- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Increases in Cancer Screenings, Chronic Condition Diagnoses in First Year of Medicare Coverage
Patients were twice as likely to get a colorectal cancer screening and 50% more likely to get a breast cancer screening in their first year of Medicare coverage.
Once a patient moves onto Medicare coverage, they are twice as likely to get a colorectal cancer screening and 50% more likely to get a breast cancer screening, as well as more likely to be newly diagnosed for a variety of conditions, according to a report published by Epic Research.
“Some previous studies have suggested that cancer screening and subsequent care is more likely at age 65, which researchers posit is due to increased insurance coverage with Medicare eligibility,” the researchers explained.
They analyzed the impact of having Medicare insurance coverage on cancer screening and diagnosis rates, as well as diagnosis rates for chronic diseases.
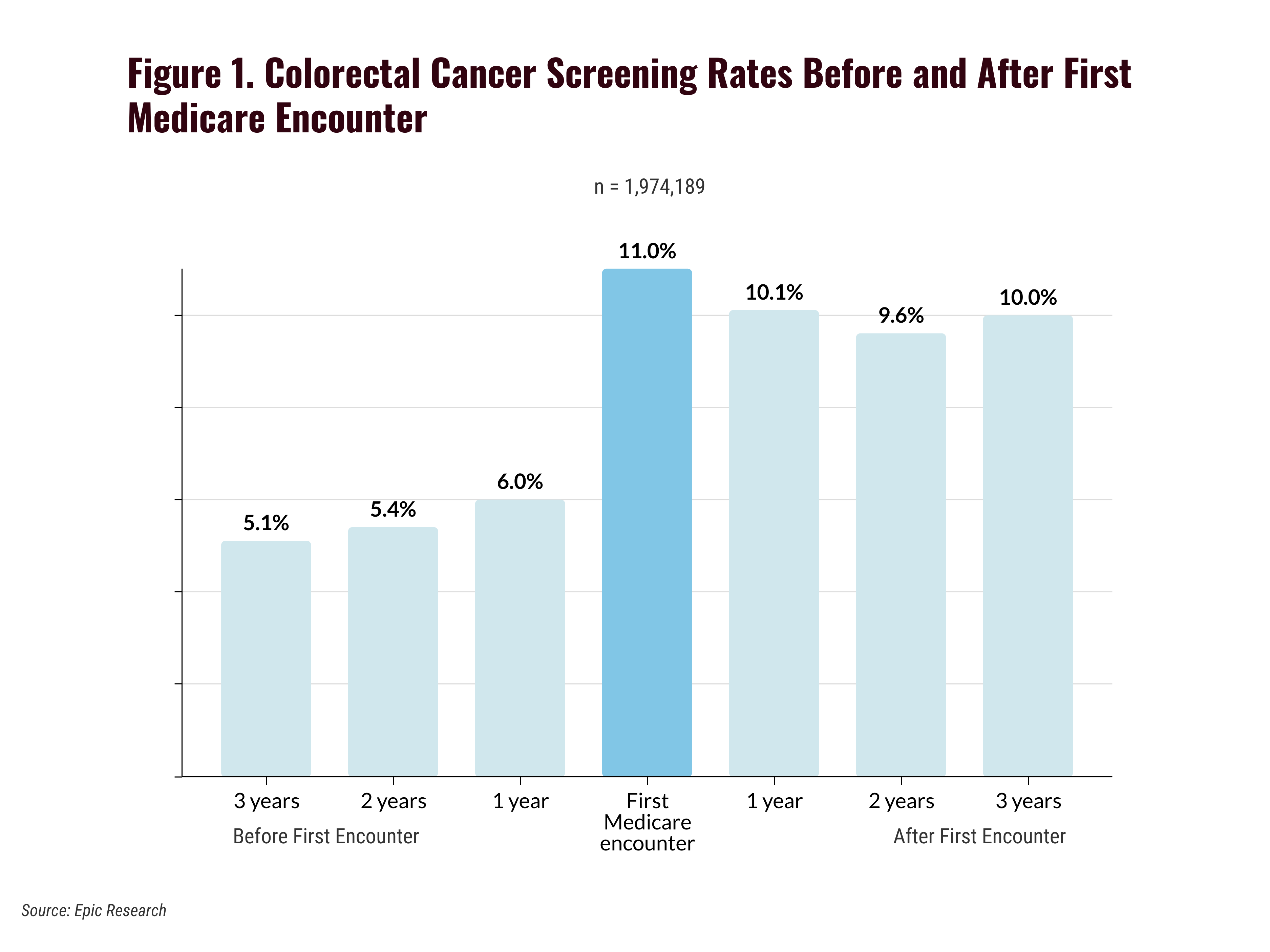
In order to do so, they looked at screening rates during the year a patient had their first Medicare encounter. Colorectal cancer screening increased from 6.0% in the year prior to a patient’s first Medicare encounter to 11.0% during the year of their first Medicare encounter (Figure 1).
