- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Largest Study of Lp(a), Recurrent ASCVD Highlights Critical Risks and Need for Screening
Higher levels of lipoprotein(a) (Lp[a]) were found to be associated with a continuously increasing risk of recurrent atherosclerotic cardiovascular disease (ASCVD) events.
A new analysis of the Family Heart Database demonstrated a link between higher lipoprotein(a) (Lp[a]) levels and continuously increased risk of atherosclerotic cardiovascular disease (ASCVD).
Seth J. Baum, MD, presented new findings from the Family Heart Database | Image credit: Hayden Klein
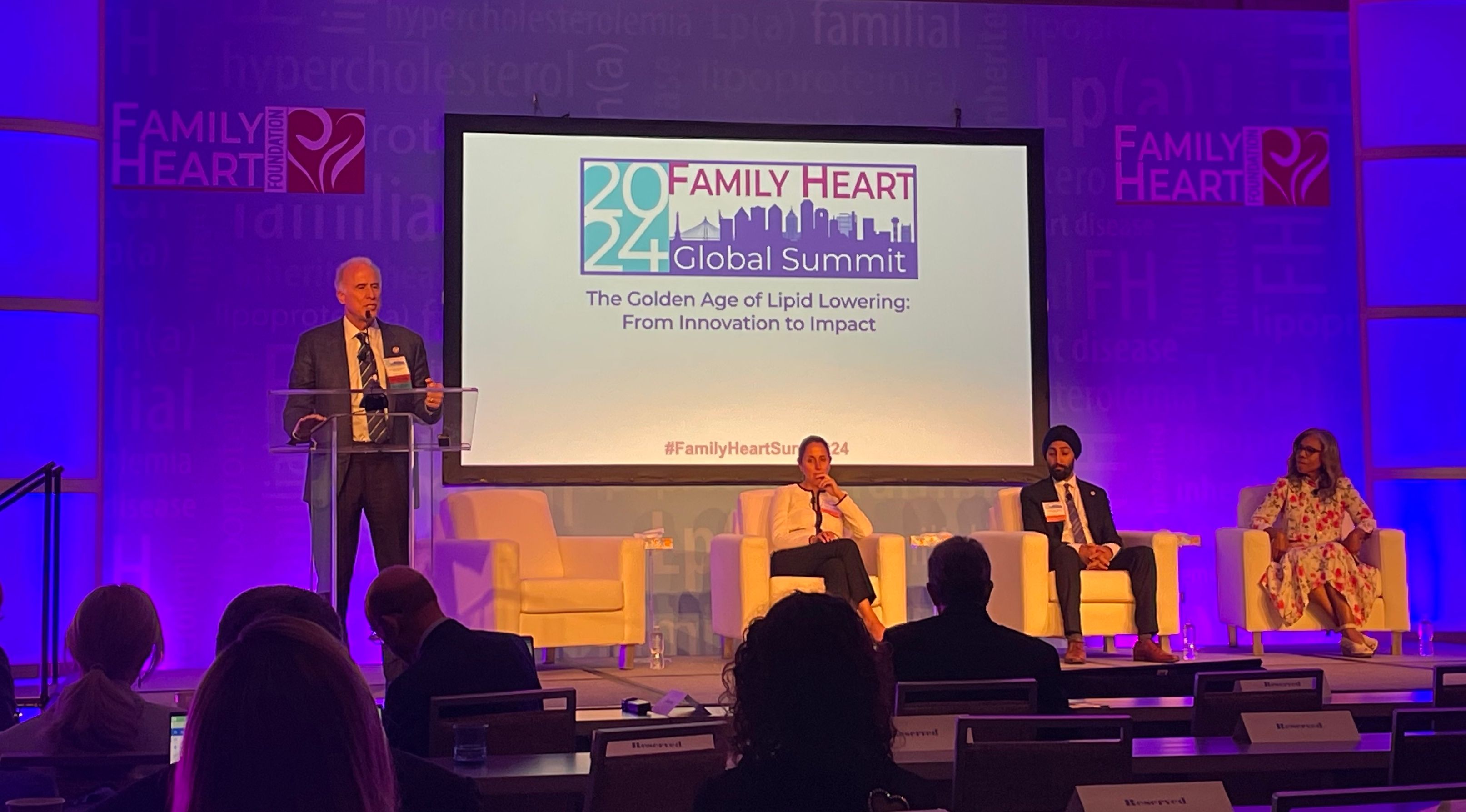
Seth J. Baum, MD, CMO of Flourish Research, vice chair and chair-elect of the Family Heart Foundation, presented these groundbreaking data—which are not yet published—at the 2024 Family Heart Global Summit.
