- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Glomerular Filtration Rate Change and Outcomes in Type 2 Diabetes
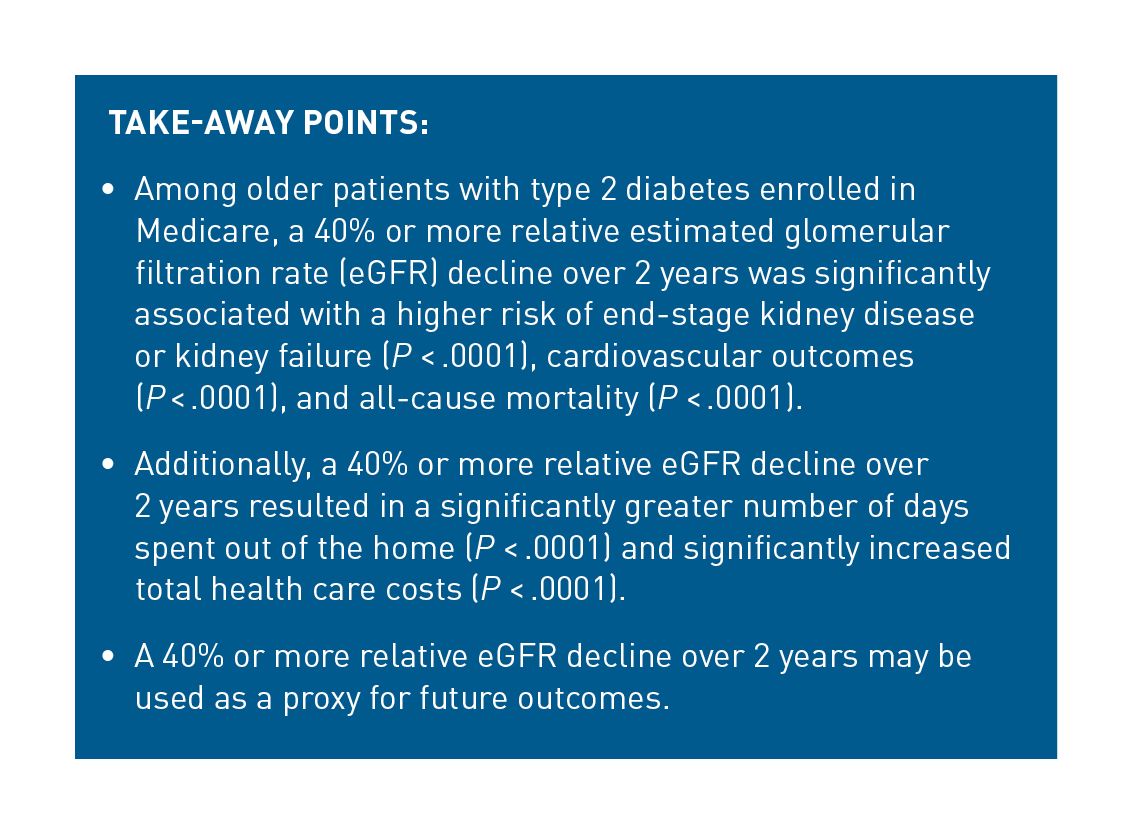
Objectives: To assess the relationship between relative estimated glomerular filtration rate (eGFR) change and outcomes in patients with type 2 diabetes (T2D).
Study Design: This retrospective cohort study utilized administrative claims (Humana Research Database) for patients with T2D aged 65 to 89 years, enrolled in a Medicare Advantage plan, with an initial eGFR of 25 to 89 mL/min/1.73m2 in 2008 to 2017, and a second eGFR measurement within 3 to 24 months after the identification date.
Methods: The primary exposure was relative decline in eGFR of 40% or more in a 2-year period. Outcomes included end-stage kidney disease (ESKD) or kidney failure, a composite cardiovascular (CV) outcome, and all-cause mortality assessed with multivariable adjusted survival models. Days out of the home and all-cause total costs were assessed using multivariable adjusted generalized linear models.
Results: A total of 288,170 patients were included. The adjusted HR for ESKD or kidney failure was 4.38 (95% CI, 3.99-4.81) in patients with 40% or greater decline versus those with a decline of less than 40%. The adjusted HR was 1.67 (95% CI, 1.53-1.82) for the composite CV outcome and 1.98 (95% CI, 1.87-2.10) for all-cause mortality. Patients with a 40% or greater relative decline had 2.23 times higher all-cause total per patient per month costs ($1910 difference) and 1.82 times higher odds of 7 or more days out of the home versus those with less than 40% relative eGFR decline.
Conclusions: Our results indicate that a relative eGFR decline of 40% or greater is associated with an increased risk of ESKD or kidney failure, CV outcomes and all-cause mortality, and increased health care resource utilization and costs.
Am J Manag Care. 2021;27(suppl 8):S160-S167. https://doi.org/10.37765/ajmc.2021.88658
For author information and disclosures, see end of text.
Introduction
An estimated 37 million, or 15%, of all adults in the United States have chronic kidney disease (CKD).1 Those with CKD have nearly twice the mortality rate compared with those without CKD, as well as higher rates of cardiovascular disease (CVD) and related events.2 In addition, approximately 37% of patients with type 2 diabetes (T2D) also have CKD.2 As such, the older patient population with T2D is at particular risk for morbidity and mortality related to CKD.
