- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
High Magnesium Depletion Scores Linked to Increased Mortality in US Patients With Hypertension
Having a higher magnesium depletion score (MDS) independently predicts increased all-cause and cardiovascular mortality risks in US patients with hypertension (HTN), emphasizing the importance of early HTN prevention and magnesium deficiency management.
Having a higher magnesium depletion score (MDS) independently predicts an elevated mortality risk in US patients with hypertension (HTN), according to a study published in Biological Trace Element Research.1
The researchers explained that HTN leads to serious complications, including stroke and cardiovascular disease (CVD).2 As of 2019, about 52% of females and 43% of males globally have been diagnosed with HTN, and it has led to approximately 10.4 million deaths each year worldwide.3,4 Consequently, early HTN prevention is needed.1
They noted that magnesium has anti-inflammatory properties that help to reduce inflammation in the vascular endothelium, reducing HTN risk.5 The researchers evaluated patients' magnesium levels using MDS, an assessment tool that considers all factors impacting renal magnesium reabsorption efficiency.6 This makes it capable of accurately measuring magnesium utilization and identifying those with reduced magnesium absorption.
Although a strong positive relationship has been established between MDS and mortality in patients with CVD, the researchers noted that the link between MDS and mortality in patients with HTN is uncertain.1 Consequently, they investigated the role of MDS in predicting outcomes of patients with HTN to help prevent future fatalities in this population.
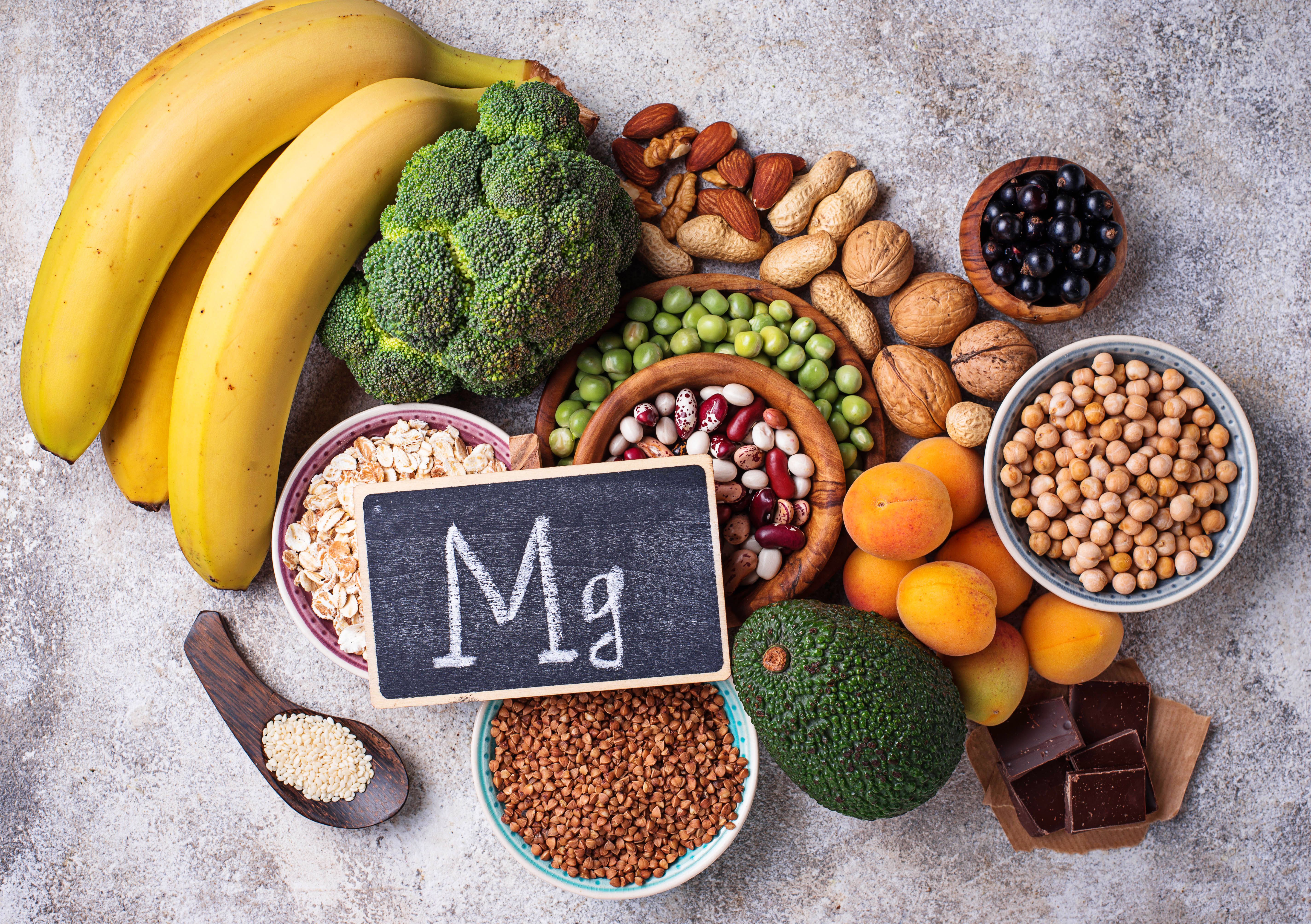
The magnesium depletion score (MDS) is significantly correlated with all-cause and cardiovascular mortality in patients with hypertension (HTN). | Image Credit: Yulia Furman - stock.adobe.com
Consistent with previous research, MDS was calculated for each patient by adding up the scores of 4 specific items. Patients scored 1 point for the current use of diuretics, the current use of proton pump inhibitors, and heavy alcohol consumption, respectively. They also scored 1 point for an estimated glomerular filtration rate (eGFR) between 60 mL/min/1.73 m2 and 90 mL/min/1.73 m2; an eGFR less than 60 mL/min/1.73 m2 scored 2 points.