For colorectal cancer screenings, rates dropped slightly after the first year, hovering around 10% for the next 4 years.
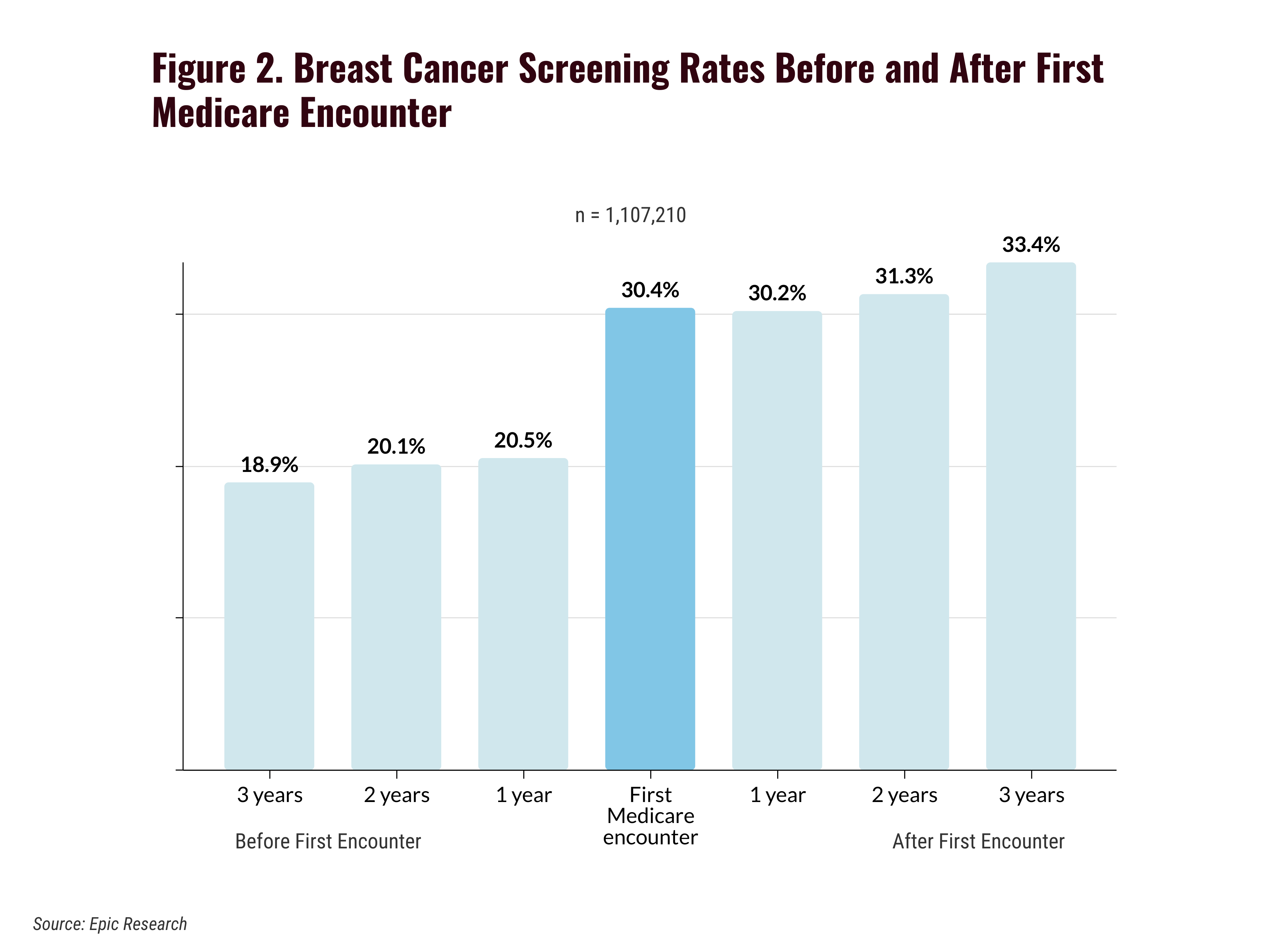
In comparison, breast cancer screenings continued to increase after Medicare coverage (Figure 2). Screening rates increased 50.0% from 20.5% in the year prior to a patient’s first Medicare encounter to 30.4% during the first year of a Medicare encounter. By 3 years after the first Medicare encounter, breast cancer screenings had increased further to 33.4% before dipping slightly to 33.2% 4 years after the first encounter.
They also evaluated more than 20 million patients between 60 and 70 years to understand the impact Medicare coverage had on new diagnoses, looking specifically at 14 common conditions. The analysis found that 10 conditions—breast cancer, colorectal cancer, prostate cancer, lung cancer, hypertension, hyperlipidemia, coronary heart disease, type 2 diabetes, depression, and chronic obstructive pulmonary disease—were more commonly initially diagnosed in the year a patient had their first Medicare encounter compared with the 5 years before and after.
The hypertension diagnosis rate had a particularly large jump in the first year of Medicare coverage from 8.1% in the year prior to 17.3% in the first year. After that first year of coverage, the diagnosis rate dropped back down to 8.0% in the year after. The hyperlipidemia diagnosis also had a relatively large jump from 14.3% in the year prior to the first year of Medicare coverage to 18.3% in the first year, before dropping back down to 12.5% the next year.
Dementia, heart failure, chronic kidney disease, and arthritis all had their highest initial diagnosis 5 years prior to starting Medicare. In the years after, all of these were on a downward trajectory of diagnosis.
