- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
IFGBP-2 Levels Indicative of Renal Prognosis in Pediatric Lupus Nephritis, Study Finds
In a cross-sectional study, insulin growth factor binding protein 2 (IFGBP-2) showed promise as a prognosis biomarker for renal disease in pediatric lupus nephritis (LN).
Serum insulin growth factor binding protein 2 (IGFBP-2) has demonstrated significant potential as a biomarker for gauging and predicting renal pathology in pediatric lupus nephritis (LN), according to a recent study published in Pediatric International.
Renal disease affects children with childhood-onset systemic lupus erythematosus (cSLE) at rates of over 50%. Additionally, individuals impacted by cSLE or SLE are often develop LN—which is one of the larger contributors to morbidity and mortality in this population.
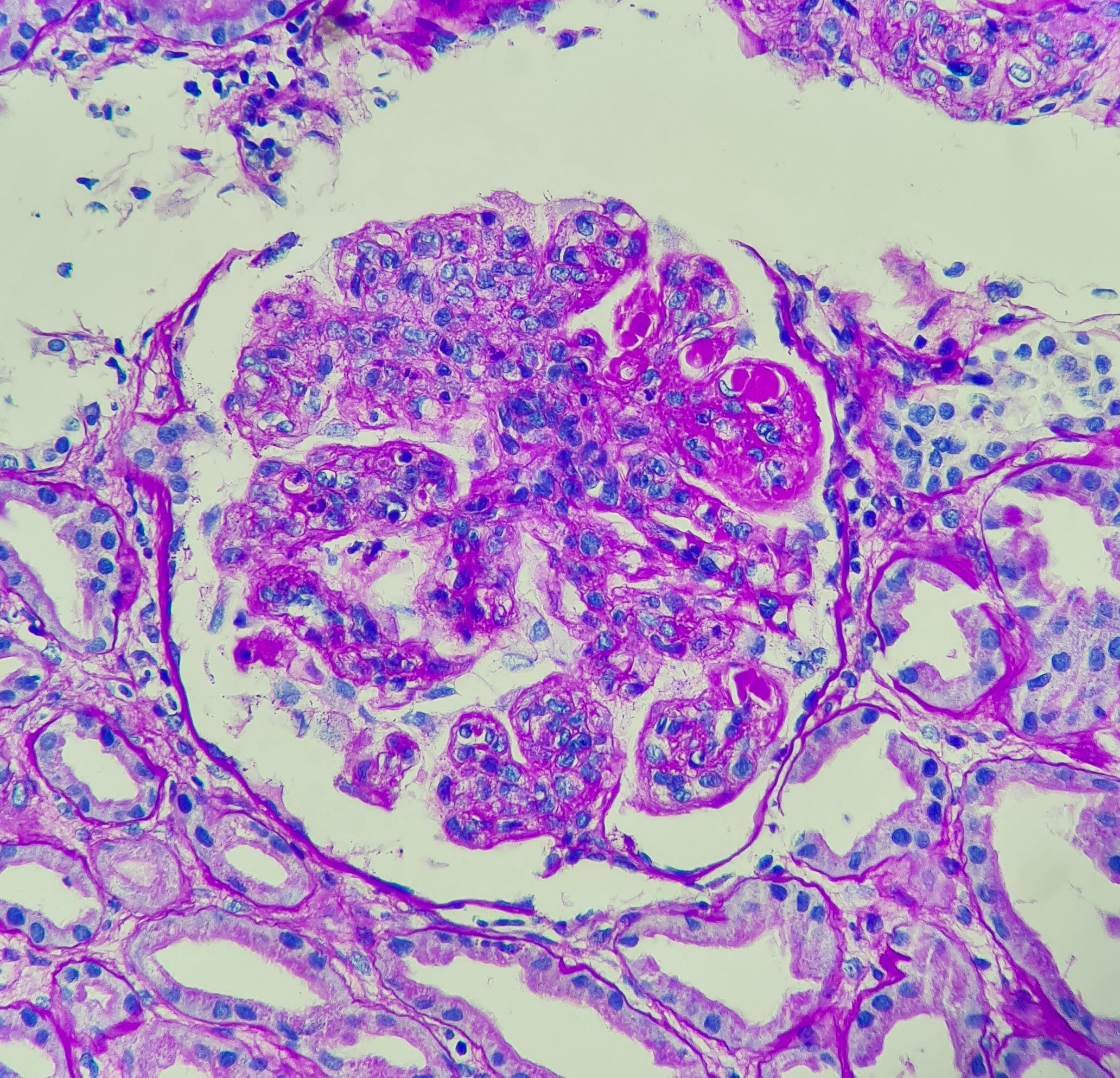
Lupus Nephritis | Chutima - stock.adobe.com
The ability to diagnose LN in earlier stages is an important step for managing the care and treatment of these patients. Multiple biomarkers have been verified to indicate patients’ disease activity; however, there is still a need to identify biomarkers that accurately depict renal activity, predict pathology, and potential flare-ups. The current lab tests and kidney biopsies that these assessments rely upon produce insufficient results and are quite invasive, prompting the search for better, non-invasive alternatives, according to the study authors.
