- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Kaiser Survey Data Offer More Reasons to Rethink Health Risk Assessments
While incentives and penalties are effective at getting people to complete health risk assessments, the assessments do not lower costs or increase wellness.
Will Rogers once said, “The income tax has made more liars out of the American people than golf has.” Health risk assessments (HRAs), and the umbrella of wellness, could give taxes a run for their money. The intrusive and often ineffective HRA questions tend to ask about how you rate your diet, your marriage, how often you drink, and whether you’re self-aware enough to know that seatbelts should be buckled. They often come with incentives or penalties to push employees into completing them. It’s no wonder wellness has a Net Promoter Score of —52.
It’s Not All Bad, Is It?
Interestingly, wellness' popularity with employers, brokers, and consultants seems unshakeable. The 2017 Kaiser Family Foundation Employer Health Benefits survey data reveal that in 2016, HRAs were offered by over 78% of firms with at least 1000 employees. A full two-thirds of those firms offered an incentive (carrot) or penalty (stick), to participate in wellness. Even so, wellness has an increasingly hard time showing savings. The University of Illinois Wellness study, which is the gold standard as the only randomized controlled trial on wellness that I’m aware of, showed no savings for the year after it was implemented. People didn’t go to the gym more, and they didn’t spend less on healthcare.
Business and Courts
Even so, wellness and its sexier sibling well-being, are increasingly mentioned in business, healthcare, and the courts. Jamie Dimon, CEO, JPMorgan Chase, in his 2018 letter to JPMorgan Chase shareholders, mentions wellness, particularly obesity and smoking, as 1 of the first 6 issues to address as part of the Berkshire—Amazon–JPMorgan Chase healthcare joint venture. Towers Watson’s 2017 high-performance insights employer survey mentions well-being 77 times—an 88% increase compared to the 2015 survey. The case of AARP v the Equal Employment Opportunity Commission highlights the debate of what is considered voluntary wellness, with current fines of 4 figures having serious implications on wellness programs and the use of wellness incentives going forward.
Kaiser Study Data
The Kaiser study adds another voice and is based on a deeper dive into the actual survey data. Sometimes 200-plus pages of survey results are not enough to get a grasp on things. What the data show is that wellness carrots or sticks are effective in 3 ways:
- Getting people to fill out HRAs
- Helping companies spend money on incentives or penalties for employees (reducing morale)
- Improving a company’s own perception of wellness’s effectiveness.
But when you look at premiums, there is no sense that those that offer HRAs show a reduction in premiums for health plans even when controlled for other factors.
The below grid is a summary of HRA completion and premiums. The first row shows the 164 large companies that offer no HRA; the next rows show the quartiles based on the percentage of employees within the companies that completed a HRA, the lowest tier having 0% to 20% completion, and the highest with 70% to 100% completion.
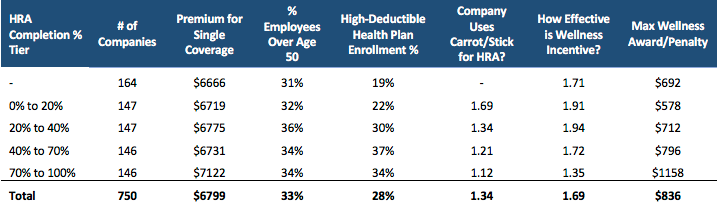
The grid reflects the unweighted averages of the following: the annual yearly premiums for single coverage, a demographic field (percent of employees over 50), and a broad estimate of companies plan benefit values (high-deductible health plan enrollments as a percent of total enrollments). The field “Company Uses Carrot/Stick for HRA” is listed as either a 1 or 2, with 1 indicating that a company uses either an incentive or penalty to encourage HRA completion. The next column is the average measure of the perception of the effectiveness of the wellness incentives offered: 1 = very effective, 2 = somewhat effective, and 3 = not at all effective. The last column is the average of the maximum total wellness reward or penalty for all wellness and health program promotions.
Groups in the Highest Quartile of HRA Completion
As stated, wellness carrots and sticks are effective at getting people to complete HRAs and are associated with a 26% average increase in completion rates (P<.0001). That’s where it ends. The highest quartile group of 70% to 100% completion shows that there are no consistencies in premiums, demographics, or other driving factors and HRA completion doing anything other than costing money through program costs, rewards, and damages to morale through penalties. This group also spends more than $400 more per year than the companies that don’t use HRAs.
The management guru Peter Drucker famously stated: “There is nothing so useless as doing efficiently that which should not be done at all.” Businesses need to wake up and lead with a new approach on employee wellness, healthcare education, and its personal and financial implications. Companies could take wellness dollars and direct them to other things: simpler healthcare education programs, richer plan designs, increased health savings contributions, sports equipment reimbursement programs (people love the idea of getting money for skates or skis), or fancier greens in the cafeteria. That is how you promote a culture of wellness without spending money foolishly, penalizing employees, or encouraging them to lie.