The reason these may be diagnosed prior to Medicare coverage is because “these diseases are more likely to have noticeable symptoms that might prompt a patient to seek medical care,” the authors explained.
The researchers noted that the reason why many chronic conditions are diagnosed in the first year of Medicare coverage, with rates decreasing in subsequent years is because many of these conditions that are commonly diagnosed in the first year of coverage have associated quality measures that CMS has reporting requirements on.
“Lung, breast, prostate, and colorectal cancer were all more likely to be diagnosed in the first year of Medicare coverage,” they added. “This aligns with previous studies showing a ‘Medicare effect’ on the timing of cancer diagnoses.”
Reference
Barelt K, Haddock J, Piff A, et al. The ‘Medicare Effect’: Screening and diagnosis rates increase in the first year of Medicare coverage. Epic Research. July 26, 2023. Updated August 4, 2023. Accessed August 10, 2023. https://epicresearch.org/articles/the-medicare-effect-screening-and-diagnosis-rates-increase-in-the-first-year-of-medicare-coverage
Subjective and Objective Impacts of Ambulatory AI Scribes
January 8th 2026Although the vast majority of physicians using an artificial intelligence (AI) scribe perceived a reduction in documentation time, those with the most actual time savings had higher relative baseline levels of documentation time.
Read More
Telehealth Intervention by Pharmacists Collaboratively Enhances Hypertension Management and Outcomes
January 7th 2026Patient interaction and enhanced support with clinical pharmacists significantly improved pass rates for a measure of controlling blood pressure compared with usual care.
Read More