The clinical consequences of CKD are substantial; subsequently, health care resource utilization (HCRU) and costs for these patients are also high. In fact, hospitalizations and readmissions are higher among those with CKD than without CKD, and as age increases, hospitalizations and readmissions increase, particularly for those over 85 years of age.2 Medicare spending alone exceeded $70 billion for CKD in 2018, with 47% higher expenditures for patients with any diabetes and CKD compared with those with any diabetes and without CKD. Patients whose CKD progresses to end-stage kidney disease (ESKD) account for an additional $49 billion; spending on treatment, particularly dialysis, is a substantial cost driver in this population.2
Patients often progress slowly to ESKD or kidney failure, with few overt symptoms until late in the disease, presenting challenges for development of treatments in this therapeutic area. Although doubling of serum creatinine (ie, halving of estimated glomerular filtration rate [eGFR]) is an accepted surrogate end point by the FDA,3 it takes a long time to occur, which makes it a difficult surrogate end point to use in clinical trials. As such, the associations between lesser changes in eGFR (eg, 30% or 40%) have been more recently explored as surrogate end points for ESKD or CKD progression.3,4 These changes and their associations with outcomes have been evaluated in multiple prospective studies, meta-analyses, and observational studies of patients enrolled in clinical trials, although few use administrative claims or electronic health record (EHR) data.5-14 Whereas results of a pooled analysis of clinical trials showed that a general linear trend in eGFR decline occurs in most patients who have kidney disease with or without T2D, there may be greater fluctuations and differences in these trajectories in patients with T2D, warranting specific evaluations in this high-risk patient population.13
Additional real-world evaluations to support the validity of change in eGFR as a surrogate end point for clinical outcomes (eg, ESKD) or other outcomes, such as HCRU or cost, in large, representative populations of patients over time are warranted. As such, the primary purpose of this study was to examine the relationship between relative eGFR change and outcomes in patients with T2D.
Methods
Study Design
This study employed an observational, retrospective cohort design (Figure 1). Data used for this study were collected from patients with a diagnosis of T2D and who enrolled in a Medicare Advantage Prescription Drug (MAPD) plan through Humana Inc between January 1, 2008, and December 31, 2017. Enrollment, medical claims, pharmacy claims, and laboratory data were linked via a unique identifier. The identification date was the date of the first serum creatinine measure used to calculate eGFR. The latest available serum creatinine measure in the 3 to 24 months after the identification date was set as the second value and used to calculate eGFR change. Patients were required to have 12 months of preidentification continuous enrollment, which served as the baseline period. The index date was set as 24 months after the identification date.
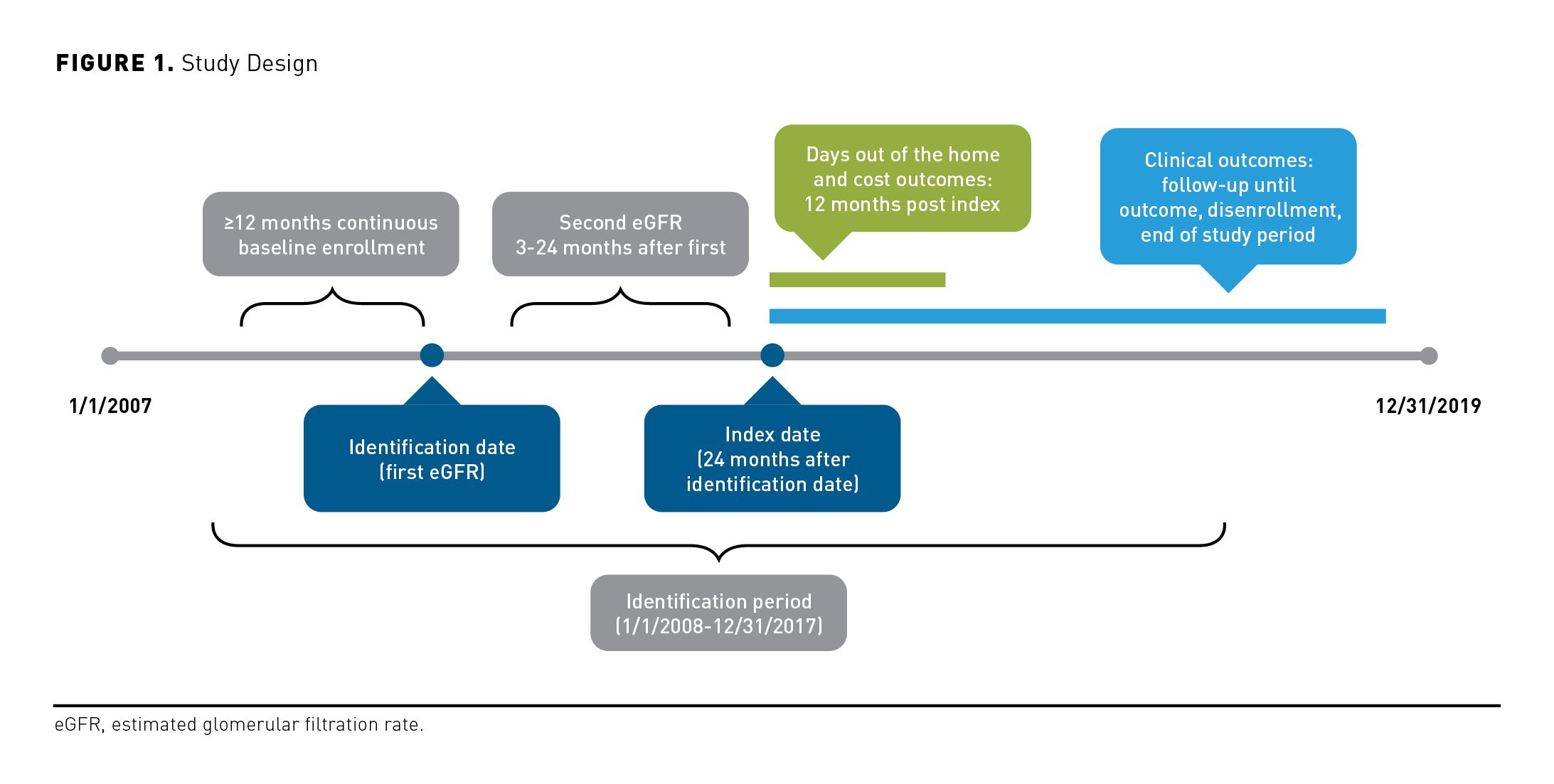
Clinical outcomes were assessed throughout all available patient follow-up, starting at the index date through December 31, 2019. HCRU and cost measures were evaluated up to 12 months post index.
Patients between the ages of 65 to 89 years with T2D and without initial stage V CKD (eGFR < 15 mL/min/1.73 m2) or ESKD (diagnosis, renal transplant, or dialysis) and with an eGFR of 25 to 89 mL/min/1.73 m2 at the identification date and at least a second serum creatinine measurement within 3 to 24 months of the first value were included. Patients with any of the following prior to the index date were excluded: (a) disenrollment or death (all analyses), (b) ESKD or stage V CKD (for the outcomes analyses of ESKD or kidney failure), or (c) a cardiovascular (CV) event (for the CV outcomes analyses). Patients with a diagnosis of type 1 diabetes in the baseline period were also excluded from all analyses.
