- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Emerging Care Management Strategies for Severe Asthma: Integrating Biologic Therapy
To claim CE credit for this activity, please visit https://www.pharmacytimes.org/courses/emerging-care-management-strategies-for-severe-asthma-integrating-biologic-therapy
Introduction
Asthma is a chronic lung disease causing airways to intermittently become inflamed and narrow.1,2 Production of thick mucus further blocks airways. Patients with asthma indicate it feels like breathing through a straw.1 Severe asthma (SA) is associated with high morbidity for patients. Compared with patients with more mild asthma, patients with SA receive more oral corticosteroids (OCS) and report a decreased quality of life. SA imposes a high financial burden for patients, payers, and health systems.3 Furthermore, SA is strongly associated with comorbidities such as depression, gastroesophageal reflux disease, obesity, and obstructive sleep apnea.4
Disease State Overview
Severe Asthma: Background and Pathophysiology
Epidemiology
Asthma is a heterogenous disease.3 Thus, researchers have a poor understanding of asthma’s epidemiology.5 Risk factors for developing asthma include exposure to allergens and irritants, genetics, obesity, and urbanization.5 Studies suggest genetic risk influences childhood-onset asthma more than adult-onset asthma.6
Prevalence
Nationally, the American Lung Association estimates 5% to 10% of patients with asthma experience SA.7 Interestingly, there is a switch in asthma prevalence from males to females that coincides with puberty onset.5 Boys have a higher prevalence than girls, whereas adult women have a higher prevalence than men.8 Emergency department (ED) and urgent care center visits, key indicators of poorly controlled asthma, are more prevalent among children, women (18 years and older), and all racial groups except American Indian and Alaska Native persons compared with non-Hispanic White persons.8 In urban and rural areas, socioeconomic and demographic factors and healthcare usage shape patient health patterns. Patients in these areas have worse health outcomes than patients living in nonmetropolitan areas and tend to have less access to healthcare resources. Furthermore, asthma prevalence differs by poverty level. Asthma is more prevalent in patients with family incomes less than 100% of the federal poverty level (FPL) and among patients with family incomes 100% to less than 250% of the FPL compared with patients with family incomes at or above 450% of the FPL.8 To summarize, asthma is more prevalent in children younger than 18 years whose families have low incomes and among non-Hispanic Black children and those of Puerto Rican descent (compared with non-Hispanic White children).8
Symptoms
Patients with asthma experience respiratory symptoms including chest tightness, coughing, dyspnea, and wheezing, and these symptoms may vary among patients.1 Typically, symptoms are worse at night or in the early morning and may vary over time and in intensity. Asthma triggers include allergens, exercise, irritants (car exhaust fumes, smoke, strong smells), laughter, viral infections, and weather changes. Patients with asthma experience variable lung function. Forced expiratory volume in 1 second (FEV1) from spirometry and peak expiratory flow (PEF) assess lung function. Poor lung function associated with asthma is consistent with a decrease in FEV1 of more than 12% and more than 200 mL from baseline, or a change in PEF of at least 20%.9
Clinical classification of severe uncontrolled asthma
Asthma severity is determined retrospectively, based on the amount of medication necessary to achieve control.3 The Global Initiative for Asthma (GINA) defines SA as asthma that remains uncontrolled with optimized high-dose inhaled corticosteroids (ICS) in combination with a long-acting β2-agonist (LABA) or requires high-dose ICS-LABA to prevent asthma from becoming uncontrolled. Refractory SA, or difficult-to-treat asthma, does not indicate a “difficult patient.” GINA recommends patients with SA should use a specialist multidisciplinary care team for disease management.9
Importantly, uncontrolled asthma differs from SA. GINA reports that uncontrolled asthma is usually the reason for persistent symptoms and exacerbations. Patients with uncontrolled asthma may benefit from learning proper inhaler technique, improving medication adherence, and avoiding irritants.9 Pharmacists can support proper asthma management through increasing appropriate use of medication. A small pilot study conducted in Australia demonstrated that after pharmacist interventions, 42% (8/19) patients improved from poor to well-controlled asthma.10
