- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Emerging Mechanisms in the Management of Heart Failure With Reduced Ejection Fraction
Given the substantial economic burden of heart failure (HF), particularly HF with reduced ejection fraction (HFrEF), understanding its underlying neurohormonal mechanisms is critical toward determining optimal treatment regimens for patients. Several classes of pharmacologic interventions are available for the treatment of HF, each with unique mechanisms reflecting the complex pathophysiology of the disease. Recent clinical trials, such as PARADIGM-HF, DAPA-HF, and VICTORIA, have shed new light on worsening HF and demonstrated the potential of several emerging agents and mechanisms. This article reviews recent trial data that are shaping the treatment spectrum and the role of neurohormonal activation in the evolving therapeutic landscape.
Pathophysiology and Neurohormonal Activation
HF pathophysiology is complex and involves the activation of several neurohormonal mechanisms designed to compensate for a poorly functioning heart pump and the accompanying decrease in cardiac output.1-3 These compensatory mechanisms are helpful in normal physiological conditions, but their chronic activation in the setting of HF becomes maladaptive and problematic.2,3 There are 3 main neurohormonal systems that become activated in HF and play a role in the pathophysiology of disease: the sympathetic nervous system (SNS),the renin-angiotensin-aldosterone system (RAAS),and the natriuretic peptide (NP) system.1
In the setting of a failing heart pump, the SNS attempts to maintain cardiac output and blood perfusion to organs by releasing catecholamines (epinephrine and norepinephrine), which make the heart pump harder and faster (positive inotropic and chronotropic effects, respectively) and cause widespread peripheral vasoconstriction to maintain blood pressure.1,2 The RAAS attempts to increase blood pressure by both vasoconstriction and by increasing blood volume.1,2 Renin is released, which cleaves angiotensinogen into angiotensin I. Angiotensin I is subsequently converted to angiotensin II by the angiotensin-converting enzyme (ACE).1,2 Angiotensin II is a potent vasoconstrictor and also activates aldosterone synthesis and releases from the adrenal glands.1,2 Aldosterone acts at mineralocorticoid receptors in the kidney tubules to increase sodium and water retention; this action increases blood volume.1,2
The NP system attempts to counteract the vasoconstriction and the fluid retention brought about by the SNS and RAAS by releasing the natriuretic peptides ANP and BNP.1,2 These hormonal peptides bring about natriuresis (excretion of sodium and water in the urine), vasodilation, and inhibition of aldosterone synthesis, as well as several cardioprotective mechanisms.1 The NP is successful at compensating for the deleterious effects of the SNS and RAAS for a time. However, as HF progresses, the actions of the SNS and RAAS overwhelm the NP system’s beneficial and protective effects, andthe imbalance that ensues brings about symptomatic decompensation.1
One of the natriuretic peptides and its inactive fragment (BNP and NT-proBNP [N-terminal pro-B-type natriuretic peptide, respectively]) have become useful prognostic biomarkers in HF.1,2,4,5 The precursor to both BNP and NT-proBNP is the peptide proBNP108, which is released by cardiomyocytes in response to myocardial stretch secondary to cardiac congestion.4 During processing, proBNP108 is cleaved into BNP (active form) and an N-terminus (or amino-terminus) fragment, NT-proBNP.4 Levels of these hormones go up with HF worsening and go down when HF is stable.4,6 Higher levels are associated with higher risk for poor clinical outcomes, including hospital readmission and mortality.5
