- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Food Impaction May Be Cause for Concern When Diagnosing EoE
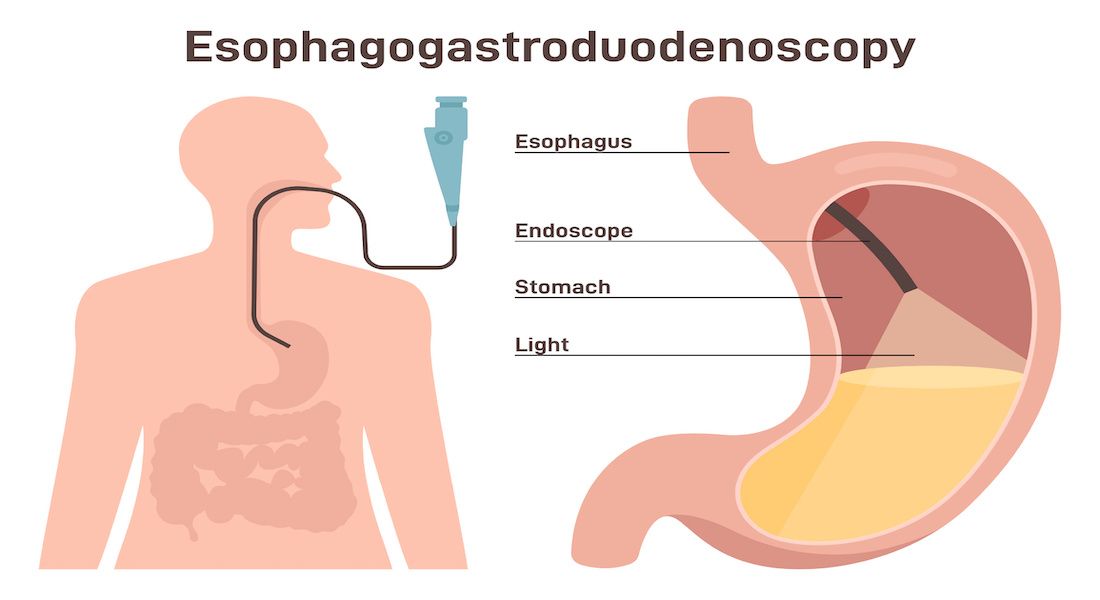
Outcomes of concern for this retrospective study were eosinophilic esophagitis (EOE) mucosal biopsies, EoE diagnosis, proton pump inhibitor initiation, and recommendations being followed for repeat esophagogastroduodenoscopy.
New research shows that esophageal food impactions (EFIs), which often precede a diagnosis of eosinophilic esophagitis (EoE), may not always lead to a diagnostic biopsy, thereby potentially delaying diagnosis and treatment of the inflammatory condition.
Data published in Journal of Clinical Medicine note that EFIs are the primary indication of EoE in up to 50% of patients who receive an EoE diagnosis, with past research showing the condition continues to increase on a global scale: approximately 17 cases per 100,000 individuals.1,2 Primary outcomes of concern for the present study were EoE mucosal biopsies, EoE diagnosis, proton pump inhibitor (PPI) initiation, and recommendations being followed for repeat esophagogastroduodenoscopy (EGD).
“Despite the relationship between EoE and EFI, there is no standard diagnostic and therapeutic practice for EoE at the time of EFI,” the authors wrote. “The 2018 AGREE Conference and 2020 AGA guidelines provide flexible recommendations that suggest obtaining esophageal mucosal biopsies from 2 or more esophageal levels upon suspicion of EoE, such as in the setting of an EFI.”
However, they added, data indicate just 34% of gastroenterologists follow through with biopsies following presentation of EFI.
Study data came from the University of Minnesota Medical Center, and they encompassed adult patients (N = 91; 56.04%, male patients; mean [SD] age, 50.30 [18.68] years; 92.31%, White patients) who had an endoscopically confirmed EFI between 2009 and 2020. Incomplete medical records and esophageal carcinoma precluded participation.
A scant 29% of the study population had an esophageal biopsy when they had their index EGD, the investigator highlighted, even though 41% were suspected of having EoE. And of this patient group, only 20% eventually underwent a biopsy. Younger patients (40 years and younger) were more likely to have a biopsy (P = .04).
Overall, 62% of biopsies came back with a diagnosis of EoE, with 16 patients receiving their diagnosis at the index EFI and 14 needing to undergo repeat EGDs (which produced 14 more diagnoses). Further, 55% of patients underwent a repeat EGD within 3 months of their initial EGD and 53% at some follow-up point.
The cause of EFI was not identified in 41 patients, and statistical differences in race and sex were not evident between those with and without an EoE diagnosis.
Age was, however, a significant factor is patient diagnosis. Patients shown to have EoE at their index EGD had a median (IQR) age of 39 (30-46) years compared with 59 (43-72) years for those who did not have EoE.
“ROC analysis identified the age of 51 or younger as predictive of EoE ([odds ratio], 14; 95% CI, 3.4%-50.0%; P < .0001),” the authors wrote.
For PPI therapy, 87% of patients were discharged with the treatment after their index EGD, while 92% of those suspected of having EoE vs 85% who were not (P = .05) were discharged on PPI treatment. Men were more likely to receive this treatment vs women, at 60% vs 40% (P = .05).
“While it is encouraging that most patients are discharged on a PPI, we identified several care gaps that resulted in diagnostic delays of EoE,” the study authors concluded. “These missed opportunities resulted in delayed diagnosis and unnecessary repeat EGDs, and overall poor patient care.”
They underscore that their findings echo previous research showing few gastroenterologists (one-third) perform esophageal biopsies when an EFI occurs, and they propose 2 potential reasons for this:
- Perceived potential for patient complications
- Therapeutic inertia
To make inroads in diagnosing EoE following an EFI, the study authors suggest potential biopsy guidelines be investigated and drawn up, as well as that health care providers receive more education on identifying care gaps and standardizing their management and treatment recommendations following an EFI.
Reference
1. Lee C, Sievers TJ, Vaughn BP. Diagnosis of eosinophilic esophagitis at the time of esophageal food impaction. J Clin Med. Published online May 31, 2023. doi:10.3390/jcm12113768
2. Murray FR, Kreienbühl A, Straumann A, Biedermann L, Shreiner P. Natural history of patients lost to follow-up after esophageal food impaction. Clin Gastroenterol Hepatol. Published online July 20, 2022. doi:10.1016/j.cgh.2022.07.00