Exposure and Outcomes
The relative change in eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration formula15 as the latest eGFR value within 3 to 24 months after the identification date minus the identification eGFR value divided by identification value and multiplied by 100 to yield a relative percentage change. The exposure for the primary analysis was defined as relative eGFR decline of 40% or more in the 24-month postidentification period.
Three clinical outcomes were assessed: ESKD or kidney failure, composite CV outcome, and all-cause mortality. Patients with 1 or more inpatient or outpatient medical claims for dialysis or renal transplant or a sustained eGFR less than 15 mL/min/1.73m2 (2 eGFR < 15 mL/min/1.73m2 values ≥ 4 weeks apart) were identified as having the ESKD or kidney failure outcome. The composite CV outcome was defined as a nonfatal myocardial infarction, stroke, hospitalization for heart failure, or death in hospital or within 30 days of discharge for patients with a principal CV-related admission (detailed in eAppendix, available at ajmc.com). All-cause mortality based on Centers for Medicare & Medicaid Services Social Security Administration records was reported.
HCRU was measured as the number of days out of the home (ie, the number of days a patient spent out of their primary ambulatory residence for health care). This was calculated as the total number of days spent in hospitals and long-term care facilities plus 0.75 (based on 18 hours of 24-hour period) times the number of days with emergency department (ED) visits plus 0.0835 (based on 2 hours of 24-hour period) times number of days with outpatient visits divided by the follow-up time (as study end date [death date, hospice date, or index date plus 365, whichever occurred first]) minus the index date. This measure aligns closely to the healthy days at home measure, which was developed in collaboration with the Medicare Payment Advisory Commission and reflects population-based quality of care of health care organizations among Medicare beneficiaries.16 Fewer days out of the home (ie, days patients are not in facility-based settings) reflects a patient-centered approach to evaluating quality of care. The proportion of patients with 7 or more days out of the home was used as the outcome of interest.
All-cause total health care costs were calculated based on the health plan total allowed amount for a given procedure or health care encounter. Medical (eg, inpatient and outpatient) and pharmacy costs were included and measured as per person per month (PPPM). Costs for all services were adjusted to 2019 US dollars using the Medical Consumer Price Index.
Statistical Analysis
Demographics, enrollment data, clinical characteristics, and HCRU were described for the identified patients in the baseline period. Outcomes were described by the primary independent variable of 40% or more versus less than 40% eGFR relative decline. Unadjusted Kaplan-Meier curves were generated for each of the clinical outcomes, stratified by the exposure.
The association between relative change in eGFR (binary variable, ≥ 40% relative decline vs < 40% decline) and the 3 clinical outcomes were evaluated in unadjusted and multivariable confounder adjusted Cox survival models after the index date. All-cause mortality was included as a competing event in the non–all-cause mortality by using the Fine and Gray method to model the subdistribution hazard function.17 The crude and adjusted HRs with 95% CI and P values were reported. To ensure that patients with at least 40% relative decline were represented well in the models and to reduce possible bias with a large sample of patients with less than 40% decline,18 10% of patients with less than 40% decline were randomly sampled prior to modeling. This 10% was compared with the remaining 90% using standardized differences to ensure comparability (eAppendix Table 1). The 10% representative sample population was then used for modeling. Independent baseline variables, such as demographic and socioeconomic factors (age, sex, race, region of residence, population density, low-income subsidy, dual eligibility), clinical characteristics (Elixhauser score, Diabetes Complications and Severity Index score, initial eGFR), laboratory values (urine albumin-to-creatinine ratio, cholesterol, glycated hemoglobin), glucose-lowering and CV medication use, HCRU (inpatient hospitalizations, ED visits, outpatient visits), and total all-cause costs were included in the models based on a priori considerations. Similarly, the proportion of patients with 7 or more days out of the home was modeled using logistic regression, and cost outcome was modeled on a PPPM basis using a generalized linear model with a log link.
Adjusted survival models and generalized linear models were also created for subgroup and sensitivity analyses. Outcomes were evaluated among 2 subgroups of patients with initial eGFR values of 25 to 59 mL/min/1.73m2 and 60 to 89 mL/min/1.73m2. Additional subgroups included patients stratified by the following different categories of relative eGFR change: increase or stable, decrease of up to 29.9%, decrease of 30.0% to 39.9%, decrease of 40.0% to 56.9%, and decrease of 57% or more. Sensitivity analyses were conducted for patients with a sustained relative decline in eGFR (ie, with an additional eGFR measurement suggesting a sustained relative decline of ≥ 40% with values ≥ 4 weeks apart and before the index date) and with an eGFR relative decline using a 1-year period to assess the relative change in eGFR. Analyses of the primary outcomes using the full cohort of patients were also conducted to ensure comparability with the analyses conducted with the sample.
All analyses were conducted in SAS Enterprise Guide version 7.15. The study was approved by an independent institutional review board prior to initiation.
