- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Enhancing Retinal Disease Outcomes With Anti-VEGF Therapies
New anti–vascular endothelial growth factor (VEGF) therapies are improving retinal disease management by providing patients with more treatment options, optimizing timing, and introducing innovative administration methods.
Several ranibizumab, bevacizumab, and aflibercept biosimilars have been approved by the FDA. | svetazi - adobe.stock.com
Advancements in anti–vascular endothelial growth factor (VEGF) therapy are transforming the management of retinal diseases by improving patient outcomes and reducing treatment burden, according to Anthony DeWilde, OD, at Southeastern Educational Congress of Optometry (SECO) 2025.1
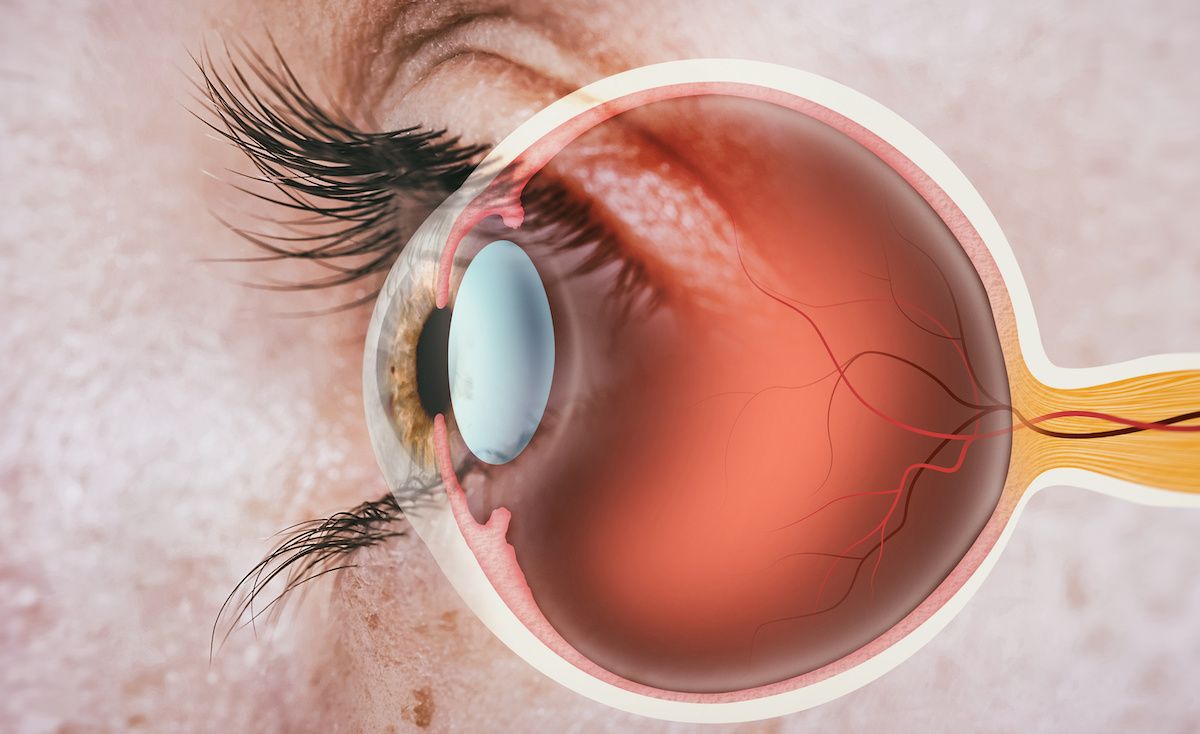
The comprehensive session on anti-VEGF treatment explored the role these products play in managing retinal diseases. He explained the critical role of VEGF in embryonic development and how it can get out of control in conditions like age-related macular degeneration (AMD), retinal vein occlusions, and diabetic retinopathy, leading to neovascularization, or the creation of new blood vessels in the eye.2
“Neovascularization sounds good. We talk to patients…who will say, ‘The reason you're having these issues is that there's a lack of blood flow to certain parts of your eye, and it stands to reason that new blood vessels would help out, right?’ But the problem is not so much the new blood vessels; it's where the new blood vessels are growing and the fragility of those blood vessels,” he explained.1
When discussing neovascularization, DeWilde emphasized the fragility of new blood vessels and the significance of their location in disease progression. He introduced key topics, including neovascular membranes, macular edema, and diabetic retinopathy, using a case study of a 75-year-old patient with blurry vision to illustrate the diagnostic process.