Central to HF therapy management is the targeting of 1 or all of these maladapted neurohormonal systems and/or their deleterious effects.1 Pharmaceutical agents that directly suppress the SNS and/or the RAAS; ameliorate fluid retention, vasoconstriction, and/or rapid heart rate; and/or leverage the beneficial effects of the NP system, are potentially advantageous in the setting of HF management.1,7
Guideline-Based Approaches for HFrEF
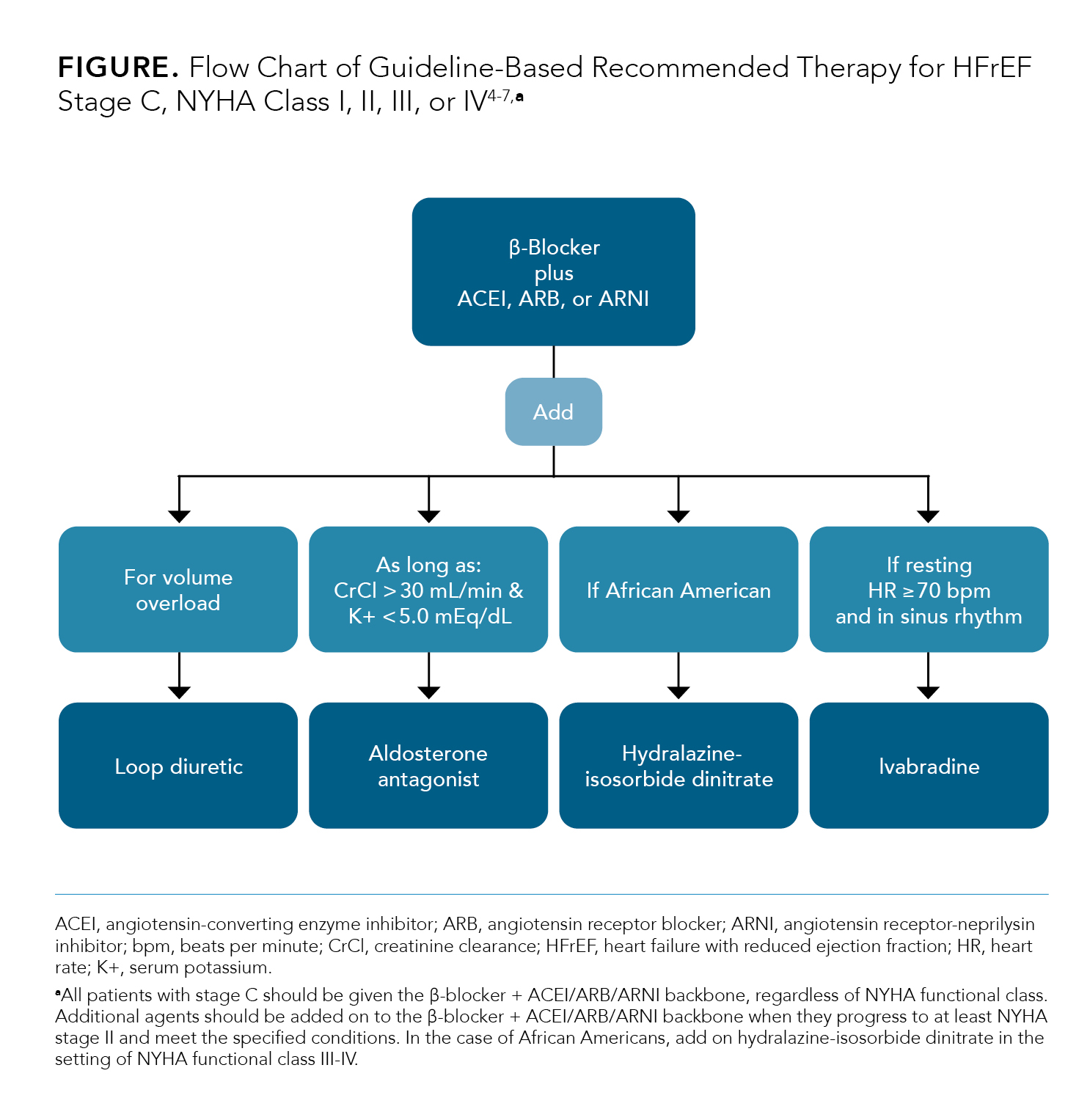
Before examining newer therapies/mechanisms, it is important to review current recommendations for the treatment of HF. The American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines recommend a β-blocker plus either an angiotensin-converting enzyme inhibitor (ACEI) or an angiotensin receptor blocker (ARB) as the backbone of therapy to reduce morbidity and mortality.4,7 Added to this backbone are (1) an aldosterone antagonist, provided that the patient’s kidney function and potassium levels are within the acceptable range (creatinine clearance > 30 mL/min and serum potassium (K+) < 5.0 mEq/dL, respectively); (2) hydralazine and isosorbide dinitrate if the patient is African American; and (3) a loop diuretic in thesetting of volume overload.4 The set of agents recommended by evidence-based practice guidelines for treating HFrEF, along with the system or effect that they target, are provided in Table 1.3-9
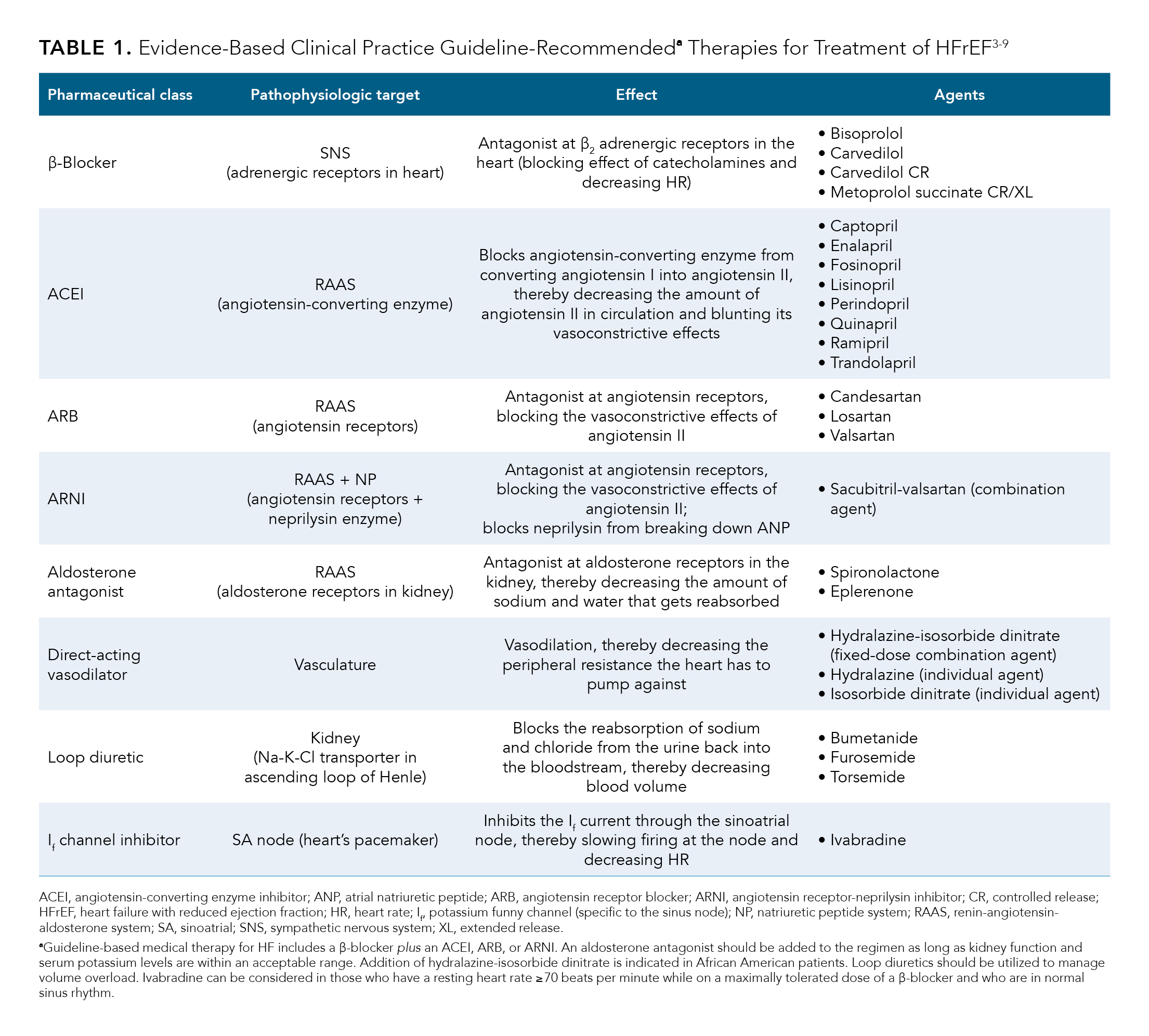
Since the publication of the 2013 ACCF/AHA guideline document, several novel therapies have been added to the recommendations based on key clinical trials. These new recommendations were included in the 2017 ACCF/AHA focused guideline update and include the addition of ivabradine, an agent that functions at the sinoatrial node to reduce heart rate, and sacubitril-valsartan, an ARB combined with a neprilysin inhibitor (ARNI).5 Guideline-based therapy recommendations for managing HFrEF are summarized in the Figure.4-7
Since the publication of the guidelines, new results from trials have pointed to new directions in care. The results of the SHIFT trial showed that adding ivabradine to a background of guideline-directed medical therapy in patients who had a persistently elevated resting heart rate significantly lowered HF-related hospitalizations.5,7,10 Ivabradine reduces heart rate without concomitantly lowering blood pressure by selectively inhibiting the potassium funny current (If) in the sinoatrial node.5,7 Candidates for ivabradine are those already on a maximally tolerated dose of a β-blocker and in sinus rhythm with a resting heart rate of at least 70 bpm.5-7 For patients who need resting heart rate control but who are not in sinus rhythm (ie, in atrial fibrillation), digoxin can be considered, although this drug has fallen out of favor in recent years because of its high risk for various drug toxicities, especially among the elderly population.3,4,6
Exploring New Mechanisms: PARADIGM-HF, DAPA-HF, and VICTORIA
In addition to the SHIFT trial, several other key trials have signaled new directions in the management of HRrEF, including PARADIGM-HF, DAPA-HF, and VICTORIA.11-15
PARADIGM-HF. The beneficial effects of sacubitril-valsartan monotherapy were demonstrated in PARADIGM-HF, a randomized, double-blind, parallel group, active-controlled, 2-arm, event-driven trial comparing enalapril (an ACEI) with sacubitril-valsartan in patients with chronic HFrEF.16 The primary efficacy outcome in this trial was a composite of death from cardiovascular causes or a first hospitalization for HF.13 Over 8000 patients were evaluated (4187 in the sacubitril-valsartan arm and 4212 in the enalapril arm), and the mean left ventricular ejection fraction