Results
Study Population
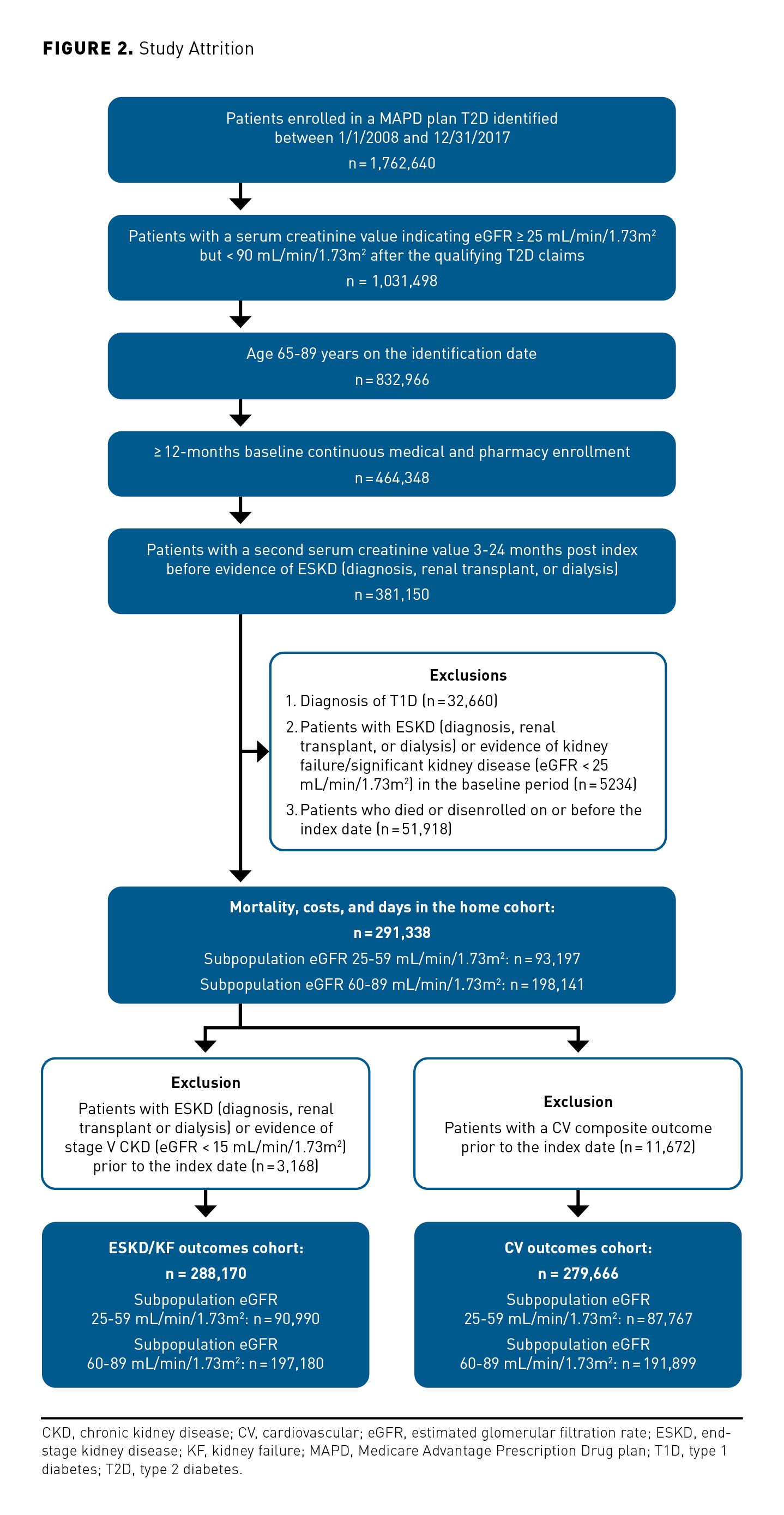
A total of 291,338 patients were eligible for the all-cause mortality, days out of the home, and costs analyses, of whom 5440 (1.9%) had a 40% or greater relative eGFR decline (Figure 2). When applying the outcome-specific exclusions for ESKD or kidney function and composite CV outcomes, 288,170 patients were included for the ESKD or kidney failure outcomes analyses and 279,666 patients for the composite CV outcomes; 4581 (1.6%) and 4527 (1.6%) had a 40% or greater relative eGFR decline, respectively.
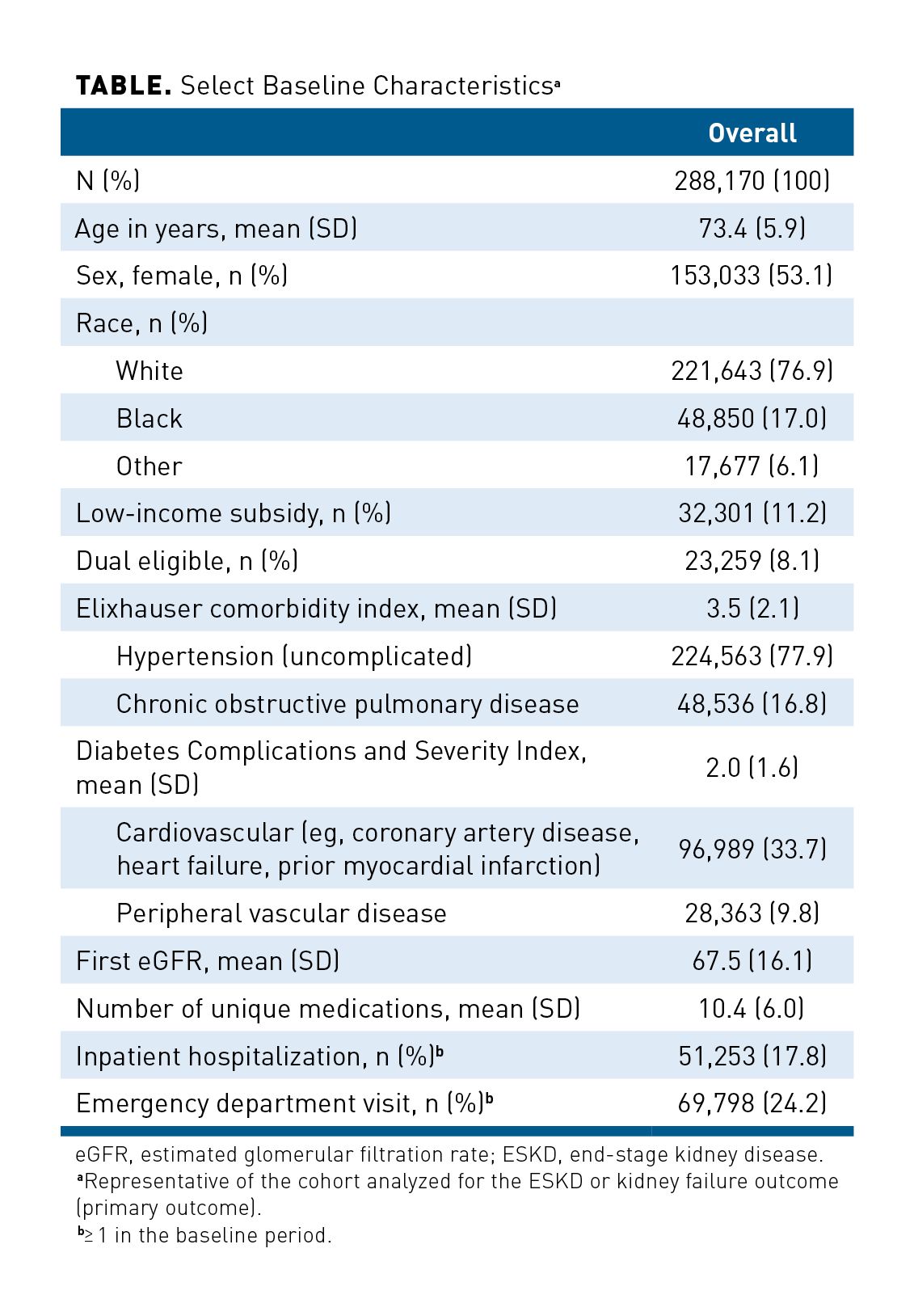
Baseline Characteristics
Select baseline characteristics for the overall study population are provided in the Table. Patients with a relative eGFR decline of 40% or greater were, on average, older, with more comorbidities and greater baseline HCRU. Full baseline characteristics stratified by eGFR change (< 40% and ≥ 40%) and stratified by initial eGFR (25-59 mL/min/1.73m2 and 60-89 mL/min/1.73m2) are provided in the eAppendix (eAppendix Table 2).
