- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Hospitalization, ER, and Medication Discontinuation Rates Still High in PNH
A retrospective analysis surveys the treatment landscape and patterns of patients with paroxysmal nocturnal hemoglobinuria (PNH), illuminating high hospitalization rates and emergency department use despite the availability of multiple treatment options.
Although multiple new treatments have become available in paroxysmal nocturnal hemoglobinuria (PNH), many patients do not receive PNH-specific medication, discontinue their therapy, and still experience emergency department visits or inpatient stays, according to a recent study published in Clinical and Applied Thrombosis/Hemostasis.
Hemolysis Model | image credit: tang90246 - stock.adobe.com
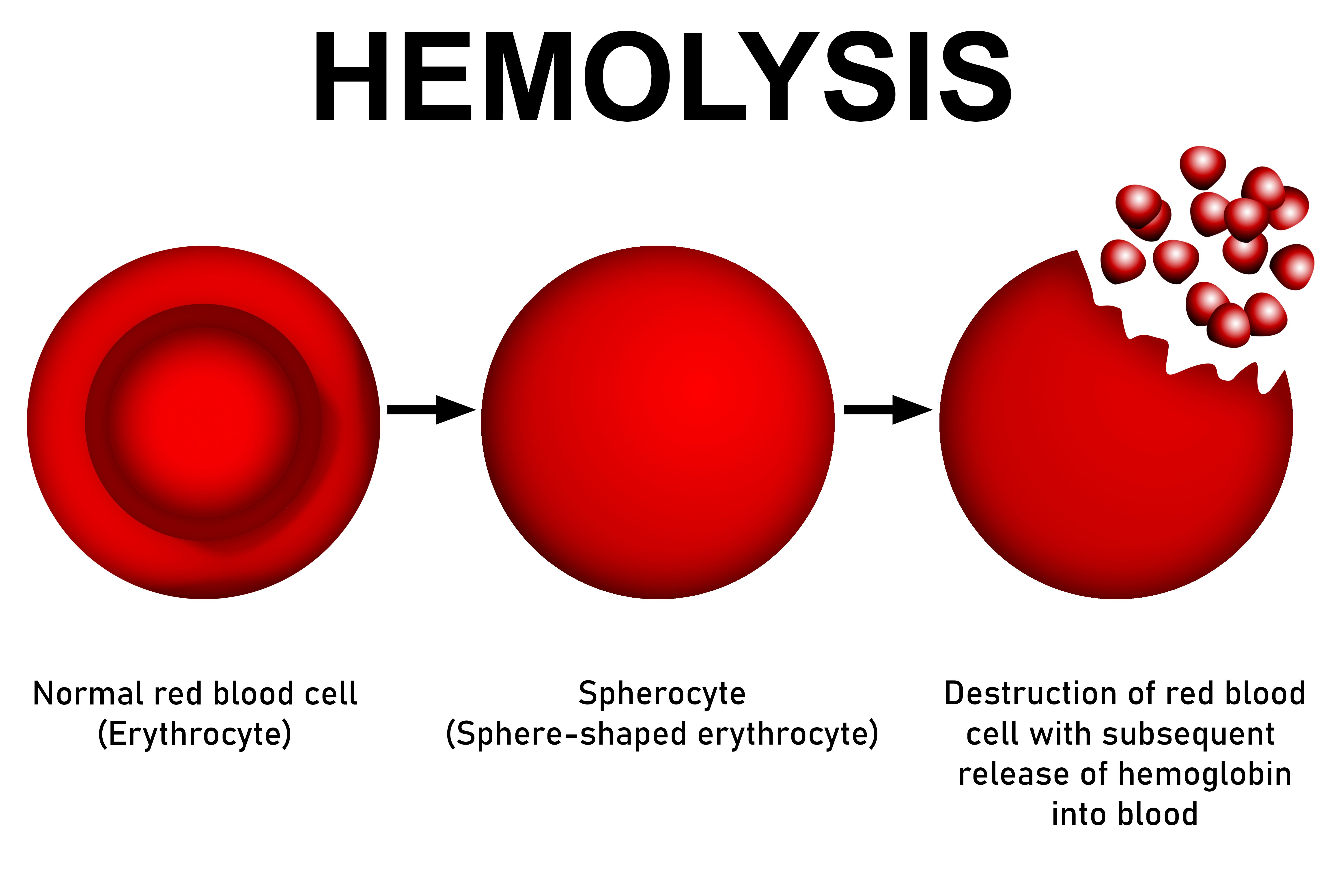
In patients with PNH, blood cells are more vulnerable to hemolysis. This defect stems from a somatic mutation of the PIGA gene and dysfunctional stem cells that cannot create glycosyl phosphatidylinositol (GPI) anchors to attach complement regulatory proteins to a cell’s membrane. In turn, those cells are destroyed by the complement system. There are a myriad of symptoms affected patients can experience including headaches, dysphagia, fatigue, and sexual dysfunction, as well as more severe complications like chronic kidney disease or thromboses.