Pathophysiology and phenotypes
Phenotypes stratify patients with asthma into groups based on observable characteristics and allow personalized treatment. Early-onset allergic asthma, late-onset eosinophilic asthma, exercise-induced asthma, obesity-related asthma, and neutrophilic asthma (nonallergic) are phenotypes.3
Endotypes are subgroups within phenotypes. Endotypes separate patients with SA into 2 groups based on airway inflammation pathways: T-helper type 2 (T2) lymphocytes high and T2 low.3 T2 inflammation is eosinophilic-stimulated airway inflammation. Interleukin (IL)-3, IL-4, IL-5, IL-9, IL-13, and granulocyte-macrophage colony-stimulating factor induce eosinophil maturation, basophil recruitment, and immunoglobulin (Ig) E production, driving T2-high endotype. Mucus production, airway granulocyte activation, and airway hyperactivity result.4
Biomarker detection identifies patients with T2-high or T2-low SA. Clinicians use fraction of exhaled nitric oxide (FeNO), IgE, and serum periostin levels to individualize therapy based on endotype. Clinicians cannot use IgE levels alone to differentiate between T2-high and T2-low SA because patients with nonatopic asthma may have elevated IgE levels. Patients with T2 inflammation have blood eosinophils greater than or equal to 150 cells per microliter, FeNO greater than or equal to 20 parts per billion, and may have a beneficial response to ICS.11-13 Serum periostin is another biomarker useful to determine T2 airway inflammation in patients with SA.14 Although the T2-low endotype is not well defined, the pathophysiology involves neutrophils. Asthma associated with obesity, smoking, bacterial and viral infections, and late-onset asthma are associated with the T2-low inflammatory endotype.4
Assessment
Multiple asthma guidelines are used to assess and treat asthma, including guidelines from the European Respiratory Society and American Thoracic Society (ERS/ATS), the National Asthma Education and Prevention Program (NAEPP), and GINA. ERS/ATS and GINA recommend assessing asthma control and severity.9,15 Similarly, NAEPP guidelines advise assessing control because it is a key element of asthma care. Pharmacists should first check adherence, inhaler technique, environmental factors, and comorbid conditions.16 Pharmacists can also assist with appropriate medication selection by recommending step-up or step-down therapy.10 Healthcare professionals can assess symptom control using the Asthma Control Test and Asthma Control Questionnaire. As risk factors for future exacerbations are independent of symptom control, the following should be considered9 :
- Blood eosinophil levels
- Greater than or equal to 1 exacerbation in the previous year
- Incorrect inhaler technique
- Low FEV1
- Poor adherence
- Smoking
- Socioeconomic problems
Furthermore, GINA advises assessing risk factors for persistent airflow limitation, medication adverse effects, and comorbidities that could contribute to symptom burden and poor quality of life. Providers should assess lung function at diagnosis (or start of treatment), after 3 to 6 months of controller treatment, and periodically thereafter.9
Clinical Guidelines and FDA-Approved Treatments
Current Treatments for Severe Asthma
The main goal of therapy for patients with SA is disease control. Previously, high-dose ICS in combination with LABAs were the only treatments available for SA. Presently, biologics are indicated after phenotyping individual patients who continue to exhibit symptoms and have exacerbations to encourage specific treatment plans.3
Standards of care
GINA guidelines offer a decision tree to treat SA phenotypes.9 The ERS/ATS guidelines use the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) acronym to provide individual recommendations for using biologics that target IL-5, IgE, and IL-4/IL-13 pathways.17 NAEPP also uses the GRADE framework to develop recommendations for step diagrams that guide treatment. Unsurprisingly, strong recommendations are absent for treating asthma, given the variations in phenotypes and endotypes. A need exists for optimized personalized medicine to tailor interventions and treatments to patients with certain characteristics.16 Providers should use patient phenotype and endotype to guide treatment.