at baseline across both groups was approximately 29%.13,14 Other enalapril baseline characteristics to note were that approximately 5% had symptoms consistent with NYHA class I, 70% with class II, 25% with class III, and only 1% with class IV.13,14 Approximately 37% had atrial fibrillation/flutter, 15% had an implantable cardioverter-defibrillator (ICD), and 7% had a biventricular pacemaker (ie, were receiving cardiac resynchronization therapy) at baseline.13,14 The median NT-proBNP level at baseline across both groups was 1608 pg/mL.13,14 Baseline kidney function, as measured by the mean estimated glomerular filtration rate (eGFR) was 68 mL/min/1.73 m2 across both groups.13,14
The proportion of patients who had a primary outcome event (either death from cardiovascular causes or a first hospitalization for HF) was significantly lower in the sacubitril-valsartan arm compared with the enalapril arm, with a hazard ratio of 0.80 and a 95% CI of 0.73 to 0.87.13 Based on the reduction of cardiovascular death or first hospitalization associated with sacubitril-valsartan compared with enalapril in the PARADIGM-HF trial, the 2017 ACCF/AHA focused guideline update recommends replacing an ACEI or an ARB with an ARNI for patients who are already tolerating an ACEI or an ARB in order to further reduce morbidity and mortality.5,7 Sacubitril-valsartan carries an FDA-approved indication for reducing the risk of cardiovascular death and hospitalization for HF in adult patients with chronic HFrEF, NYHA classes II to IV.17
DAPA-HF. Another new mechanism of action that is used to treat HF is dapagliflozin, a sodium-glucose cotransporter 2 (SGLT-2) inhibitor that blocks the reuptake of glucose within the proximal tubule of the kidney.18 The increased amount of glucose in the urine creates an osmotic gradient where water is also pulled into the urine, creating a diuretic effect.18,19 Dapagliflozin was originally approved for use in adults with type 2 diabetes (T2D) as an agent to improve glycemic control.18 However, based on the results of DECLARE-TIMI 58 (2018), DAPA-HF (2019), and other recent trials, it gained FDA approval for an expanded set of indications, including (1) reducing the risk of cardiovascular death among adult patients with T2D who have established cardiovascular disease or multiple cardiovascular risk factors and (2) reducing the risk of cardiovascular death and hospitalization for HF in adults with HFrEF.12,18,19 Where the DECLARE-TIMI 58 trial showed that dapagliflozin significantly reduced the risk of a first hospitalization for HF or cardiovascular death in patients with T2D compared with placebo,19 the DAPA-HF evaluated the ability of dapagliflozin to prevent HF worsening, as defined by the reduction in HF hospitalizations or outpatient visits, in a more general HF population regardless of their T2D status.12
DAPA-HF, a phase 3, randomized, placebo-controlled trial, compared dapagliflozin with placebo to evaluate a primary composite outcome of worsening HF or death from cardiovascular causes.12 In the trial, a worsening event was defined as an unplanned HF-related hospitalization or an outpatient visit involving urgent use of intravenous (IV) diuretics.12 Over 4500 patients were evaluated (n = 2373 in the dapagliflozin arm and n = 2371 in the placebo arm), and the mean left ventricular ejection fraction at baseline across both groups was approximately 31%.12 Other baseline characteristics to note were that there were no patients in this trial who had symptoms consistent with NYHA functional class I, but instead were all classified as NYHA II, III, or IV (approximately 67%, 32%, and 1%, respectively).12 Approximately 38% had atrial fibrillation, approximately 26% had an ICD, and about 7% had a biventricular pacemaker (ie, were receiving cardiac resynchronization therapy).12 The median NT-proBNP level at baseline was 1428 pg/mL in the dapagliflozin group and 1446 pg/mL in the placebo group.12 Baseline kidney function, as measured by the mean eGFR was approximately 66 mL/min/1.73 m2 across both groups.12
