- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Keratoconus Associated With ADHD in Male Patients
Male adolescent and young adult patients were found to have an increased risk of keratoconus if they had attention-deficit/hyperactivity disorder (ADHD), regardless of confounders.
Male patients who had attention-deficit/hyperactivity disorder (ADHD) had a higher rate of keratoconus compared with other patients. These results could help with educating younger patients on eye care, according to JAMA Ophthalmology.
Keratoconus consists of corneal thinning and steepening from a bilateral corneal ectasia, or when the cornea thins and bulges outward. The general population has a prevalence of 50 to 230 cases per 100,000 individuals. Irritation of the corneal surface has been linked to keratoconus, including eye-rubbing. Patients who have cognitive and psychiatric conditions that cause eye rubbing have not been evaluated for the relationship to keratoconus. This study aimed to evaluate the association between keratoconus and other psychological disorders, such as anxiety, intellectual disabilities, and obsessive compulsive disorder (OCD).
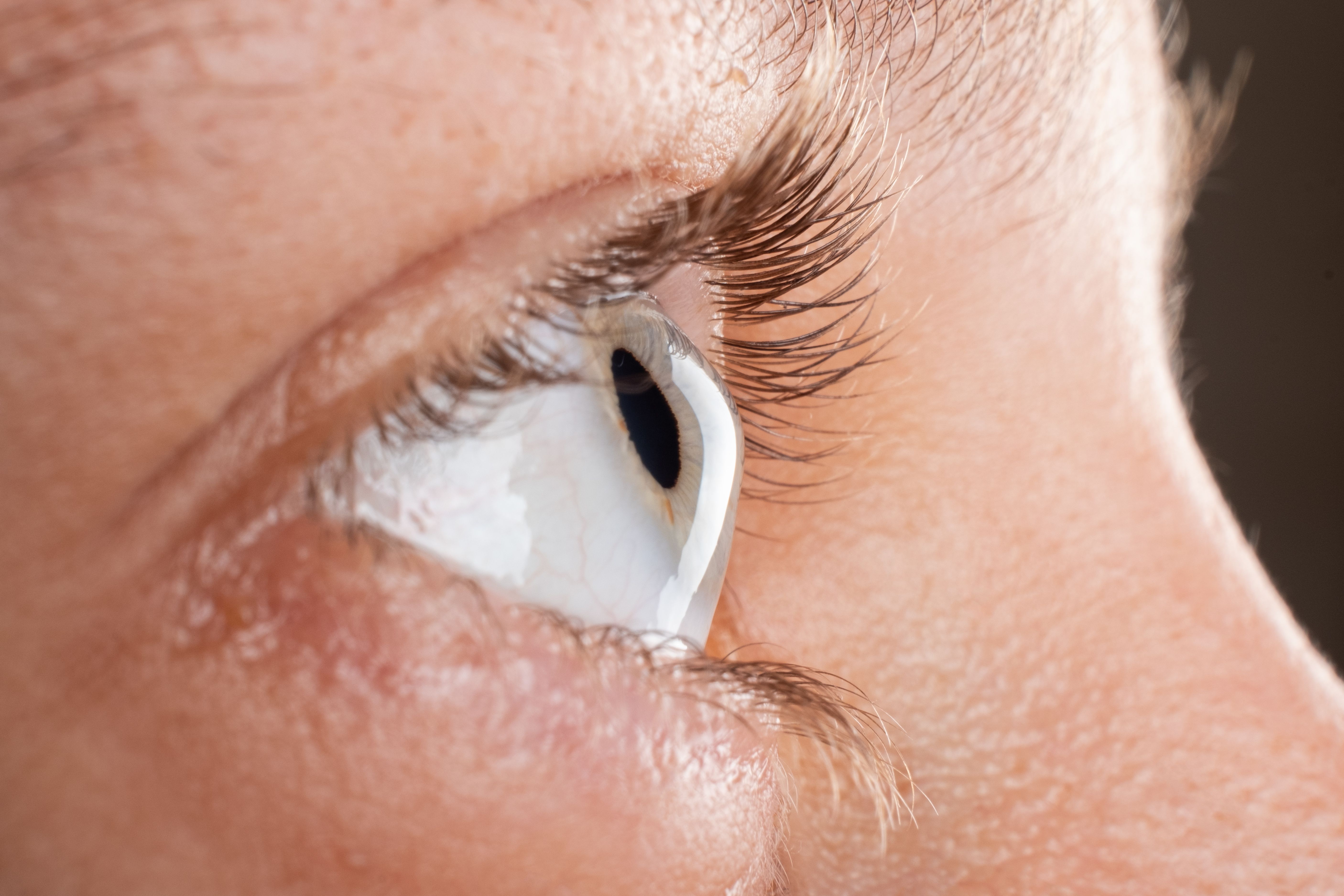
Female eye diagnosed with keratoconus corneal thinning | Image credit: Fukume - stock.adobe.com
The researchers conducted a retrospective cross-sectional study. All patients included were from Israel, where medical evaluation and fitness for service occurs for individuals aged 16 to 18 years. Each applicant and their physician report visual acuity and refractive status from their ophthalmologist, and patients with astigmatism of 2.00 diopters and higher have corneal topography performed. All candidates for the military also under an intelligence test. A psychiatrist makes certified diagnoses for patients which informed the fitness-for-services (FFS) psychiatric codes given.
For this study, corneal topography, medical history, best spectacle-corrected visual acuity, contact lens dependence, graft failure or rejection, and history of corneal transplant were used. Keratoconus cases were split into 2 groups: mild keratoconus, where visual acuity was 6/6 to 6/15 when using spectacles, and moderate to severe keratoconus, when visual acuity was worse than 6/15 even after correction with spectacles. Individuals who were examined for the Israeli military between January 2011 and December 2021 were eligible. Patients were excluded if they had incomplete FFS information or had medical conditions that could affect cognitive function.
