- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Low Hepatitis B Reactivation Risk in Patients Treated With Immune Checkpoint Inhibitors, Study Says
The researchers found that patients with cancer exposed to immune checkpoint inhibitors have a 1.3% risk of hepatitis B virus reactivation.
There is a low risk of hepatitis B virus reactivation (HBVr) in patients treated with immune checkpoint inhibitors (ICIs) for advanced cancer, according to a study published in Infectious Diseases of Poverty.
The researchers explained that with immunotherapy increasingly used to treat cancer, patient concerns over potential complications from HBVr after checkpoint blockade immunotherapy also increased. More ICI clinical trials allowed diverse patient populations to receive the treatment. On the other hand, the researchers noted that most trials excluded patients with HBV, resulting in a lack of efficacy and safety data.
Because of this, the researchers conducted a study to assess “the risk of HBVr in patients receiving ICIs for advanced cancer,” their primary outcome being the rate of HBVr in patients with preexisting HBV infection or chronic hepatitis B who received ICI treatment. To do so, the researchers retrieved relevant studies published before April 30, 2023, through a comprehensive search across multiple databases. The Newcastle-Ottawa Scale (NOS) was used to assess the quality of each study based on patient selection, comparability of groups, and assessment of outcome. The researchers noted that “studies with less than 6 stars were considered relatively low quality and were excluded.”
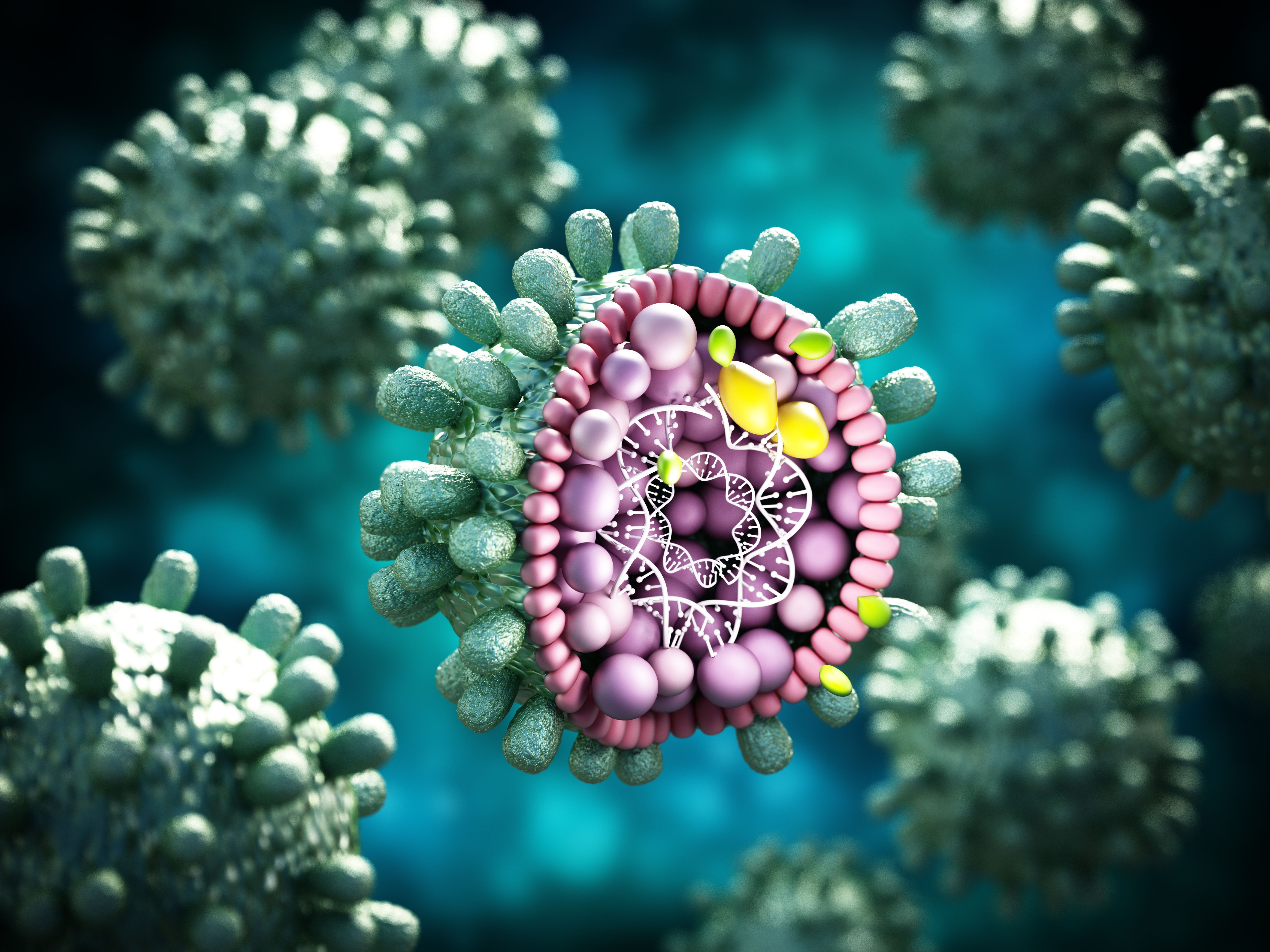
Hepatitis B Virus | Image credit: Destina - stock.adobe.com.
