- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
High Rates of Inhaler Misuse Found Among Patients With COPD Using Soft Mist Inhalers
Misuse of soft mist inhalers (SMIs) is common among patients with chronic obstructive pulmonary disease (COPD), particularly those with low education levels, higher symptom scores, and a shorter disease duration.
Inhaler misuse was common among patients with chronic obstructive pulmonary disease (COPD) only using soft mist inhalers (SMIs), according to a study published in the International Journal of Chronic Obstructive Pulmonary Disease.1
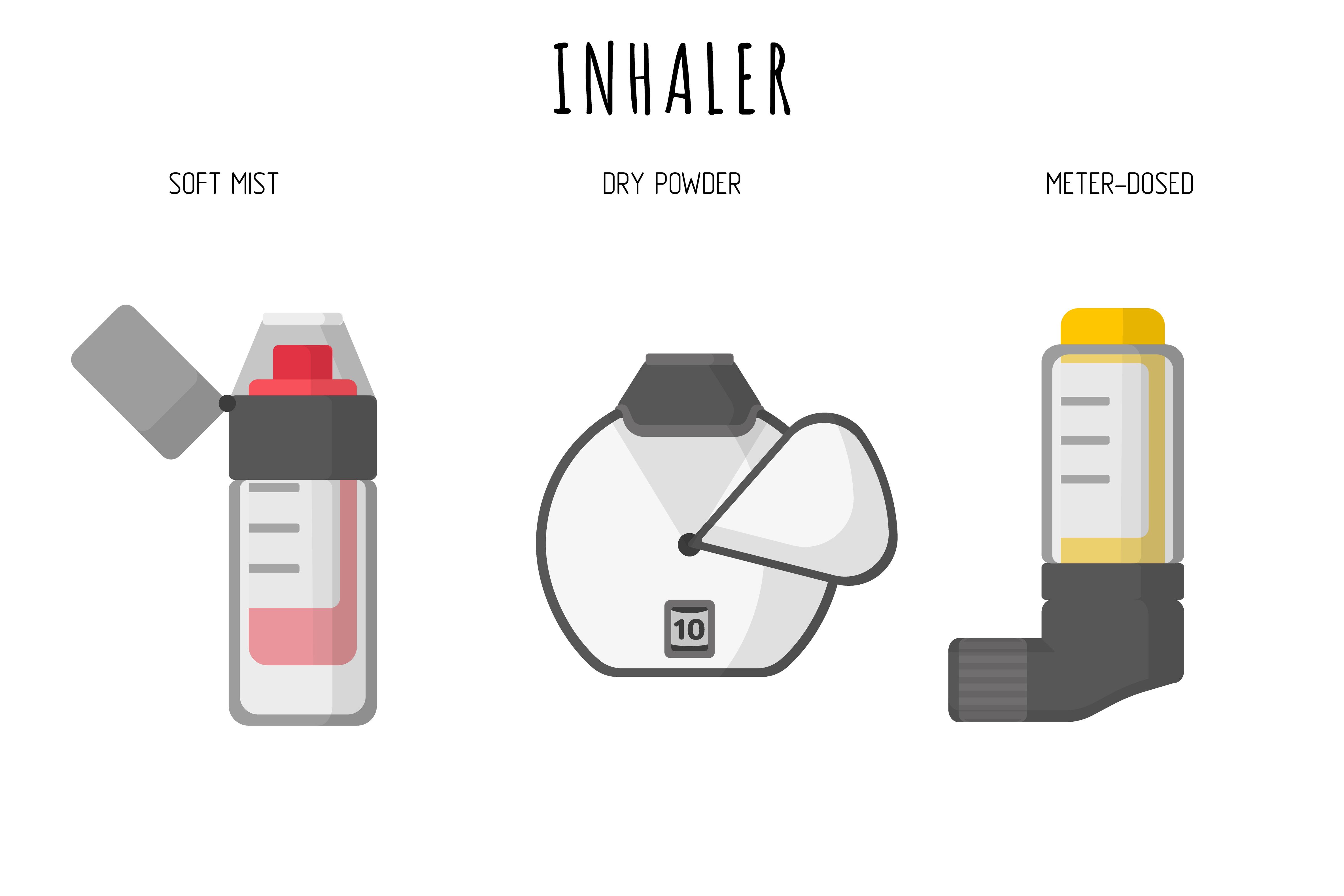
Inhaler therapy is the most common treatment for patients with COPD. Inhalers deliver long-acting bronchodilators to the respiratory tract, which reduce acute exacerbations and improve quality of life, dyspnea, and lung function in patients with COPD.2 The most common inhaler types are the pressurized metered-dose inhaler (pMDI) and the drug powder inhaler (DPI).1 Another inhaler option is the SMI, a propellant-free, multi-dose inhaler that provides slow-moving, long-lasting aerosolization that helps to minimize errors between hand actuation and inhalation.3
The researchers explained that correct inhaler use is essential for effective delivery as errors are associated with acute exacerbations of COPD, increased economic burden, and reduced disease control.1 Previous studies found that misuse of DPI and pMDI is common in clinical practice; however, past studies have not focused on SMI use in patients with COPD, meaning the risk factors associated with SMI misuse remain unclear. Therefore, the researchers conducted a study to evaluate the error rate and identify SMI misuse risk factors in patients with COPD exclusively using SMIs.