There were 940,763 patient files reviewed. The patients had a mean (SD) age of 17.56 (1.47) years, 40.7% were female patients, and 0.16% had keratoconus. More male patients had keratoconus compared with female patients (72.8% vs 59.2%) and an overall higher risk of keratoconus compared with females (OR, 1.93; 95% CI, 1.72-2.16).
There were 107,249 patients who reported a psychiatric comorbidity, of which 0.5% had anxiety, 0.1% had OCD, 0.1% had autism, and 10.6% had ADHD. Keratoconus was more prevalent in patients with ADHD compared with patients without (15.9% vs 10.7%). ADHD was also more likely to be diagnosed in patients with keratoconus compared with those without (OR, 1.58; 95% CI, 1.38-1.81), with the OR being 1.62 (95% CI, 1.41-1.86) when adjusting for age, sex, and weight. Associations between anxiety, OCD, and autism with keratoconus was not found.
Men with ADHD were more likely to have keratoconus compared with men without (OR, 1.62; 95% CI, 1.39-1.90); keratoconus did not have a significant association with females with ADHD. A binary logistic regression analysis found that keratoconus and ADHD had an association in both men and men (OR, 1.54; 95% CI, 1.34-1.77).
There were some limitations to the generalizability of these study findings. Data were limited for disease severity due to the retrospective study design and the FFS coding system. There also was no way to establish a causal relationship between ADHD and keratoconus, becase there were no data on which disease was diagnosed first. Eye rubbing was also not documented in any patients.
The researchers concluded that there was an association between ADHD and keratoconus in adolescents and young adults. This association persisted despite adjustments. Future studies, they recommend, should focus on cause and effect between ADHD and keratoconus.
Reference
Safir M, Hecht I, Heller D, Pras E, Lifshitz M, Einan-Lifshitz A. Psychiatric comorbidities associated with keratoconus. JAMA Ophthalmol. Published online November 9, 2023. doi:10.1001/jamaophthalmol.2023.5176