They first retrieved 12,384 articles, which the researchers narrowed down to 34 studies published between 2018 and 2023 that analyzed 7126 patients. Of these studies, 25 were conducted in Asia, 5 in the United States, 2 in Australia, 1 in New Zealand, and 1 in Italy. HBVr events transpired in 16 studies, with reactivation cases occurring in 123 patients. Consequently, the pooled HBVr rate was 1.3%, and the risk estimates varied from 0% to 30.0%, which indicated considerable heterogeneity among the included studies (95% CI, 0.2%-2.9%; I2 = 90.44%; P < .001).
“ICI therapy can be considered close to a low risk factor, according to the threshold recommended by the AGA [American Gastroenterological Association] guideline for the prevention and management of HBVr, which defines an expected incidence of [less than] 1% of cases as low risk,” the authors wrote.
The researchers also performed subgroup analyses to discover the heterogeneity sources and to examine how various factors affect HBVr risk in patients with cancer receiving ICIs. They first conducted a subgroup analysis comparing HBVr rates between patients with hepatocellular carcinoma (HCC) and patients without HCC. The researchers found that the reaction rates in those with HCC and those without HCC were 1.9% (95% CI, 0%-5.7%; I2 = 92.52%; P < .001) and 0.5% (95% CI, 0%-2.2%; I2 = 72.37%; P < .001), respectively.
Also, the researchers found that the reactivation rates of patients who were hepatitis B surface antigen (HBsAg)-seropositive vs those who were HBsAg-negative were 1.3% (95% CI, 0%-4.5%; I2 = 87.44%; P < .001) and 0% (95% CI, 0%-0%; I2 = 0; P = 0.796, respectively. This showed that patients with positive HBsAg status had a higher risk of HBVr than those with negative HBsAg status.
Lastly, they analyzed the studies based on their level of regional economic development as classified by the International Monetary Fund (IMF), comparing the HBVr rates of developing regions with those of developed regions. The meta-analysis of the 14 studies from developing regions showed a pooled HBVr rate of 2.9% (95% CI, 0.2%-7.5%; I2 = 91.85%; P < .001), and the reactivation rate in the 20 studies from developed countries was 0.2% (95% CI, 0%-1.0%; I2 = 72.91%; P < .001). The researchers learned that the reported reactivation rate varied greatly between regions.
They acknowledged their study’s limitations, one being that it did not cover all ICI or cancer types, meaning the findings may not be generalizable to all populations. Also, because most included studies were retrospective, they noted that it may have led to high levels of selection bias. Despite these limitations, the researchers explained that meta-analyses such as this are necessary given the severe situation surrounding hepatitis B prevention and control, as well as the urgent need for evidence-based information. Consequently, they called for further research to build upon their findings.
“Further research is needed to expand upon these findings and better understand the risks associated with ICI-based therapy for advanced cancer in patients with hepatitis B,” the authors concluded.
Reference
Xia Z, Zhang J, Chen W, et al. Hepatitis B reactivation in cancer patients receiving immune checkpoint inhibitors: a systematic review and meta-analysis. Infect Dis Poverty. 2023;12(1):87. doi:10.1186/s40249-023-01128-6
