- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
FDA Approves Exagamglogene Autotemcel, First CRISPR Gene-Editing Therapy for SCD
The FDA has approved a gene-editing therapy for sickle cell disease (SCD) for the first time.
The FDA has approved the first clustered regularly interspaced short palindromic repeats (CRISPR) gene-editing therapy for use in patients with sickle cell disease (SCD). Exagamglogene autotemcel (exa-cel; Casgevy), developed by Vertex Pharmaceuticals in collaboration with CRISPR Therapeutics, is aimed at reducing or eliminating painful vaso-occlusive crises (VOCs) in patients with SCD.
“Sickle cell disease is a rare, debilitating and life-threatening blood disorder with significant unmet need, and we are excited to advance the field especially for individuals whose lives have been severely disrupted by the disease by approving 2 cell-based gene therapies today,” Nicole Verdun, MD, director of the Office of Therapeutic Products within the FDA’s Center for Biologics Evaluation and Research, said in a press release.1
This decision from the FDA comes after the committee accepted a biologics license application in June.2 The application contained data from trials evaluating exa-cel in patients with SCD and transfusion-dependent β-thalassemia (TDT). The treatment alters hematopoietic stem cells from a patient to produce more fetal hemoglobin F (HbF) in red blood cells. This increase in HbF could help to eliminate or reduce the amount of VOCs in patients with SCD, as well as reduce the transfusion requirements in patients with TDT.
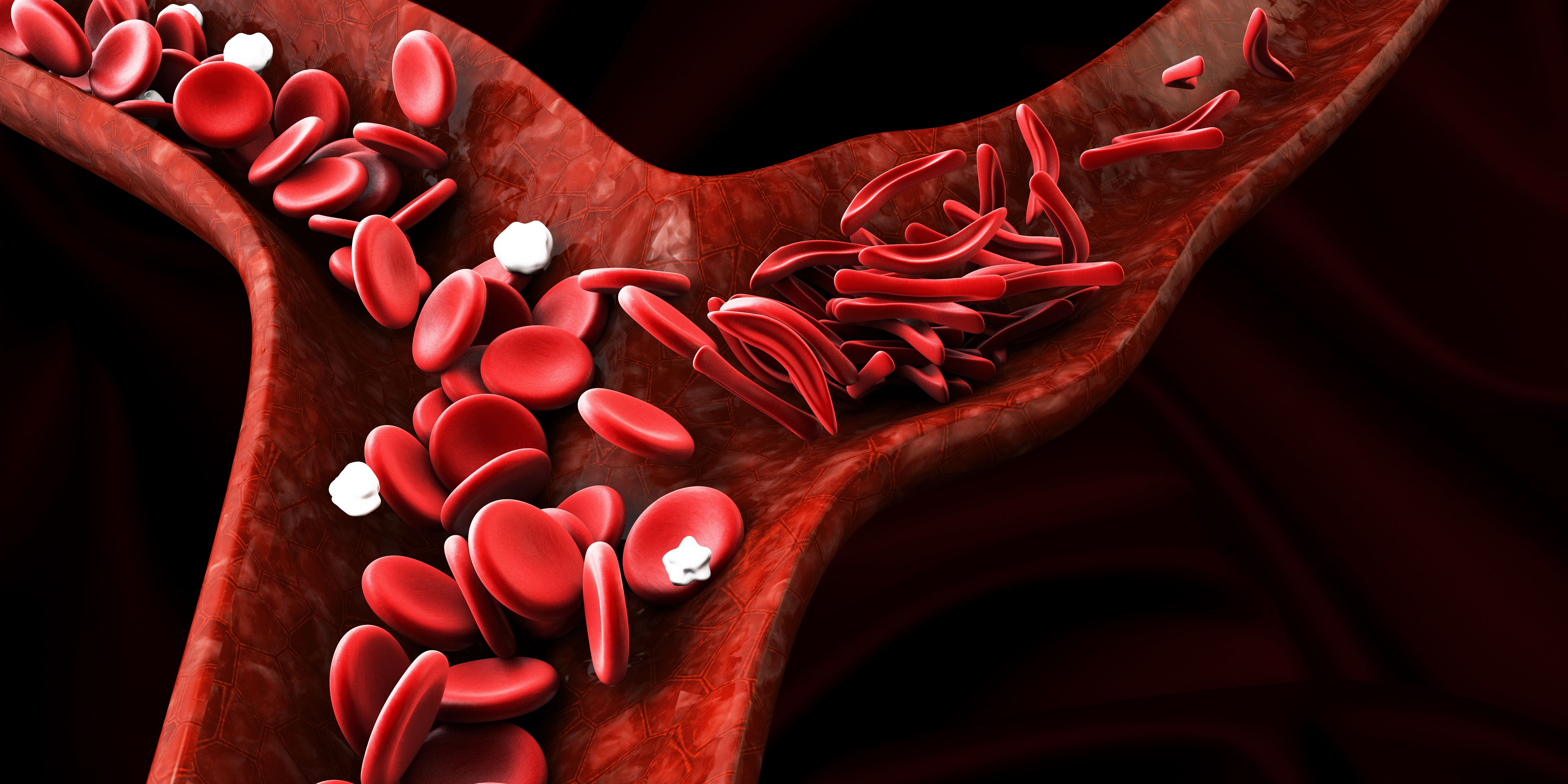
Sickle cell anemia, showing blood vessel with normal and deformated crescent | Image credit: tussik - stock.adobe.com
Several trials are looking into the effectiveness of exa-cel in these populations. For example, CLIMB-111 and CLIMB-121 are ongoing phase 1/2/3 open-label trials evaluating the safety of exa-cel in patients aged 12 to 35 years and will continue into the CLIMB-131 long-term trial. Although the trials are still ongoing, results from the early stages of these trials had been presented at the European Hematology Association Congress in 2022.3
Included in the CLIMB-111, CLIMB-121, and CLIMB-131 trials were 75 patients, 44 of whom had TDT and 31 who had SCD. The follow-up ranged from 1.2 to 37.2 months. After exa-cel infusion, 42 of the 44 patients with TDT no longer needed transfusions after follow-up. The other 2 patients had 75% and 89% reductions in transfusions. HbF was also increased in patients with TDT after infusion, with an increase to more than 11 g/dL by the third month.
Similar results were found in patients with SCD in the same study, with all patients with SCD who had a mean of 3.9 VOCs per year having full elimination of VOCs after exa-cel infusion. HbF also made up about 40% of total Hb by month 4. The follow-up period for this was slightly different at 2.0 to 32.3 months. All results for patients with TDT and SCD were maintained after months 3 and 4, respectively.