Candidates for biologic agents
Patients with SA who remains uncontrolled, despite treatment with high-dose ICS and LABAs, have options to help alleviate symptoms. Add-on therapy with leukotriene receptor antagonists, OCS, macrolides, and long-acting muscarinic antagonists may help reduce symptoms.3,6 Unfortunately, SA may remain uncontrolled with these therapies, and the adverse effects of OCS limit their use.6 Allergic IgE-related SA and eosinophilic asthma are responsive to treatment with anti-IgE and anti–IL-5 cytokine therapies, respectively. However, there are limited treatment options for patients who lack evidence of T2 inflammation.3
Biologics
Current guidelines recommend phenotyping patients to aid in the selection of additional treatment.9 Pharmacists can use phenotype to choose among 5 biologics for the treatment of eosinophilic inflammation (see Table 118-24).3
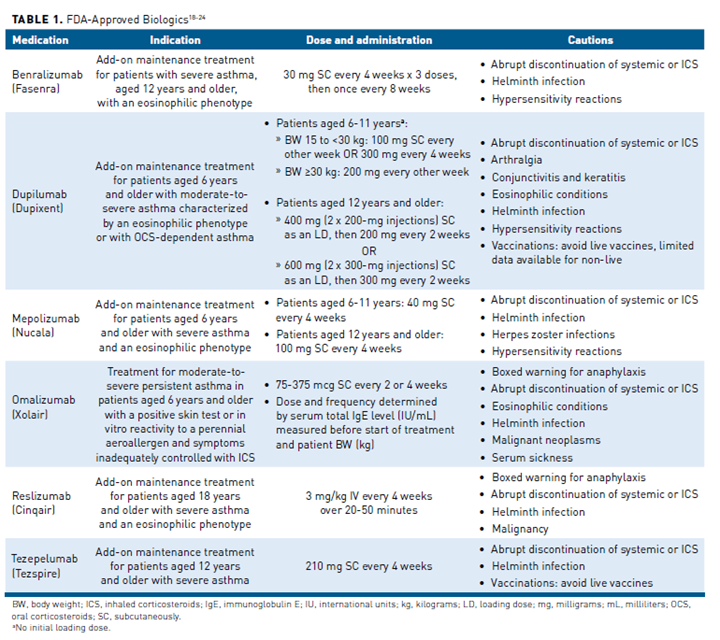
Patient adherence is generally higher with asthma biologics than with inhalers, in part because biologics are not dosed daily.25 Depending on the agent, administration is every 2 to 8 weeks. The first 5 FDA-approved biologics to treat moderate to SA are18-24:
Benralizumab, an IL-5 receptor alpha-directed cytolytic monoclonal antibody (IgG1 kappa [Κ])
- Dupilumab, an IL-4 receptor α antagonist
- Mepolizumab, an IL-5 antagonist monoclonal antibody (IgG1 Κ)
- Omalizumab, an anti-IgE antibody
- Reslizumab, an IL-5 antagonist monoclonal antibody (IgG4 Κ)
Benralizumab
Researchers conducted three phase 3 confirmatory trials (SIROCCO, CALIMA, and ZONDA) and a lung function trial (BISE). SIROCCO and CALIMA were both randomized, double-blind, placebo-controlled trials with a primary end point of asthma exacerbations. These trials showed reductions in exacerbation rates for treated patients compared with patients receiving placebo. Also, the time to first exacerbation was longer for patients receiving benralizumab compared with placebo. Researchers studied the effect of benralizumab on reducing maintenance OCS use in the ZONDA trial (randomized, double blind). Treated patients achieved greater reductions in daily maintenance OCS doses while maintaining asthma control. In the phase 3 BISE trial, benralizumab provided consistent improvements in the mean change from baseline FEV1.20,26-29
Dupilumab
Researchers evaluated dupilumab in 3 randomized, placebo-controlled, multicenter trials (DRI12544, QUEST, and VENTURE). The primary end point of DRI12544 was mean change from baseline FEV1. The primary end points of the QUEST trial were annualized rate of severe exacerbation events and change of FEV1 from baseline before treatment with a bronchodilator. Treated patients had significant reductions in asthma exacerbation rates and had significant increases in pre-bronchodilator FEV1. Additionally, treated patients in QUEST experienced a longer time to first exacerbation compared with placebo. VENTURE’s primary end point was percent reduction of OCS dose, while maintaining asthma control, compared with baseline OCS doses. Patients receiving dupilumab achieved greater reductions in daily maintenance OCS dose compared with placebo. Researchers also evaluated dupilumab’s safety profile in pediatric patients aged 6 years to 11 years in the VOYAGE trial. Researchers concluded that treatment with dupilumab significantly reduced asthma exacerbation rates in patients with an eosinophilic phenotype.19
Mepolizumab
Mepolizumab was similarly tested in 2 double-blind, randomized, placebo-controlled confirmatory trials (MENSA and SIRIUS). MENSA, a phase 3 trial, assessed efficacy of mepolizumab. The primary outcome was rate of exacerbations. Researchers found that treated patients experienced significantly fewer exacerbations compared with placebo. SIRIUS, a phase 3 trial, evaluated mepolizumab’s effect on reducing maintenance OCS. Treated patients achieved greater reductions in maintenance OCS, while maintaining asthma control, compared with placebo. More than half (54%) of treated patients achieved at least a 50% reduction in the daily prednisone dose.21,30
Omalizumab
Omalizumab was also evaluated for safety and efficacy in 3 randomized, double-blind, placebo-controlled trials. The trials enrolled patients with moderate to severe persistent asthma for at least 1 year, and a positive skin test reaction to a perennial aeroallergen. Asthma Trials 1 and 2 concluded that treated patients had fewer exacerbations compared with placebo. At screening, Trials 1 and 2 included patients with an FEV1 from 40% to 80% predicted; however, there was no restriction on screening FEV1 in Trial 3. Unlike Trials 1 and 2, researchers allowed using LABAs in Trial 3. Unfortunately, treated patients in Trial 3 had a similar number of exacerbations compared with placebo. Researchers hypothesize that differences in patient population, study sample size, or other factors may explain the lack of efficacy in Trial 3.22,31-33
Reslizumab