The proportion of patients who experienced a primary outcome event was significantly lower in the dapagliflozin arm compared with the placebo arm, with a hazard ratio of 0.74 and a 95% CI of 0.65 to 0.85.12 Thus, dapagliflozin lowered the risk of a primary event by approximately 26% compared with placebo.
VICTORIA. One of the most recent trials to explore new mechanisms in the treatment of HF is the phase 3 VICTORIA trial, a randomized, double-blind, placebo-controlled trial that evaluated the oral soluble guanylate cyclase stimulator, vericiguat, against placebo.11
Stimulating the nitric oxide (NO)–soluble guanylate cyclase (sGC)–cyclic guanosine monophosphate pathway (GMP) is a novel approach to the treatment of HF and addresses a deficit in this pathway likely to be present in patients with worsening HFrEF as seen previously in the SOCRATES-REDUCED trial.20 During certain physiologic stimuli, NO is generated in endothelial cells and diffuses into vascular and cardiac muscle cells. Once inside the cell, NO binds to its intracellular receptor, sGC, stimulating it to generate cGMP. The production of cGMP exerts vasodilatory, antifibrotic, and cardioprotective effects.21
Reduced bioavailability of NO is thought to occur in the setting of HF, resulting in a relative sGC deficiency, as well as a reduction in cGMP and its beneficial effects. A reduced level of endogenous NO and sGC activity—and the corresponding decline in cGMP synthesis—has been correlated with cardiomyocyte stiffness, interstitial fibrosis, myocardial dysfunction, and coronary microvascular dysfunction, all things that can contribute to worsening HF. By directly stimulating sGC in a manner similar to, but independent of, endogenous NO, it is hypothesized that cGMP levels will increase and protective effects can be restored.11,21
In addition to having a diagnosis of chronic HFrEF, like the DAPA-HF and PARADIGM-HF trials, patients enrolled in the VICTORIA trial had to have evidence of worsening HF, which is a feature that sets it apart from the aforementioned trials.11-13 Worsening HF was defined as a previous HF hospitalization within 6 months prior to randomization or outpatient IV diuretic treatment for HF without hospitalization within 3 months before randomization.11 The primary efficacy outcome in the VICTORIA trial was a composite of first hospitalization for HF or death from cardiovascular causes.11
Over 5000 patients were evaluated (2526 in the vericiguat arm and 2524 in the placebo arm), and the mean left ventricular ejection fraction at baseline across both groups was approximately 29%.11 Other baseline characteristics to note were that the distribution of patients who had symptoms consistent with NYHA functional classes I, II, III, and IV were < 0.1%, 59.0%, 39.7%, and 1.3%, respectively.11 Approximately 45% had atrial fibrillation, 28% had an ICD, and 15% had a biventricular pacemaker (ie, were receiving cardiac resynchronization therapy).11 The median NT-proBNP level at baseline across both groups was 2816 pg/mL.11Baseline kidney function, as measured by the mean eGFR was approximately 62 mL/min/1.73 m2 across both groups.11
The proportion of patients who experienced a primary outcome event was significantly lower in the vericiguat arm compared with the placebo arm, with a hazard ratio of 0.90 and a 95% CI of 0.82 to 0.98.11 Thus, vericiguat lowered the risk of a primary event by 10% compared with placebo.