Analyses
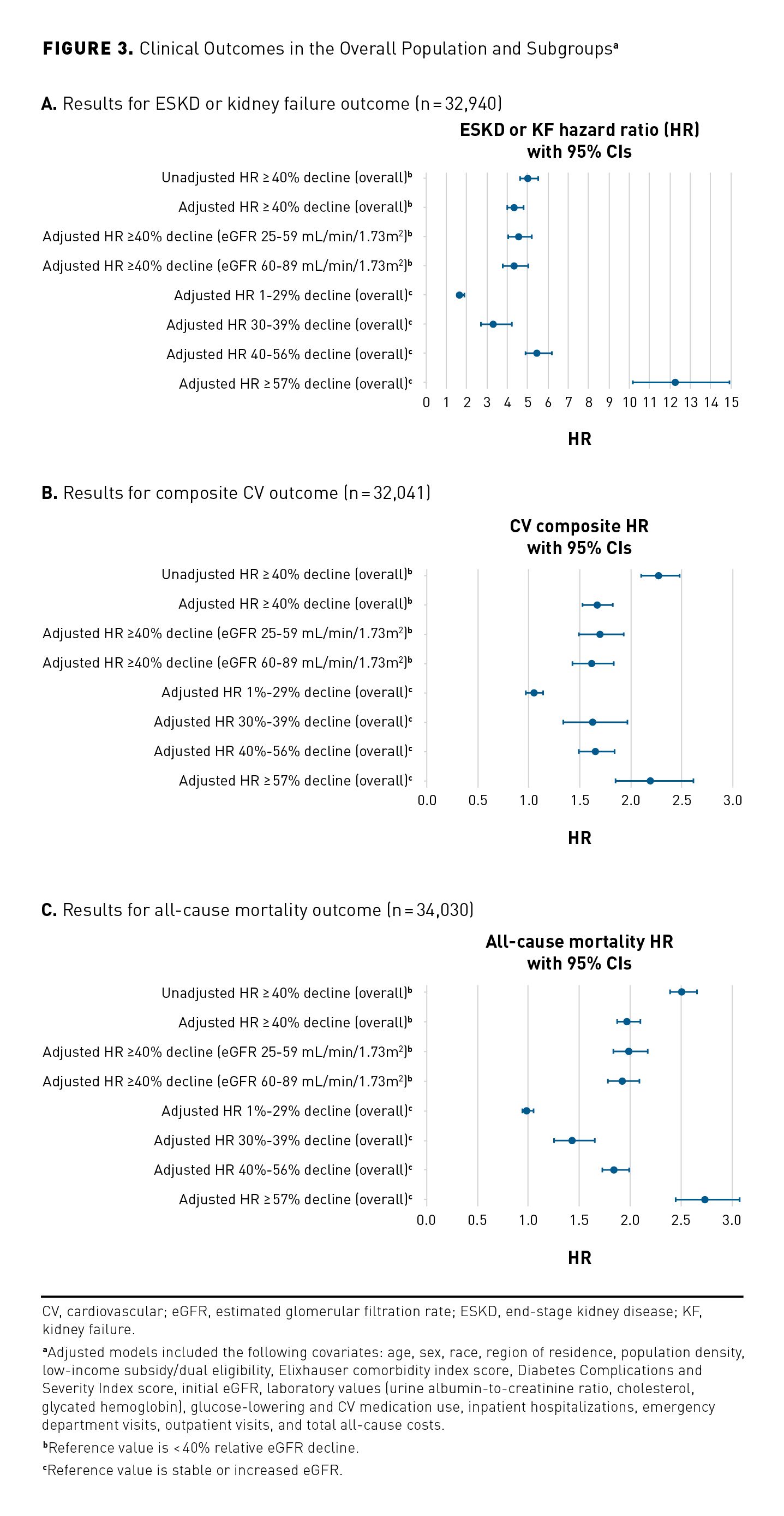
Unadjusted and adjusted model results for the overall population and adjusted model results for the subgroups for clinical outcomes were calculated (Figure 3); unadjusted descriptive results are available in the eAppendix (eAppendix Table 3 and eAppendix Figures 1-3). Patients with a 40% or greater relative decline had a 4.38 (95% CI, 3.99-4.81), 1.67 (95% CI, 1.53-1.82), and 1.98 (95% CI, 1.87-2.10) higher risk of ESKD or kidney failure, composite CV outcome, and all-cause mortality, respectively, than those with relative eGFR decline of less than 40%.