Studying insulin growth factor binding proteins (IGFBPs) can provide much-needed insights on this issue due to the role they play in immune responses. IFG1, for example, is connected to B-cell activation, which is a distinctive feature of SLE. Recent studies, as the authors mention, have prioritized IGFBPs in the search for diagnostic biomarkers for lupus. Specifically related to SLE, the authors cited a study that discovered the presence of IFGBP-2 in an array-based proteomic screening related to lupus.
To expand upon this finding and address the need for early LN detection, researchers conducted a cross-sectional study to evaluate whether IGFBP-2 can be considered a non-invasive biomarker for renal and disease pathology in pediatric LN.
Between September 2019 and September 2021, children who presented with LN were identified from the Nephrology and Dialysis Department in the Vietnam National Children’s Hospital. In total, 93 children were recruited, all of whom had renal biopsies to determine LN. This LN group was then age- and gender-matched with 35 SLE patients who were not displaying kidney damage (disease controls) and 30 healthy controls (HC).
The systemic lupus erythematosus disease activity index (SLEDAI) was used to measure SLE activity (with higher scores indicating more serious disease states). Patient labs collected data on blood count, various immunobiological tests, C3 and C4 levels, urine analysis and protein-creatinine rates, and estimated glomerular filtration rate (eGFR). Serum double-stranded DNA (dsDNA) was also collected from every child in the SLE group. Furthermore, an enzyme-linked immunosorbent assay was used to measure serum IGFBP-2, and LN activity was classified according to criteria given by the International Society of Nephrology and the Renal Pathology Society: class I (minimal mesangial,) II (mesangial proliferative), III (focal), IV (diffuse), V (membranous), and VI (advanced sclerosing).
Patients had a median age of just over 11 years and were over 80% female. This trend was true across all groups. Proliferative forms of LN were the most prevalent with over 46% of children classified as class IV and over 35% as class III. The authors found that the vast majority of SLEDAI scores indicated high (score of 11-20) or very high (score > 20) disease activity.
Serum IGFBP-2 levels were significantly higher in the LN group (841.29 ng/mL) compared with the SLE disease controls (244.88 ng/mL, P < .001) and HC (172.69 ng/mL, P < .0001). There were no significant differences found between the classes of LN individuals.
A receiver operating curve analysis showed that IFGBP-2 levels more accurately differentiated between LN and SLE individuals than anti-dsDNA, which is a commonly used lab test. Specifically, the area under curve (AUC) value was 0.895 for IFGBP-2 levels, while anti-dsDNA had an AUC of 0.643.
Although IFGBP-2 did not significantly correlate with renal disease chronicity (P = .215), it did significantly correlate with the disease activity index (P = .007).
The researchers’ findings demonstrate the value and efficacy of using serum IFGBP-2 as a biomarker for assessing renal disease and pathology in pediatric LN. They concluded by indicating that their results will continue to be reported on in future studies.
Reference
Luong PT, Nguyen TTD, Nguyen NT, et al. Insulin-like growth factor binding protein-2 as a biomarker for lupus nephritis. Pediatr Int. Published August 25, 2023;65(1). doi: 10.1111/ped.15613
Telehealth Intervention by Pharmacists Collaboratively Enhances Hypertension Management and Outcomes
January 7th 2026Patient interaction and enhanced support with clinical pharmacists significantly improved pass rates for a measure of controlling blood pressure compared with usual care.
Read More
