- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Fluvoxamine Fails to Shorten COVID-19 Symptom Duration in Mild to Moderate Outpatients
Study finds no benefit of fluvoxamine in shortening COVID-19 symptom duration among mild to moderate cases.
The effectiveness of repurposed medications for treating COVID-19 remains a critical area of investigation. A new analysis found that higher-dose fluvoxamine (Luvox), an antidepressant with anti-inflammatory properties, did not significantly reduce the time to sustained recovery compared with placebo, highlighting the need for continued research into alternative therapeutic options.1
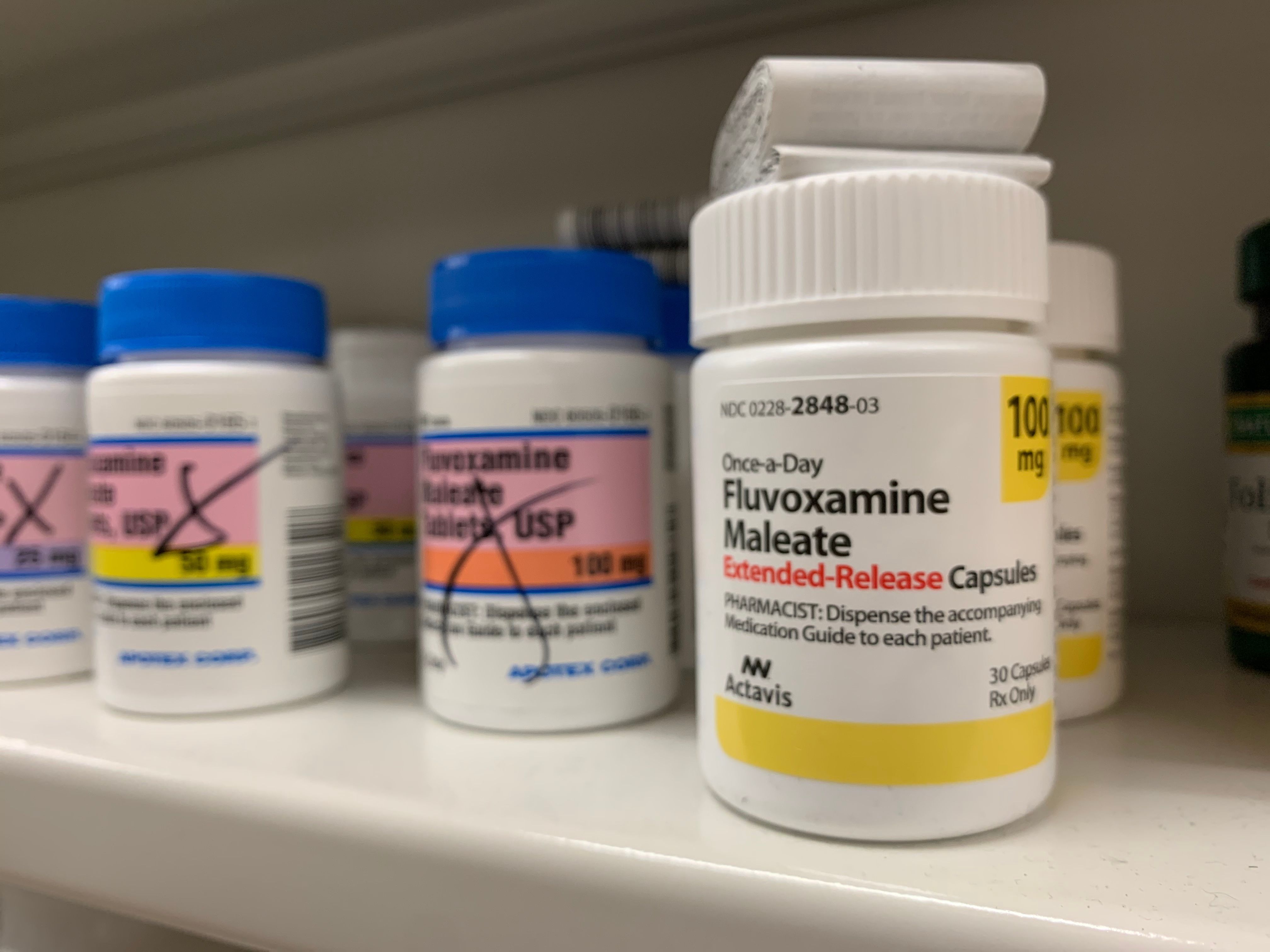
The researchers believe the study suggests no benefit of shortening COVID-19 symptom duration with fluvoxamine in this patient population. | Image credit: pureradiancecmp - stock.adobe.com
The double-blind, randomized, placebo-controlled trial is published in JAMA.