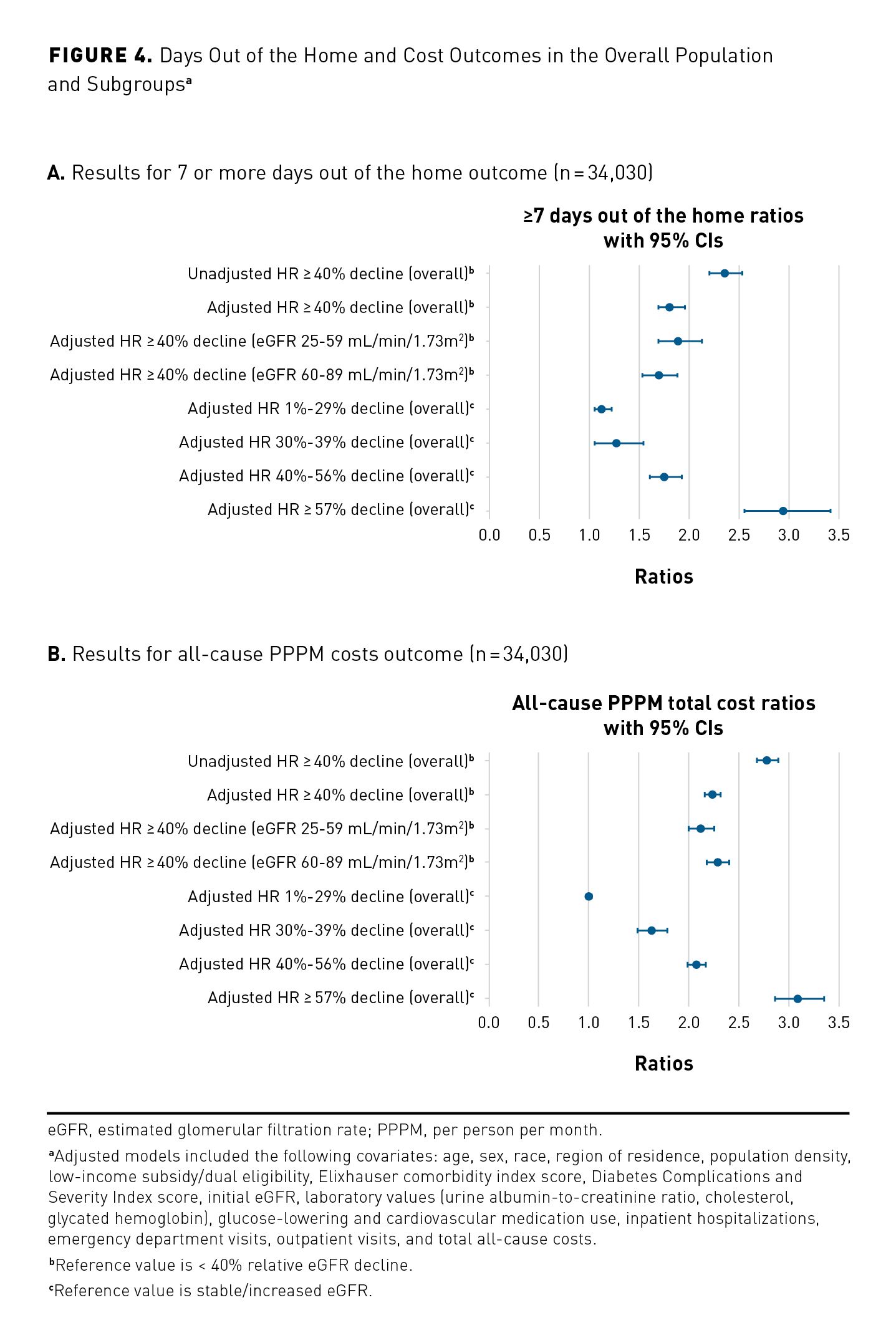
The unadjusted and adjusted model results for the overall population and adjusted model results for subgroups for days out of the home and all-cause total PPPM costs are in Figure 4. Patients with a 40% or greater relative decline had a 1.82 (95% CI, 1.69-1.96) and 2.23 (95% CI, 2.15-2.31) higher risk of 7 or more days out of the home and higher all-cause total PPPM costs, respectively, compared with those with a relative eGFR decline of less than 40%. This translates to an adjusted mean difference of 12.6% (95% CI, 11.6%-13.5%), with 7 or more days out of the home for those with a 40% or greater relative decline compared with those with a less than 40% relative decline. For costs, the adjusted difference for the overall population was $1910 PPPM (95% CI, $1839-$1982) for patients with a 40% or greater relative decline compared with patients with a less than 40% relative decline. As with the clinical outcomes, there were increased days out of the home and increased PPPM costs as the magnitude of the relative eGFR decline increased.However, results across the overall cohort and the subgroups stratified by initial eGFR were consistent (eAppendix Table 4). Results across outcomes in the sensitivity analyses were consistent with those of the primary analysis (eAppendix Table 5).
Discussion
This study examined the relationships between relative changes in eGFR and clinical health care resource use and cost outcomes among patients with T2D. Although several clinical trials and meta-analyses have been published regarding the association of eGFR decline with clinical outcomes, few studies have evaluated the relationship in a large population using administrative claims or EHR data. In this study, we found that the adjusted HR of ESKD or kidney failure was significantly higher by a magnitude of more than 4-fold among patients with a 40% or greater relative eGFR decline over a 2-year period compared with patients with a less than 40% decline, stable, or increased eGFR for the overall population, indicating that there is evidence for use of this measure as a surrogate end point for CKD progression.
Furthermore, when comparing patients with relative eGFR declines of 40% to 56% and 57% or greater with those specifically with stable or increased eGFR, the adjusted hazard of ESKD or kidney failure was 5.5- and 12.3-fold for the primary population, respectively. These associations were stronger among those patients with an initial eGFR of 25 to 59 mL/min/1.73m2. In a recent meta-analysis, Coresh et al reported similar trends with the association of ESKD and 2-year change in eGFR. However, the magnitude of estimates was stronger between a relative eGFR decline of 40% to 56% and 57% or greater and the ESKD outcome. The cohorts included in the meta-analysis were diverse not only in age but also in baseline comorbidities (eg, diabetes). The outcome assessed in that study was initiation of renal replacement therapy or death due to kidney disease, which varies from the definition we used in these analyses. Additional literature has also noted the association between increased risk of ESKD and declines in eGFR of 40% or more, further supporting use of this measure as a surrogate end point for CKD outcomes.4,5
Studies have explored whether lesser declines in eGFR (eg, ≥ 30%) may also be utilized as a surrogate end point for clinical outcomes. We found that patients with a 30% to 39% relative decline in eGFR had a 3.4-fold increased risk of ESKD or kidney failure compared with those with stable or increased eGFR over a 2-year period. Although this risk is lower than noted for those with a relative decline of at least 40%, it remains clinically and statistically significant and also parallels results from Coresh et al.10 Although a decline in eGFR of 40% or more is considered a stronger surrogate for ESKD outcomes, a decline in eGFR of 30% or more has also been noted as a possible valid measure under some circumstances.4,19
When assessing the relative eGFR change in a 1-year period, HR estimates, although slightly lower than those of the 2-year primary analysis, remained significant and consistent for the primary population and across subgroups stratified by initial eGFR, suggesting that the associations are robust to the time period chosen. Coresh et al conducted similar sensitivity analyses and also found lower estimates with the 1-year baseline period for eGFR change; however, the authors concluded that the association remained strong and relatively consistent.10 We observed that 65% of patients who showed a large, short-term decline in eGFR had improved (higher) eGFR results in the second year. This may suggest that the eGFR change in the first year may reflect more acute fluctuations or that this measurement is not as reliable as an eGFR calculated over longer periods of time (ie, 2 years).