“These results highlight the need to screen for Lp(a) and also consider the magnitude of the Lp(a) elevation in assessing the risk of recurrent ASCVD events,” he said. “Also, an unmet need for safe and effective Lp(a)-lowering treatments.”
The Family Heart Database includes medical claims and lab data of 340 million unique individuals. This particular retrospective cohort study included nearly 274,000 of these individuals with established ASCVD between 2012 and 2022, making it “8 times as large as the next largest study” on the topic, according to Baum.
All patients were adults who had at least 1 Lp(a) test on file and at least 1 medical claim submitted at least 30 days after initial ASCVD diagnosis. Of this cohort, 43% were women and 57% were men, with 8% of patients being Black, 9% being Hispanic, and 57% being White.
Baseline ASCVD events included myocardial infarction (MI), acute ischemic heart disease, percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG), unstable or stable angina, stroke, other cerebral vascular disease, peripheral vascular disease, and general ASCVD. Recurrent ASCVD events included MI hospitalization, other acute coronary syndromes, ischemic stroke, PCI, and CABG, and the primary end point was time to event.
The study broke down the data into 5 Lp(a) categories.
- Less than 15 mg/dL
- 15 to 79 mg/dL
- 80 to 179 mg/dL
- 180 to 299 mg/dL
- 300 or more mg/dL
Across these ascending categories, the results showed a continuous increase in the risk of recurrent ASCVD events, particularly in individuals with higher Lp(a) levels, who saw a 43% higher risk of recurrent ASCVD events compared with those in the lowest category after adjusting for all covariates (HR, 1.43; 95% CI, 1.38-1.49).
Baum also highlighted the need to “redefine normalcy” in cholesterol levels, as individuals with Lp(a) levels between 15 and 79 mg/dL—long thought to be relatively safe—showed a statistically significant increase in cardiovascular risk.
“I harken back to where we were when I started medical school in 1981, where a cholesterol level of 300 mg/dL was considered normal,” Baum concluded. “If we look at the data we saw today…there’s a statistically significant increase in risk.”
In closing, Baum reiterated the importance of widespread Lp(a) screening, especially for individuals with a history of ASCVD. As research continues to clarify the role of Lp(a) in heart disease, Baum emphasized that future guidelines must reflect this growing body of evidence. He also highlighted the need for accessible treatments tailored to individuals with elevated Lp(a) levels, noting that these patients are at a particularly high risk of recurrent events.
Reference
Baum SJ. The link between lipoprotein(a) levels and recurrent ASCVD events: an analysis of the Family Heart Database. Presented at: Family Heart Global Summit; September 23, 2024; Dallas, TX. https://familyheart.org/2024-family-heart-global-summit/agenda
What It Takes to Improve Guideline-Based Heart Failure Care With Ty J. Gluckman, MD
August 5th 2025Explore innovative strategies to enhance heart failure treatment through guideline-directed medical therapy, remote monitoring, and artificial intelligence–driven solutions for better patient outcomes.
Listen
From Polypharmacy to Personalized Care: Dr Nihar Desai Discusses Holistic Cardiovascular Care
May 30th 2024In this episode of Managed Care Cast, Nihar Desai, MD, MPH, cardiologist and vice chief of Cardiology at the Yale School of Medicine, discusses therapies for cardiovascular conditions as they relate to patient adherence, polypharmacy, and health access.
Listen