Through optical coherence tomography (OCT) imaging and fundoscopic evaluation, he demonstrated how different types of fluid accumulation in the retina guide treatment decisions. He underscored the necessity of OCT in diagnosing neovascular membranes, warning that up to half of cases could be missed without it. The session also highlighted the complementary role of stereopsis and fundoscopic evaluation in ensuring accurate diagnosis.
DeWilde then reviewed historical and current treatment options for neovascular AMD, transitioning from early laser therapy and visudyne to modern anti-VEGF therapies like ranibizumab (Lucentis), bevacizumab (Avastin), and brolucizumab-dbll (Beovu) and newer products like Susvimo, an ocular implant utilizing ranibizumab. He explained that 90% of patients maintain visual acuity with these treatments, emphasizing that initial acuity plays a significant role in long-term outcomes.
Before diving into anti-VEGF therapies for retinal vein occlusion, DeWilde clarified the difference between branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO), highlighting the risks of neovascularization and macular edema in BRVO and the greater treatment challenges presented by CRVO due to more extensive edema. He emphasized the clinical benefits of anti-VEGF therapy in these patients and the importance of early intervention and proactive monitoring.
“If you see a patient who has a branch retinal vein occlusion and there's no neovascularization or macular edema, you don't just say, ‘OK, good luck! I'll see you next year.’ You say, ‘Let's follow up about this in a few weeks to see if neovascularization or macular edema develops.’”
Turning to diabetic retinopathy, DeWilde presented a case study of a patient with diabetes and hypertension to illustrate the importance of monitoring for macular edema and neovascularization. He detailed the vision-threatening complications of diabetic retinopathy, including neovascular glaucoma and traction retinal detachment.
The criteria for referring patients for anti-VEGF therapy, particularly those with high-risk neovascularization and center-involved diabetic macular edema, were discussed alongside the benefits and limitations of anti-VEGF and laser therapy. For proliferative diabetic retinopathy, DeWilde reviewed clinical trial data comparing anti-VEGF therapy with panretinal photocoagulation (PRP), noting similar visual acuity outcomes at 2 and 5 years, highlighting anti-VEGF’s potential to reduce PRP-related complications.
Finally, DeWilde explored future developments in anti-VEGF treatment, including biosimilars, implantable devices like Susvimo, and potential new delivery methods such as eye drops. He emphasized the need for continued innovation to enhance patient outcomes as well as continued care for patients even after they receive anti-VEGF therapy.
“Despite our best efforts and our best anti-VEGF today, low vision still plays a very vital role because even with our best treatment available, these patients will often still need low vision rehabilitation in addition to the anti-VEGF treatment they may receive.”
References
1. DeWilde A. Anti-VEGF & the eye: past, present, & future. Presented at: SECO 2025; February 26-March 2, 2025; Atlanta, GA.
2. Neovascularization of the eye. Cleveland Clinic. Updated September 7, 2022. Accessed February 28, 2025. https://my.clevelandclinic.org/health/diseases/24131-neovascularization-of-the-eye
The Importance of Examining and Preventing Atrial Fibrillation
August 29th 2023At this year’s American Society for Preventive Cardiology Congress on CVD Prevention, Emelia J. Benjamin, MD, ScM, delivered the Honorary Fellow Award Lecture, “The Imperative to Focus on the Prevention of Atrial Fibrillation,” as the recipient of this year’s Honorary Fellow of the American Society for Preventive Cardiology award.
Listen
Promoting Equity in Public Health: Policy, Investment, and Community Engagement Solutions
June 28th 2022On this episode of Managed Care Cast, we speak with Georges C. Benjamin, MD, executive director of the American Public Health Association, on the core takeaways of his keynote session at AHIP 2022 on public health policy and other solutions to promote equitable health and well-being.
Listen