CKD is an established risk factor for CVD and mortality, and management of modifiable risk factors can slow progression of kidney disease as well as reduce the risk of CV events.20 In the primary population of our study, we found a nearly 2-fold higher hazard of composite CV outcomes in patients with a relative eGFR decline of at least 40% over a 2-year period compared with those with a relative decline of less than 40%, which was generally consistent across subgroups and sensitivity analyses. Rebholz et al also noted a 2 times higher hazard of CVD among those with a 30% or greater eGFR decline; however, that change was noted over a 6-year period among a community-based cohort.7 Other studies have also reported declines in eGFR associated with CVD outcomes.21-24
In the current study, a relative decline in eGFR of 40% or greater was associated with a 2-fold increased HR in all-cause mortality in the primary population as well as in the subgroups and sensitivity analyses. Other studies have also reported similar increases in mortality with higher declines in eGFR.7,10,21,24
The odds of incurring 7 or more days out of the home overall and across subgroups, including those with a 40% or higher relative eGFR decline compared with those with less than a 40% decline, were nearly doubled.When a patient is out of the home for a substantial number of days, the cost drivers and opportunities for intervention to reduce those days are investigated. Care management teams may then initiate outreach programs based on trends in utilization.
Patients with a less than 40% relative decline in eGFR had more than twice the PPPM total all-cause costs, which was generally consistent across subgroups and sensitivity analyses. As adjusted annualized costs, these patients would have incurred nearly an additional $23,000 per year compared with patients with less than 40% relative declines. Higher costs with CKD progression or, ultimately, ESKD, have been similarly reported.25-27 Preventing or delaying disease progression may confer clinical benefits and cost savings to the health care system by reducing HCRU for patients with CKD and related comorbidities.
Limitations
This study utilized administrative claims data, which are subject to certain limitations, such as the potential for missing data and errors in coding. When utilizing retrospective data, relationships may be established based on a statistical or temporal basis, but causal inference may not be directly determined. Adjusted analyses were used, but unmeasured confounders could nonetheless create bias. However, an extensive list of demographics, clinical, laboratory, HCRU, and cost variables was available. A further limitation to the study design is that patients who had the events of interest in the period between the last eGFR measurement and the index date (2 years post identification) were not included in the analysis. This could have created a selection bias toward a potentially “healthier” population, especially in patients with a previously strong eGFR decline, thus reducing the number of possible events, leading to a potential underestimation of the outcome rates and relative risk estimates. Therefore, we conducted sensitivity analyses with a 1-year time period to determine the impact of the time period for eGFR measurement chosen on outcomes; however, results were similar, suggesting that the results of the 2-year primary analysis were robust.
Further, our study utilized data from a US Medicare population, so the results may not be generalizable for younger patients in commercial plans or for patients outside of the United States. Moreover, cost data for patients following an ESKD diagnosis may not be completely accounted for in claims due to bundled payments. Additionally, during the period of this study, patients with ESKD were not eligible for enrollment into MAPD plans. However, in this study, the majority of HCRU and cost data for these patients were collected prior to an indication of ESKD (diagnosis, transplant, dialysis) and should not significantly affect the results.
Conclusions
Our study indicates that a relative eGFR decline of 40% or more is associated with an increased risk of ESKD or kidney failure, CV events, and all-cause mortality, as well as with increased HCRU and total health care costs.
Author affiliations: Bayer AG (NS), Berlin, Germany; Bayer AG (TE), Wuppertal, Germany; Humana Healthcare Research, Inc (EOC, MKP, RS), Louisville, KY; Humana Inc (MC, MT), Louisville, KY; University of Tennessee Health Science Center (CPK), Memphis, TN.
Funding source: This study and supplement were funded by Bayer AG.
Author disclosures: Dr Caplan, Dr Pasquale, and Mr Sheer are employees of Humana Healthcare Research, a wholly owned subsidiary of Humana. Ms Cockrell and Dr Tindal are employed by Humana Inc. Ms Cockrell owns restricted stock with Humana. Dr Evers and Dr Schmedt are employees of Bayer AG and also report an institutional conflict of interest with subject matter discussed in the manuscript. Dr Kovesdy reports serving as a consultant or on paid advisory boards for Akebia Therapeutics, Ardelyx, AstraZeneca, Bayer, Boehringer Ingelheim, Cara Therapeutics, Reata Pharmaceuticals, and Tricida, as well as receiving royalties for UpToDate Inc. Dr Pasquale, Mr Sheer, and Dr Tindal own stock at Humana Inc.
Authorship information: Concept and design (EOC, MC, TE, CPK, MKP, RS, NS, MT); acquisition of data (TE); analysis and interpretation of data (EOC, TE, CPK, MKP, RS, NS, MT); drafting of the manuscript (EOC, NS); critical revision of the manuscript for important intellectual content (EOC, MC, CPK, MKP, RS, NS, MT); statistical analysis (RS); administrative, technical, or logistical support (EOC, MC); and supervision (TE, MKP).