Patients with PNH experience high degrees of financial burden. For those who are more reliant on transfusions, annual medical costs can soar above $100,000 a year. Various treatment methods are available to patients such as eculizumab (an intravenous complement inhibitor), ravulizumab (another intravenous complement inhibitor), pegcetacoplan (a subcutaneous complement inhibitor), as well as anticoagulants, growth factors, blood transfusions, and immunosuppressants.
Due to the limited literary evidence exploring drug and treatment patterns in PNH, researchers conducted an analysis on real-world data that investigated these patterns as well as the associated costs for patients newly diagnosed with PNH.
Between October 2015 and July 2021, data were gathered from the MarketScan database, which included pharmacy and medical claims data, and this information was bolstered with data from the US Optum research administrative claims database. Adherence to medication was measured through proportion of days covered (PDC) and medication possession ratio (MPR).
Results from the MarketScan data identified 272 eligible patients with a PNH diagnosis. In this sample, 68 patients (25.1%) were administered a type of C5 inhibitor and began their treatment 140.9 days postdiagnosis on average. Patients receiving eculizumab continued treatment for an average of 346.1 days but researchers saw a 63.6% discontinuation rate. As for those receiving ravulizumab, these patients continued treatment for an average of 369.4 days and had a 50% discontinuation rate. The PDC for eculizumab and ravulizumab was 48% and 45%, respectively.
Over 25% of patients who received treatment switched their C5 inhibitor. For those on eculizumab, 33.3% ended up changing to ravulizumab at an average time of 654.9 days. Only a single patient on ravulizumab (7.1%) changed to eculizumab.
The analysis further revealed that 108 of the 271 patients with PNH (39.9%) experienced an inpatient stay and 138 (50.9%) had to visit the emergency department. These incidences were for PNH-related events in 10 and 39 patients, respectively. Additionally, 62 patients (22.9%) underwent a blood transfusion and 13 patients (4.85) experienced a bone marrow transplant.
Inpatient costs and pharmaceutical were the main drivers of PNH-associated costs. Per-patient-per-month (PPPM) costs were $18,978, which translated to $227,736 per-patient-per-year (PPPY). A total of $11,182 PPPM (58.9%) of costs were linked to pharmacies. Pharmaceutical costs for eculizumab and ravulizumab was $8988 (81.4%) of these costs.
The authors conclude by noting the value of their study’s evidence regarding treatment patterns in patients with PHN. Furthermore, they emphasize the need for improved care management and development of new treatment options that can counteract treatment delays in newly diagnosed patients with PNH, as well as their rates of inpatient and emergency department visitation.
Reference
Clayton D, Shafrin J, Yen G, et al. Treatment patterns and healthcare resource utilization of patients with paroxysmal nocturnal hemoglobinuria: A retrospective claims data analysis. Clin Appl Thromb Hemost. Published online January 4, 2024. doi:10.1177/10760296231213073