Trial Synthesis
The results of the VICTORIA, DAPA-HF, and PARADIGM-HF trials each present the clinician with drug treatment options that may augment the standard of care for patients with chronic HFrEF. Choosing which agent to utilize on top of a background of guideline-directed medical therapy becomes an important decision point, especially in the setting of worsening HF, where care has already been
optimized, yet patients are still experiencing clinical declines. Therefore, it is helpful to examine the baseline characteristics (Table 2a11-15) and efficacy outcomes (Table 2b11-13,15,22) of each of the trials against one another.
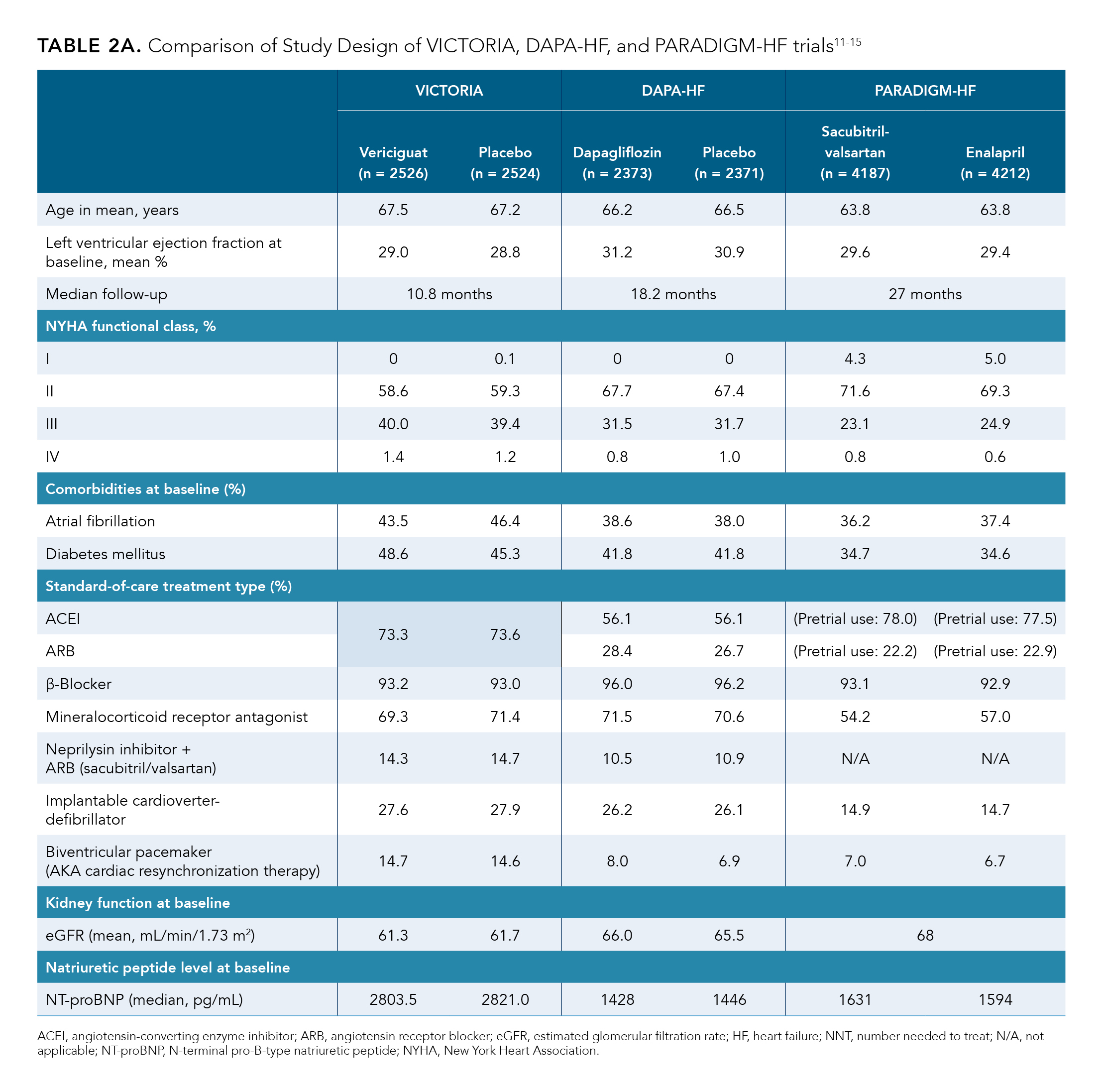
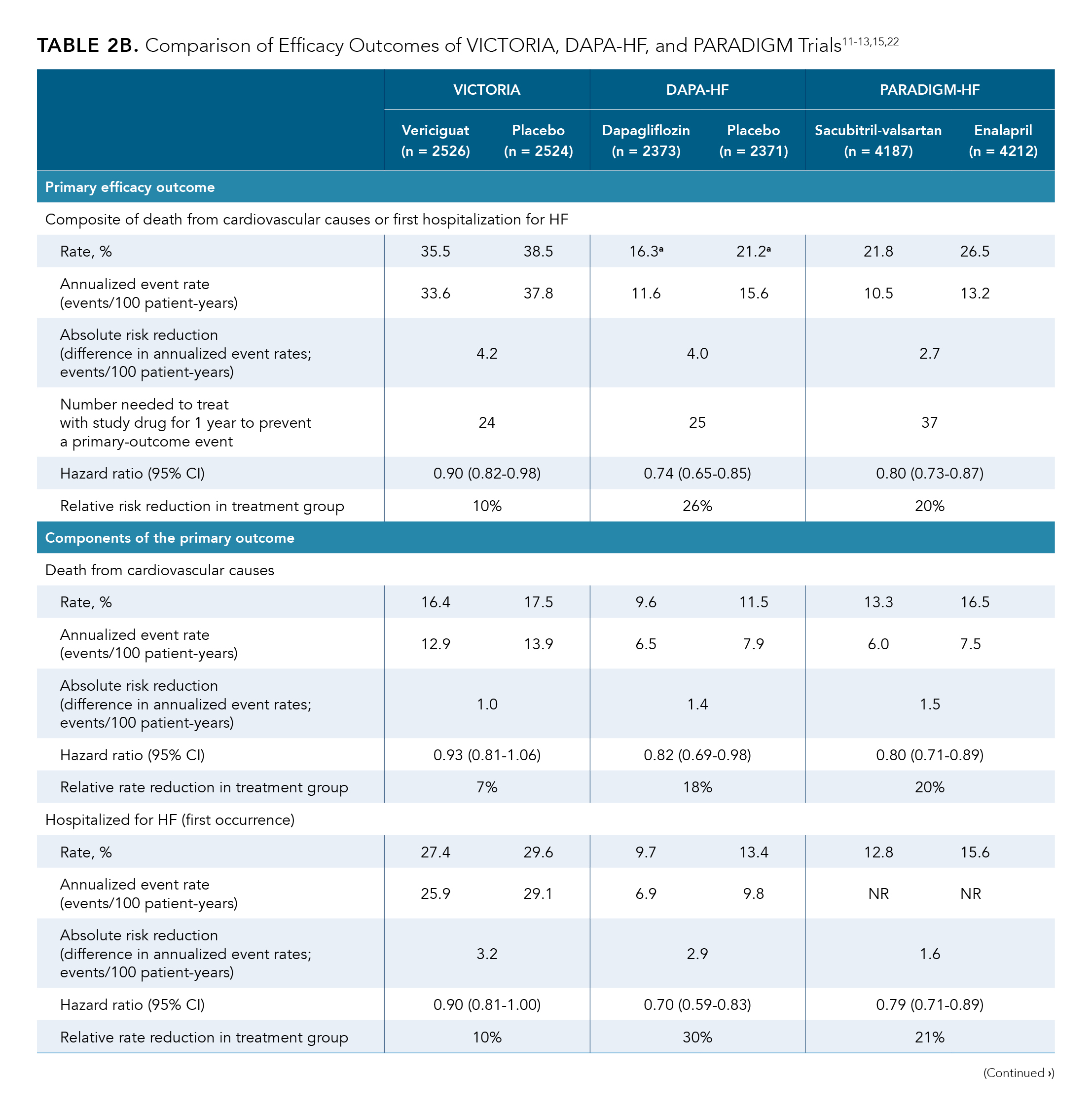
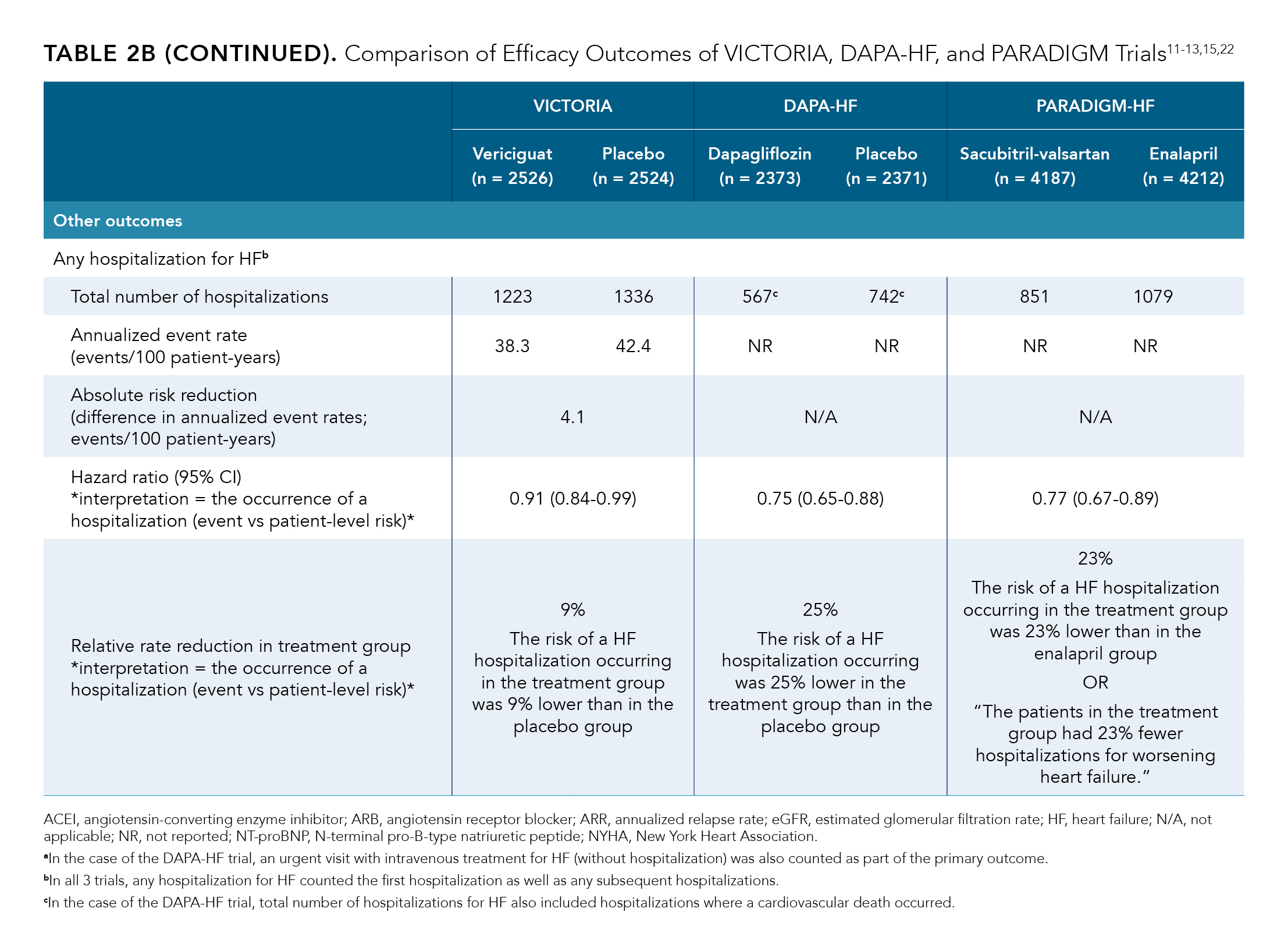
Notably, VICTORIA evaluated a subset of patients whose baseline clinical characteristics were worse than those evaluated in both the DAPA-HF and PARADIGM-HF trials, as evidenced by an inclusion criteria requirement of an HF hospitalization or outpatient HF treatment within within the past 3 to 6 months, a higher proportion of patients with NYHA functional class III or IV, a higher proportion of patients with a biventricular pacemaker, and a median