Address correspondence to: Eleanor O. Caplan, PharmD, PhD, Humana Healthcare Research, Inc, 500 W Main St, Louisville, KY 40202. Email: ecaplan@humana.com
References
1. Chronic kidney disease in the United States, 2019. US Department of Health and Human
Services/Centers for Disease Control and Prevention. March 5, 2019. Accessed February 2, 2021. www.cdc.gov/kidneydisease/pdf/2019_National-Chronic-Kidney-Disease-Fact-Sheet.pdf
2. Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2019 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2020;75(suppl 1):A6-A7. doi:10.1053/j.ajkd.2019.09.003
3. Thompson A, Lawrence J, Stockbridge N. GFR decline as an end point in trials of CKD: a viewpoint from the FDA. Am J Kidney Dis. 2014;64(6):836-837. doi:10.1053/j.ajkd.2014.09.006
4. Levey AS, Inker LA, Matsushita K, et al. GFR decline as an end point for clinical trials in CKD: a scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am J Kidney Dis. 2014;64(6):821-835. doi:10.1053/j.ajkd.2014.07.030
5. Inker LA, Lambers Heerspink HJ, Mondal H, et al. GFR decline as an alternative end point to kidney failure in clinical trials: a meta-analysis of treatment effects from 37 randomized trials. Am J Kidney Dis. 2014;64(6):848-859. doi:10.1053/j.ajkd.2014.08.017
6. Kovesdy CP, Coresh J, Ballew SH, et al; CKD Prognosis Consortium. Past decline versus current eGFR and subsequent ESRD risk. J Am Soc Nephrol. 2016;27(8):2447-2455. doi:10.1681/ASN.2015060687
7. Rebholz CM, Grams ME, Matsushita K, et al. Change in multiple filtration markers and subsequent risk of cardiovascular disease and mortality. Clin J Am Soc Nephrol. 2015;10(6):941-948. doi:10.2215/CJN.10101014
8. Rebholz CM, Inker LA, Chen Y, et al; Chronic Kidney Disease Biomarkers Consortium. Risk of ESRD and mortality associated with change in filtration markers. Am J Kidney Dis. 2017;70(4):551-560. doi:10.1053/j.ajkd.2017.04.025
9. Naimark DMJ, Grams ME, Matsushita K, et al; CKD Prognosis Consortium. Past decline versus current eGFR and subsequent mortality risk. J Am Soc Nephrol. 2016;27(8):2456-2466.
doi:10.1681/ASN.2015060688
10. Coresh J, Turin TC, Matsushita K, et al. Decline in estimated glomerular filtration rate and subsequent risk of end-stage renal disease and mortality. JAMA. 2014;311(24):2518-2531.
doi:10.1001/jama.2014.6634
11. Tsai C-W, Ting I-W, Yeh H-C, Kuo C-C. Longitudinal change in estimated GFR among CKD patients: a 10-year follow-up study of an integrated kidney disease care program in Taiwan. PLoS One. 2017;12(4):e0173843. doi:10.1371/journal.pone.0173843
12. Shardlow A, McIntyre NJ, Fluck RJ, McIntyre CW, Taal MW. Chronic kidney disease in primary care: outcomes after five years in a prospective cohort study. PLoS Med. 2016;13(9):e1002128. doi:10.1371/journal.pmed.1002128
13. Weldegiorgis M, de Zeeuw D, Li L, et al. Longitudinal estimated GFR trajectories in patients with and without type 2 diabetes and nephropathy. Am J Kidney Dis. 2018;71(1):91-101. doi:10.1053/j.ajkd.2017.08.010
14. Koraishy FM, Hooks-Anderson D, Salas J, Rauchman M, Scherrer JF. Fast GFR decline and progression to CKD among primary care patients with preserved GFR. Int Urol Nephrol. 2018;50(3):501-508. doi:10.1007/s11255-018-1805-1
15. Levey AS, Stevens LA, Schmid CH, et al; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604-612. doi:10.7326/0003-4819-150-9-200905050-00006. Published correction appears in Ann Intern Med. 2011;155(6):408.
16. Burke LG, Orav EJ, Zheng J, Jha AK. Healthy Days at home: a novel population-based outcome measure. Healthc (Amst). 2020;8(1):100378. doi:10.1016/j.hjdsi.2019.100378
17. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496-509. doi:10.1080/01621459.1999.10474144
18. Kaplan RM, Chambers DA, Glasgow RE. Big data and large sample size: a cautionary note on the potential for bias. Clin Transl Sci. 2014;7(4):342-346. doi:10.1111/cts.12178
19. Greene T, Teng C-C, Inker LA, et al. Utility and validity of estimated GFR-based surrogate time-to-event end points in CKD: a simulation study. Am J Kidney Dis. 2014;64(6):867-879. doi:10.1053/j.ajkd.2014.08.019
20. Stevens PE, Levin A; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825-830. doi:10.7326/0003-4819-158-11-201306040-00007.
21. Perkins RM, Bucaloiu ID, Kirchner HL, Ashouian N, Hartle JE, Yahya T. GFR decline and mortality risk among patients with chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(8):1879-1886. doi:10.2215/CJN.00470111
22. Guo Y, Cui L, Ye P, Li J, Wu S, Luo Y. Change of kidney function is associated with all-cause mortality and cardiovascular diseases: results from the Kailuan study. J Am Heart Assoc. 2018;7(21):e010596. doi:10.1161/JAHA.118.010596
23. Matsushita K, Selvin E, Bash LD, Franceschini N, Astor BC, Coresh J. Change in estimated GFR associates with coronary heart disease and mortality. J Am Soc Nephrol. 2009;20(12):2617-2624. doi:10.1681/ASN.2009010025
24. Mafham M, Emberson J, Landray MJ, Wen C-P, Baigent C. Estimated glomerular filtration rate and the risk of major vascular events and all-cause mortality: a meta-analysis. PLoS One. 2011;6(10):e25920. doi:10.1371/journal.pone.0025920
25. Golestaneh L, Alvarez PJ, Reaven NL, et al. All-cause costs increase exponentially with increased chronic kidney disease stage. Am J Manag Care. 2017;23(suppl 10):S163-S172.
26. Honeycutt AA, Segel JE, Zhuo X, Hoerger TJ, Imai K, Williams D. Medical costs of CKD in the Medicare population. J Am Soc Nephrol. 2013;24(9):1478-1483. doi:10.1681/ASN.2012040392
27. Manns B, Hemmelgarn B, Tonelli M, et al; Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease. The cost of care for people with chronic kidney disease. Can J Kidney Health Dis. 2019;6:2054358119835521. doi:10.1177/2054358119835521