Inhalers most commonly used in the treatment of patients with COPD include pressurized metered-dose inhalers (pMDIs), drug powder inhalers (DPIs), and soft mist inhalers (SMIs). | Image Credit: Anastasi17 - stock.adobe.com
To do so, they enrolled patients from a tertiary hospital in South Korea between January 2018 and March 2020. Eligible patients were older than 40 years with a COPD diagnosis based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria. Those eligible also needed to receive ongoing SMI for more than 1 month. Conversely, the researchers excluded patients unable to communicate in written or spoken Korean, using an additional inhaler other than an SMI, or unable to use SMIs individually.
Upon enrollment, the researchers collected information on patients, including their age, sex, COPD duration, body mass index, SMI use duration, and smoking history; they also collected information about patients’ previous exacerbation history, education level, and spirometry measurements. Additionally, the researchers evaluated the patients’ Modified Medical Research Council (mMRC), dyspnea and COPD Assessment Test (CAT) scores.
The researchers analyzed the patients’ critical errors when using SMIs, which they defined as something that affects the deposition of inhaled particles in the lungs, resulting in little or no drug deposition. They also evaluated inhaler adherence, which was self-reported and scored as poor, partial, or good based on complete daily dose intake and whether the drug was taken as needed or not at all. Lastly, the researchers recorded when patients experienced a COPD exacerbation, which they defined as an acute worsening of respiratory symptoms that requires additional therapy; they considered a severe COPD exacerbation to involve a hospitalization or emergency room visit.
The study population consisted of 159 patients, 95% of which were male (n = 151). The mean (SD) age of the included patients was 70.39 (7.31) years, and the mean (SD) duration of COPD and SMI use was 3.33 (4.30) and 2.59 (3.16) years, respectively. The study population included approximately 89.3% current or ex-smokers, and 22% of patients experienced a severe acute exacerbation in the past year.
Also, 80% of patients exhibited good inhaler adherence as most had prior educational experience regarding inhaler use; about 40.3% had high school or higher education. Consequently, the mean (SD) value of forced expiratory volume in 1 second was 61.56 (17.20). Additionally, about 39% of patients had an mMRC score of 2 or greater and a CAT score of 10 or greater.
Of the study population, 136 (85.5%) patients had at least 1 SMI use error, the most frequently observed being “no exhalation before inhalation” (71.1%) and “no breath-holding for 5-10 seconds” (41.5%). Similarly, 74 patients (46.5%) made at least 1 critical error, the most common being “failure to inhale deeply and slowly” (39%) and “poor coordination between hand actuation and inhalation” (27%).
Through the binary logistic regression analysis, the researchers found that SMI misuse was significantly associated with a low education level (adjusted odds ratio [aOR], 3.258; 95% CI, 1.175-9.034; P = .023), a CAT score of 10 or greater (aOR, 3.341; 95% CI, 1.008-11.075; P = .049) and a disease duration of 2 years or less (aOR, 3.819; 95% CI, 1.253-11.637).
Lastly, the researchers acknowledged their limitations, one being that it was a single-center study and excluded those unable to communicate in Korean. Therefore, selection bias was unavoidable. Also, the researchers did not assess comorbidities or other factors potentially linked to inhaler misuse. However, the researchers gave clinicians advice based on their findings.
“…physicians should be aware of the potential misuse of SMI in the course of COPD treatment, especially in the early period after the diagnosis of COPD,” the authors concluded.
References
- Jang JG, Lee YS, Hong KS, Ahn JH. Risk factors associated with misuse of soft mist inhaler in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2024;19:1225-1232. doi:10.2147/COPD.S458200
- Agustí A, Celli BR, Criner GJ, et al. Global Initiative for Chronic Obstructive Lung Disease 2023 report: GOLD executive summary. Eur Respir J. 2023;61(4):2300239. doi:10.1183/13993003.00239-2023
- Hochrainer D, Hölz H, Kreher C, Scaffidi L, Spallek M, Wachtel H. Comparison of the aerosol velocity and spray duration of Respimat Soft Mist inhaler and pressurized metered dose inhalers. J Aerosol Med. 2005;18(3):273-282. doi:10.1089/jam.2005.18.273