Four randomized, double-blind, placebo-controlled trials evaluated reslizumab. Studies I, II, and III included patients with asthma and blood eosinophil counts of at least 400 cells per microliter. Study IV included patients with asthma and blood eosinophil counts fewer than 400 cells per microliter. Researchers studied patients given reslizumab or placebo by intravenous infusion every 4 weeks. The primary end point for studies I and II was frequency of asthma exacerbations. Researchers found that patients treated with reslizumab had significant reductions in asthma exacerbations, and the time to first exacerbation was significantly longer. The primary end point for study III and IV was FEV1. Treated patients produced significant changes in FEV1. Although other doses were studied, 3 mg/kg is the only recommended dose.18
Tezepelumab
Two double-blind, randomized, placebo-controlled trials demonstrated the effectiveness of tezepelumab: PATHWAY and NAVIGATOR. In PATHWAY, a phase 2 trial, researchers found patients treated with tezepelumab had significantly lower annualized asthma exacerbation rates than patients who received placebo.34 The phase 3 NAVIGATOR trial demonstrated consistent reduction of exacerbations in treated patients, irrespective of baseline blood eosinophil count.35 Patients who participated in phase 3 tezepelumab trials were eligible to enter an extension study to evaluate long-term safety and efficacy (DESTINATION).35 The study is now complete, but researchers have yet to post results.36
Managed Care Considerations
Approximately 40% of patients with SA remain uncontrolled.37 These patients consume significant healthcare resources. Asthma-related healthcare costs for patients with severe uncontrolled asthma are almost double the costs for patients with severe controlled asthma.38
Healthcare Resource Utilization
Chastek and colleagues conducted a retrospective analysis of 65,359 patients with continuous pharmacy coverage under a commercial or Medicare Advantage plan over 2 years (2012-2013). Patients in the study were 12 years or older, with 1 medical claim including an asthma diagnosis. Researchers assigned patients to either the persistent asthma or SA cohort to estimate asthma-related healthcare utilization.38
The largest driver of high asthma-related costs was medications, which were 3-fold higher for patients with SA. Notably, patients in the SA cohort had greater usage of every controller and rescue medication in both years compared with the other cohort. Adjusted costs of asthma-related medications were $4020 higher for patients with SA (cost ratio, 2.982; 95% CI, 2.660-3.342). Higher medication costs resulted from more prescription fills and better adherence to refill schedules for long-term controller therapy in the SA cohort.38
The second largest driver was more than twice as many hospitalizations, outpatient visits, and asthma-related office visits for patients with SA compared with those with persistent asthma. Furthermore, patients with SA had 41% greater use of asthma-related ED visits despite better adherence to controller therapy. Adjusted all-cause total costs among patients with SA were 77.9% higher (cost difference, $8758; cost ratio, 1.779; 95% CI, 1.623-1.950) compared with the persistent asthma cohort.38
In another study, Song et al examined direct medical costs and indirect costs due to absenteeism (productivity loss) in patients with asthma. Of the 183,537 individuals included in the study, 13,732 patients had asthma, but researchers classified just 0.7% (n = 98) as having SA. Patients with SA tended to have more hospitalizations, ED visits, and outpatient visits compared with patients with mild asthma. Researchers found that the number of hospitalizations increased as asthma severity increased. Patients with SA spent 5.55 additional days in the hospital compared with those with mild asthma. Additionally, patients had more ED visits per person per year (PPPY) in mild (0.13), moderate (0.17), and SA (0.28) than patients without asthma (P <.05). Outpatient visit rates PPPY among patients with mild (2.53), moderate (3.67), and SA (6.72) were significantly higher compared with patients without asthma (P <.05).39
This study also demonstrated that total direct medical costs increased with asthma severity. Direct medical costs were 2.8 times higher and indirect costs were 9.4 times higher for patients with SA (compared with those with mild asthma). Prescription medications PPPY (moderate vs mild, $3805; severe vs mild, $6479) and outpatient visit costs PPPY (moderate vs mild, $604; severe vs mild, $2001) are the greatest drivers contributing to direct costs. Incremental indirect costs associated with missed work or school days PPPY were greater in patients with SA ($894 compared with mild asthma) than in patients with moderate asthma ($215 compared with mild asthma). Song et al concluded that controlling asthma symptoms is crucial for reducing the socioeconomic burden of asthma.39
Poorly controlled asthma also affects children. A child’s inability to attend school may affect academic performance and may cause parents to miss work to care for their child. The Centers for Disease Control and Prevention reports that children with asthma missed 13.8 million school days in 2013. The number of reported missed school days did not differ by age, ethnicity, poverty level, race, or sex.40 However, inadequate control and treatment of severe asthma is not limited to just direct and indirect costs. Some treatments may also pose some undesirable effects in addition to poorly managing severe asthma.