NT-proBNP level that was approximately twice as high. A sicker patient population in VICTORIA was also manifested in its shorter trial duration; thus, VICTORIA accumulated more primary outcome events within a median follow-up time of approximately 11 months (35.5% and 38.5%, vericiguat and placebo, respectively), compared with 18 months in DAPA-HF (16.3% and 21.1%, dapagliflozin and placebo, respectively) and 27 months in PARADIGM-HF (21.8% and 26.5%, sacubitril-valsartan and enalapril, respectively).11-13,15,22
In addition, although both DAPA-HF and PARADIGM-HF had greater reductions in relative risk of their primary outcomes compared with the VICTORIA trial (26% and 20% vs 10%, respectively), when reductions in absolute risks (annualized event rates per 100 patient-years) are compared, the results appear more similar (a 4.2, 4.0, and 2.7 reduction in absolute risk for VICTORIA, DAPA-HF, and PARADIGM-HF, respectively).11-14, 16
Future Directions
Evidence-based practice guideline recommendations for these patients are general in nature and focus on optimizing chronic HF therapy.23 They include (1) escalation of current therapies, diuretics, and/or other decongestion strategies; (2) hemodynamic monitoring with right heart catheterization; (3) IV inotropes or pressors; (4) percutaneous or durable mechanical support devices; (5) long-term advanced treatment strategies, such as cardiac transplant; (6) reevaluation of comorbidities and alternative diagnosis; and (7) palliative care.6 To date, there is no particular agent recommended in the guidelines for improving outcomes in the subset of patients with worsening HF.23
Despite a variety of treatment options, unmet needs remain for patients with worsening HF who are already on standard of care, as evidenced by the 1-year mortality rate of 20% to 30% following a hospitalization.6 Arguably, there is a need to reduce the residual risk for patients with worsening HF who have a history of hospitalization(s) and who are already on guideline-based standard of care (β-blocker plus an ACEI, ARB, or ARNI).23
The findings of VICTORIA, DAPA-HF, and PARADIGM-HF suggest new directions in the management of HF to reducing risk of cardiovascular events. As the field advances, it will become increasingly important for clinical trials to investigate patients with worsening HF, given the significant clinical, economic, and patient burden associated with it.