In this study, serious adverse events were reported in 2 patients with TDT that were related to exa-cel. These included acute respiratory distress syndrome, headache, hemophagocytic lymphohistiocytosis, and idiopathic pneumonia syndrome in 1 patient; delayed neutrophil engraftment and thrombocytopenia were reported in the other patient. All adverse events were resolved.
The study that formed the basis of the FDA approval evaluated 31 patients with a history of at least 2 severe VOCs in the previous 2 years who had received exa-cel and had sufficient follow-up time of 24 months. The ongoing single-arm, multicenter study found that 93.5% of patients had achieved freedom from severe VOCs for at least 12 consecutive months. Engraftment was successful in all patients.
Low levels of platelets and white blood cells, abdominal pain, mouth sores, nausea, musculoskeletal pain, headache, vomiting, febrile neutropenia, and itching were among the other adverse events reported.
Simultaneous with the exa-cel approval, the FDA also approved a separate cell-based gene therapy, lovotibeglogene autotemcel (Lyfgenia), manufactured by bluebird bio, which uses a lentiviral vector to genetically modify the blood stem cells of patients with SCD to produce HbAT87Q, a form of hemoglobin that can reduce the risk of VOCs.1
References
- FDA approves first gene therapies to treat patients with sickle cell disease. News release. FDA. December 8, 2023. Accessed December 8, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease
- FDA accepts biologics license applications for exagamglogene atutemcel (exa-cel) for severe sickle cell disease and transfusion-dependent beta thalassemia. News release. Vertex Pharmaceuticals Incorporated. June 8, 2023. Accessed December 6, 2023. https://www.businesswire.com/news/home/20230608005819/en/FDA-Accepts-Biologics-License-Applications-for-exagamglogene-autotemcel-exa-cel-for-Severe-Sickle-Cell-Disease-and-Transfusion-Dependent-Beta-Thalassemia
- Vertex and CRISPR Therapeutics present new data on more patients with longer follow-up treated with exagamglogene autotemcel (exa-cel) at the 2022 European Hematology Association (EHA) Congress. News release. CRISPR Therapeutics. June 11, 2022. Accessed December 8, 2023. https://crisprtx.com/about-us/press-releases-and-presentations/vertex-and-crispr-therapeutics-present-new-data-on-more-patients-with-longer-follow-up-treated-with-exagamglogene-autotemcel-exa-cel-at-the-2022-european-hematology-association-eha-congress
Knowledge Gaps Persist in Patient Understanding of Skin Cancer–Related Terms
January 13th 2026On average, patients with multiple prior dermatology visits still scored below 75% when identifying common skin cancer terms, underscoring the need for clearer patient-physician communication.
Read More
