- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: In April 2021, Telehealth Utilization Falls Nationally for Third Straight Month
Robin Gelburd, JD, details the dip in telehealth claims observed during April 2021.
In April 2021, telehealth utilization fell nationally for the third straight month, according to FAIR Health’s Monthly Telehealth Regional Tracker. Telehealth claim lines declined 12.5 percent nationally as a percentage of medical claim lines, decreasing from 5.6 percent of claim lines in March 2021 to 4.9 percent in April (Exhibit 1). This was a greater decrease than the drop of 5.1 percent in March but not as great as the decrease of 15.7 percent in February. Telehealth usage also declined in April in all four US census regions, with the greatest decline in the South, where the decrease was 12.2 percent. The data represent the privately insured population, excluding Medicare and Medicaid.
Exhibit 1. Monthly Telehealth Regional Tracker, March versus April 2021, United States
Click to enlarge. (Source: FAIR Health)
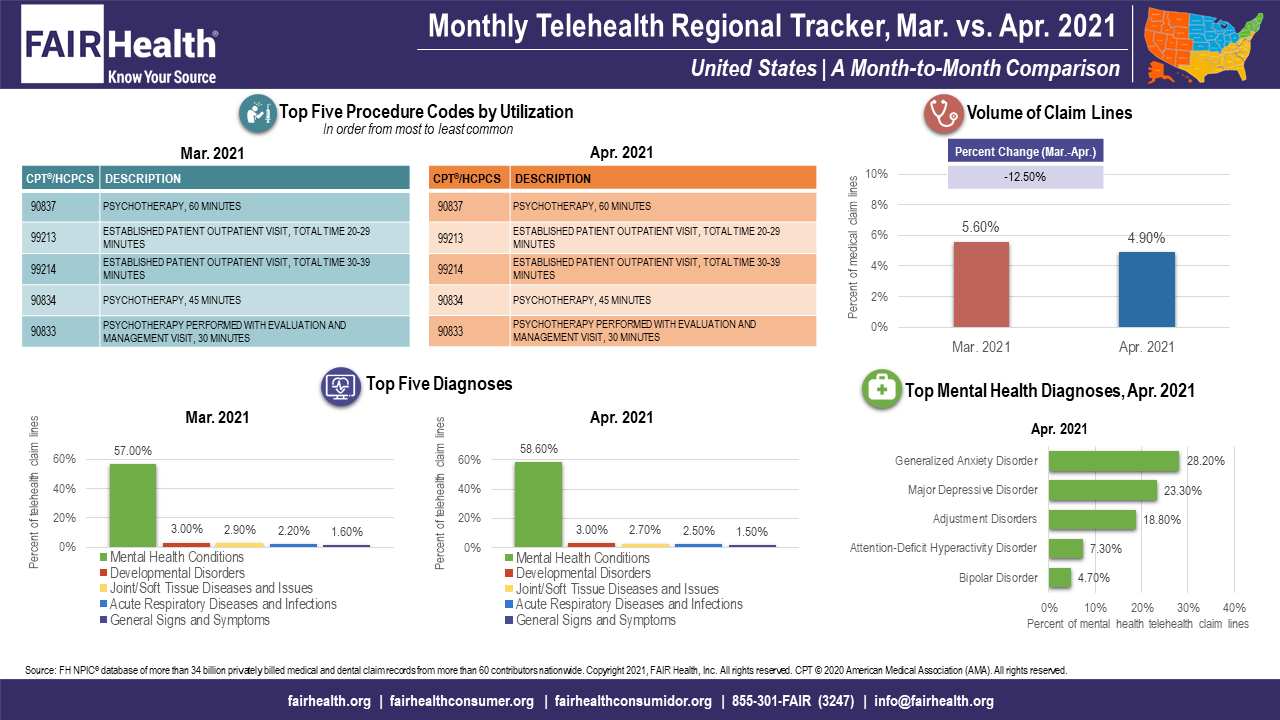
The decline in telehealth utilization appears largely to be driven by the return of non-mental-health services from telehealth—where they had shifted during the COVID-19 pandemic—to in-person settings. The percentage of telehealth claim lines associated with mental health conditions, the number one telehealth diagnosis, continued to rise nationally and in every region. Nationally, for example, mental health conditions increased from 57 percent of telehealth claim lines in March 2021 to 58.6 percent in April. Likewise in April, psychotherapeutic/psychiatric codes increased nationally as a percentage of telehealth procedure codes, whereas evaluation and management (E&M) codes decreased. Within the category of mental health conditions, there were no changes in the rankings of top mental health diagnoses nationally or regionally.