Patients with scores between 0 and 1 were classified into the lower MDS group, those with a score of 2 were put into the middle MDS group, and those with scores from 3 to 5 were placed into the higher MDS group.
The researchers used Kaplan-Meier curves to determine survival differences between MDS groups. Additionally, they analyzed the association between MDS and mortality using 3 weighted multivariate Cox regression models. Model 1 was not adjusted for confounders, but model 2 adjusted for various confounders, like age, race, sex, and body mass index (BMI); model 3 was a fully adjusted model corrected for additional variables, like diabetes, average magnesium intake, and CVD.
To conduct their study, the researchers analyzed patients within the National Health and Nutrition Examination Survey (NHANES), a nationally representative cross-sectional survey that accurately portrays the health and nutrition levels of the US population. Their study population encompassed all patients in the NHANES database who were 20 years or older between 2003 and 2018. However, they excluded those without HTN, those who lacked the information needed to calculate the MDS, and those with incomplete follow-up or covariate data.
Therefore, the study population consisted of 12,485 patients. The average patient age was 57.36 years, and 49.85% were male. Compared with those with lower MDS, patients with higher MDS tended to be older, non-Hispanic white, female, and never smokers.
Of the study population, there were 2537 cases of all-cause mortality and 707 cases of cardiovascular mortality during the median 90-month follow-up period. Through the Kaplan-Meier curves, the researchers determined that the higher MDS group had greater all-cause and cardiovascular mortality risks than the lower MDS group (P < .001).
Also, models 1 and 2 found a significant association between MDS and mortality. After controlling for all confounding variables, the higher MDS group had substantially elevated all-cause (HR, 1.31; 95% CI, 1.10-1.54) and cardiovascular (HR, 1.63; 95% CI, 1.19-1.22) mortality risks compared with the lower MDS group. Therefore, elevated MDS levels were associated with a prominent rise in both all-cause and cardiovascular mortality risks (P < .05).
Lastly, the researchers acknowledged their limitations, one being that they cannot eliminate the influence of other unknown factors on MDS despite controlling for multiple potential confounders. Also, since the study population consisted of US patients, their findings cannot be generalized to those in other countries or regions. Despite these limitations, the researchers suggested areas for future research based on their findings.
“In the future, more studies are needed to further elucidate the mechanism between MDS and prognosis in HTN patients and to explore the potential benefits of correcting magnesium deficiency in improving their prognosis,” the authors wrote.
References
- Song, J., Zhang, Y., Lin, Z. et al. Higher magnesium depletion score increases the risk of all-cause and cardiovascular mortality in hypertension participants. Biol Trace Elem Res (2024). doi:10.1007/s12011-024-04254-w
- Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-1357. doi:10.1161/HYPERTENSIONAHA.120.15026
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants Lancet. 2021;398(10304):957-980. doi:10.1016/S0140-6736(21)01330-1
- Weber MA, Poulter NR, Schutte AE, et al. Is it time to reappraise blood pressure thresholds and targets? a statement from the International Society of Hypertension-a global perspective. Hypertension. 2016;68(2):266-268. doi:10.1161/HYPERTENSIONAHA.116.07818
- Houston MC, Harper KJ. Potassium, magnesium, and calcium: their role in both the cause and treatment of hypertension. J Clin Hypertens (Greenwich). 2008;10(7 Suppl 2):3-11. doi:10.1111/j.1751-7176.2008.08575.x
- Fan L, Zhu X, Rosanoff A, et al. Magnesium Depletion Score (MDS) Predicts Risk of Systemic Inflammation and Cardiovascular Mortality among US Adults. J Nutr. 2021;151(8):2226-2235. doi:10.1093/jn/nxab138