References
- Buglioni A, Burnett JC Jr. Pathophysiology and the cardiorenal connection in heart failure. circulating hormones: biomarkers or mediators. Clin Chim Acta. 2015;443:3-8. doi:10.1016/j.cca.2014.10.027
- Jackson G, Gibbs CR, Davies MK, Lip GY. ABC of heart failure. Pathophysiology. BMJ. 2000;320(7228):167-170. doi:10.1136/bmj.320.7228.167
- Khan MK, Sanchez A. Chapter 11: congestive heart failure and management drugs. Access Medicine. Accessed August 14, 2020. https://accessmedicine.mhmedical.com/content.aspx?bookid=2224§ionid=171661368
- Yancy CW, Jessup M, Bozkurt B, et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice
Guidelines. J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019 - Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137-e161. doi:10.1161/CIR.0000000000000509
- Hollenberg SM, Warner Stevenson L, Ahmad T, et al. 2019 ACC Expert Consensus Decision Pathway on Risk Assessment, Management, and Clinical Trajectory of Patients Hospitalized With Heart Failure: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2019;74(15):1966-2011. doi:10.1016/j.jacc.2019.08.001
- Yancy CW, Januzzi JL Jr, Allen LA, et al. 2017 ACC expert consensus decision
pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction: a report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;71(2):201-230. doi:10.1016/j.jacc.2017.11.025 - Corlanor [prescribing information]. Amgen; 2019. Accessed August 14, 2020. https://www.pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/corlanor/corlanor_pi.pdf
- Bashore TM, Granger CB, Jackson KP, Patel MR. Chapter 10-28: sinus arrhythmia, bradycardia, & tachycardia. Access Medicine. Accessed August 14, 2020. http://accessmedicine.mhmedical.com/content.aspx?bookid=2683§ionid=225039960
- Swedberg K, Komajda M, Böhm M, et al; SHIFT Investigators. Ivabradine and
outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376(9744):875-885. doi:10.1016/S0140-6736(10)61198-1 - Armstrong PW, Pieske B, Anstrom KJ, et al; VICTORIA Study Group. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382(20):1883-1893. doi:10.1056/NEJMoa1915928
- McMurray JJV, Solomon SD, Inzucchi SE, et al; DAPA-HF Trial Committees and Investigators. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995-2008. doi:10.1056/NEJMoa1911303
- McMurray JJV, Packer M, Desai AS, et al; PARADIGM-HF Investigators and
Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure.
N Engl J Med. 2014;371(11):993-1004. doi:10.1056/NEJMoa1409077 - McMurray JJV, Packer M, Desai AS, et al; PARADIGM-HF Committees Investigators. Baseline characteristics and treatment of patients in prospective comparison
of ARNI with ACEI to determine impact on global mortality and morbidity
in heart failure trial (PARADIGM-HF). Eur J Heart Fail. 2014;16(7):817-825.
doi:10.1002/ejhf.115 - Packer M, McMurray JJV, Desai AS, et al; PARADIGM-HF Investigators and
Coordinators. Angiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failure. Circulation. 2015;131(1):54-61. doi:10.1161/CIRCULATIONAHA.114.013748 - McMurray JJV, Packer M, Desai AS, et al; PARADIGM-HF Committees and Investigators. Dual angiotensin receptor and neprilysin inhibition as an alternative to angiotensin-converting enzyme inhibition in patients with chronic systolic heart failure: rationale for and design of the Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart Failure trial (PARADIGM-HF). Eur J Heart Fail. 2013;15(9):1062-1073. doi:10.1093/eurjhf/hft052
- Entresto [prescribing information]. Novartis Pharmaceuticals Corp; 2019. Accessed 14, 2020. https://www.novartis.us/sites/www.novartis.us/files/entresto.pdf?cldi=PP1134
- Farxiga [prescribing information]. Bristol-Meyers Squibb Co; 2014. Accessed August 14, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/202293s003lbl.pdf
- Wiviott SD, Raz I, Bonaca MP, et al; DECLARE–TIMI 58 Investigators. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347-357. doi:10.1056/NEJMoa1812389
- Gheorghiade M, Greene SJ, Butler J, et al; SOCRATES-REDUCED Investigators and Coordinators. Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. JAMA. 2015;314(21):2251-2262. doi:10.1001/jama.2015.15734
- Armstrong PW, Roessig L, Patel MJ, et al. A multicenter, randomized, double-blind, placebo-controlled trial of the efficacy and safety of the oral soluble guanylate cyclase stimulator: the VICTORIA trial. JACC Heart Fail. 2018;6(2):96-104. doi:10.1016/j.jchf.2017.08.013
- Butler J, Anstrom KJ, Armstrong PW; VICTORIA Study Group. Comparing the benefit of novel therapies across clinical trials: insights from the VICTORIA trial. Circulation. Published online March 28, 2020. doi:10.1161/CIRCULATIONAHA.120.047086
- Greene SJ, Mentz RJ, Felker GM. Outpatient worsening heart failure as a target for therapy: a review. JAMA Cardiol. 2018;3(3):252-259. doi:10.1001/jamacardio.2017.5250