“ACTIV-6 is the only trial with a primary outcome of patient-reported sustained recovery and, in this trial of fluvoxamine 100 mg twice daily for 13 days, there was no evidence of benefit,” wrote the researchers of the study. “A secondary composite outcome of death or health care use (including urgent care or emergency department visits or hospitalizations) suggested one-third fewer events in the fluvoxamine group compared with placebo. This difference did not meet prespecified decision-making thresholds.”
Fluvoxamine belongs to a group of medicines known as selective serotonin reuptake inhibitors (SSRIs) and is used to treat obsessive-compulsive disorder (OCD).2 Moreover, fluvoxamine has been proposed to decrease the host inflammatory response and prevent progression to severe COVID-19.1
This trial aimed to incorporate diverse health care and community-based settings, including COVID-19 testing and treatment programs, to ensure broad participant inclusion. Eligibility criteria required participants to be 30 years or older with confirmed COVID-19 infection and at least 2 acute symptoms lasting no more than 7 days at the time of consent. Participants were randomized in a 1:1 ratio to receive either fluvoxamine (50 mg twice daily on day 1, followed by 100 mg twice daily for 12 days) or placebo, with study drugs delivered directly to participants' homes.
Primary outcome measures included the time to sustained recovery, defined as 3 consecutive symptom-free days, assessed through participant-reported data. Secondary outcomes included hospitalization, emergency visits, or death, as well as COVID-19 clinical progression scores and time spent unwell.
The trial enrolled 1208 participants, with 1175 included in the modified intention-to-treat analysis cohort after excluding those who did not receive the study drug within 7 days of randomization. Participants were randomized to receive fluvoxamine (n = 589) or placebo (n = 586). Most participants were White (72.7%), and 45.5% identified as Hispanic or Latino. Common comorbidities included obesity (36.1%) and hypertension (25.8%), and 76.8% had received at least 2 COVID-19 vaccine doses. The median (IQR) time to study drug delivery was 5 (4-7) days from symptom onset.
The primary outcome showed no significant difference between groups, with a median (IQR) recovery time of 10 (95% CI, 10-11) days in both arms (HR, 0.99; 95% credible interval [CrI], 0.89-1.09; posterior probability of benefit = 0.4). Secondary outcomes revealed low event rates, with no deaths and minimal hospitalizations in both groups.
Furthermore, the health care utilization composite outcome showed no significant difference (HR, 0.69; 95% CrI, 0.27-1.21; posterior probability of efficacy = 0.86). Measures of activity limitation and time spent unwell were also comparable, indicating no clinically meaningful benefit of fluvoxamine in this population.
However, the researchers acknowledged some limitations. First, the low incidence of clinical events, reflective of the evolving pandemic and population enrolled, limited the ability to assess treatment effects on clinical outcomes. Additionally, the remote, decentralized design, while increasing accessibility, introduced logistical challenges.
Despite these limitations, the researchers believe the study suggests no benefit of shortening COVID-19 symptom duration with fluvoxamine in this patient population.
“Although one-third fewer health care use events occurred in the fluvoxamine intervention group, the difference did not meet prespecified decision thresholds for concluding a treatment effect,” wrote the researchers.
References
1. Stewart TG, Rebolledo PA, Mourad A, et al. Higher-dose fluvoxamine and time to sustained recovery in outpatients with COVID-19: The ACTIV-6 Randomized Clinical Trial. JAMA. 2023;330(24):2354–2363. doi:10.1001/jama.2023.23363
2. Fluvoxamine (oral route). Mayo Clinic. Accessed December 6, 2024. https://www.mayoclinic.org/drugs-supplements/fluvoxamine-oral-route/description/drg-20066874.
The Breakdown: Breast Cancer Research Awareness Day
August 19th 2025Breast cancer is the second most common cancer among women and the second leading cause of cancer-related deaths among women in the US. In light of Breast Cancer Research Awareness Day, The American Journal of Managed Care® breaks down the most recent advancements in breast cancer prevention, screening, and therapies.
Listen