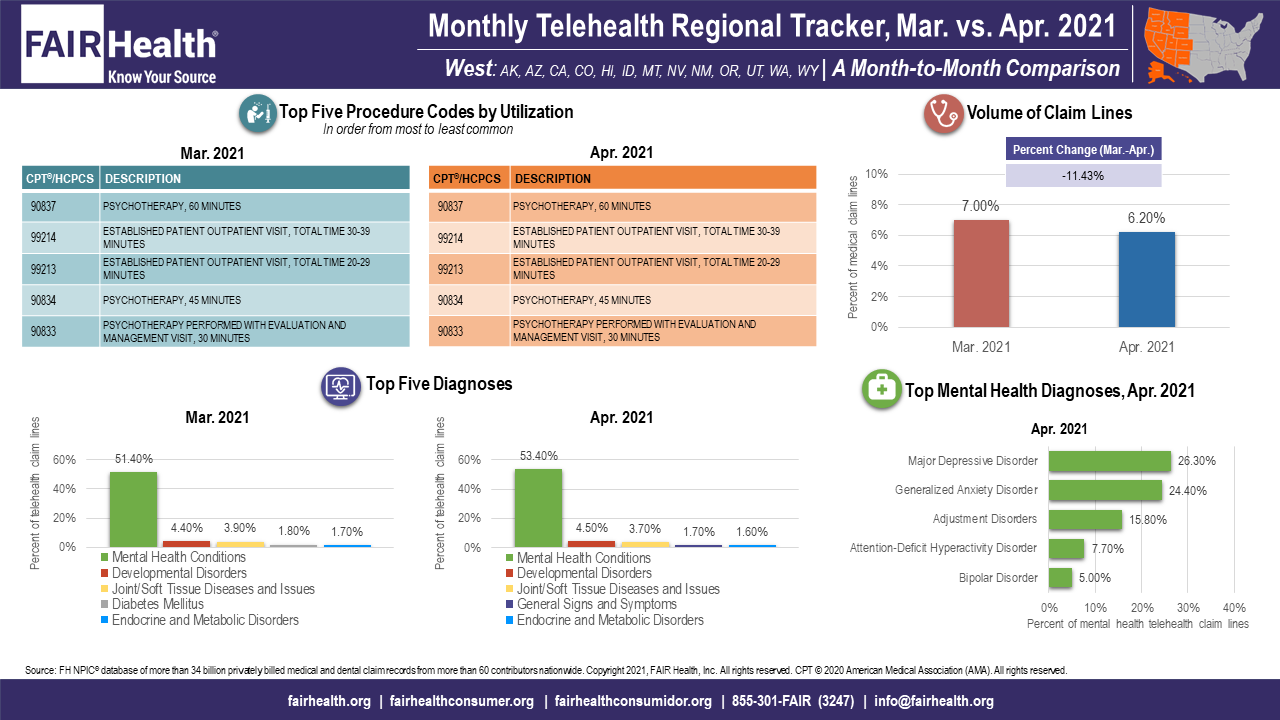
In April, acute respiratory diseases and infections increased as a percentage of telehealth claim lines nationally and in the Midwest and South. As the COVID-19 pandemic wanes, this suggests a return to non-COVID respiratory conditions, such as colds and bronchitis. Also in April, general signs and symptoms joined the top five telehealth diagnoses in the West, again suggesting a return to more “ordinary,” non-COVID conditions such as colds and stomach viruses (Exhibit 2).
Click to enlarge. (Source: FAIR Health)
About the Monthly Telehealth Regional Tracker
Launched in May 2020 as a free service, the Monthly Telehealth Regional Tracker uses FAIR Health data to track how telehealth is evolving from month to month. An interactive map of the four US census regions allows the user to view an infographic on telehealth in a specific month in the nation as a whole or in individual regions. Each infographic shows month-to-month changes in volume of telehealth claim lines, top five telehealth procedure codes, top five telehealth diagnoses (or diagnostic categories) and top five granular diagnoses within the most common diagnostic category.
FAIR Health’s Monthly Telehealth Regional Tracker continues to reveal changes in the evolution of telehealth as the COVID-19 pandemic recedes. This is one of many ways we pursue our healthcare transparency mission.
For the Monthly Telehealth Regional Tracker, click here.
Author Information
Robin Gelburd, JD, is the President of FAIR Health, a national, independent nonprofit organization with the mission of bringing transparency to healthcare costs and health insurance information. FAIR Health possesses the nation’s largest collection of private healthcare claims data, which includes over 34 billion claim records and is growing at a rate of over 2 billion claim records a year. Certified by the Centers for Medicare & Medicaid Services (CMS) as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D; FAIR Health includes among the private claims data in its database, data on Medicare Advantage enrollees. Gelburd is a nationally recognized expert on healthcare policy, data and transparency.
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
