offered patient navigation services.
However, the researchers noted some limitations to the study, which include the potential undercapture of screening in claims data, though low disenrollment (4.4%) likely minimized this issue. Additionally, the individual effects of advance notifications and reminders were not assessed.
Despite these limitations, the researchers believe the study suggests that mailed FIT outreach and patient navigation boosted CRC screening among Medicaid enrollees.
“More efforts are needed to address low participation in both FIT testing and follow-up colonoscopy,” wrote the researchers of the study. “Future research might explore how to reach individuals for preventive care who are enrolled in Medicaid but do not have an established primary care clinic.”
References
1. Coronado GD, Petrik AF, Leo MC, et al. Mailed outreach and patient navigation for colorectal cancer screening among rural Medicaid enrollees: a cluster randomized clinical trial. JAMA Netw Open. 2025;8(3):e250928. doi:10.1001/jamanetworkopen.2025.0928
2. Bonavitacola J. Commercial FIT capable of similar diagnostic results as new stool DNA test. AJMC. November 19, 2024. Accessed April 7, 2025. https://www.ajmc.com/view/commercial-fit-capable-of-similar-diagnostic-results-as-new-stool-dna-test