Glucocorticoid-Sparing Effect
SA treated with chronic and intermittent OCS is associated with considerable adverse effects. OCS are associated with comorbidities such as bone fractures, diabetes, dyspeptic disorders, hypertension, osteoporosis, and sleep disturbances. These comorbidities may decrease health-related quality of life and worsen prognosis. Following long-term use, withdrawal from maintenance OCS may result in prolonged adrenal insufficiency.
Biologics and OCS target the same T2 inflammation mediators (ie, IgE, IL-5, IL-4, IL-13). Observational studies confirm the OCS-sparing effect of biologic therapies in SA, indicating that they offer a safer alternative. Clinicians should avoid direct comparisons among biologics because study design impacts outcomes.37
OCS pose another problem for patients: OCS deplete blood eosinophils. Reimbursement criteria for biologics may require blood eosinophil levels greater than or equal to 300 cells per microliter during the last year and at initiation. To circumvent this criterion, providers may temporarily decrease OCS doses to allow patient eosinophil levels to recover. Unfortunately, this work-around comes with risk of worsening asthma or causing exacerbations.37 To avoid these adverse effects and better manage severe asthma, initiation of biologics should be considered.
Prior Authorization Criteria
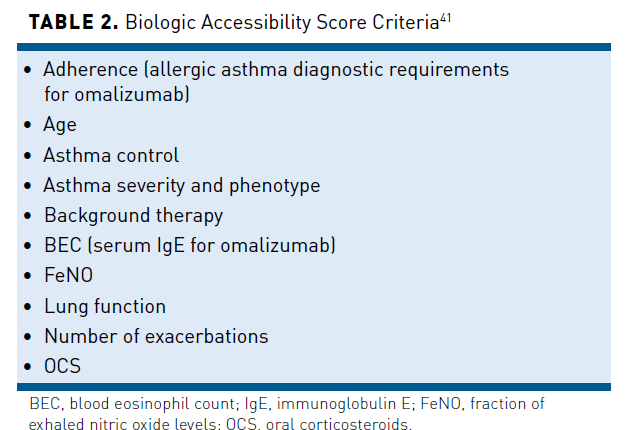
Biologic therapies often require prior authorization. Delayed access to biologics may have long-term detrimental impacts for patients with SA. Porsbjerg et al studied accessibility to the first 5 FDA-approved biologics. Researchers developed the Biologic Accessibility Score (BACS) to stratify ease of access to these prescriptions. BACS incorporates 10 prescription criteria (see Table 241), and a higher score indicates easier access. This study found BACS specifications for benralizumab, dupilumab, both mepolizumab and omalizumab, and reslizumab, respectively, to be 58, 68, 52, and 61.41
A recent study looking at the impact of prior authorizations on patients found insurance approval time varied from 1 day to 97 days (from date prior authorization submitted to date approved). This study also examined pharmacy fill times and found a mean time of more than 40 days to approve and fill asthma biologics. Researchers associated significant delays in biologic initiation with a risk of asthma exacerbations. In this study, almost half of the subjects (47%) with SA had exacerbations requiring 1 or more courses of prednisone while waiting for a biologic.42 Managed care organizations (MCOs) need to optimize prior authorization processes to ensure prompt decisions for timely and appropriate patient access to biologics.
Care Management/Coordination of Care
The NAEPP recommends a collaborative effort among pharmacists, primary care physicians, pulmonary specialists, and case managers. MCOs that use this comprehensive approach have shown an improvement in asthma outcomes. Teams work together to identify high-risk patients, use treatment guidelines, and educate patients on disease and treatment.43 After patients receive disease education, they are equipped with knowledge to identify and avoid asthma triggers. Education increases patient awareness of their disease, allowing them to better manage it and improve their quality of life.43
Clinical Pathway Efficacy in Severe Asthma
As new data and emerging agents become available, it is important for pharmacists to stay informed on therapeutic advances with the most recent studies. Education allows managed care pharmacists to recommend emerging treatments targeted to individual patients, maximize safety, increase access, and decrease exacerbations and hospitalizations.43
Conclusions
The heterogeneity of SA calls upon caregivers to advance personalized medicine. Prescribers and pharmacists can collaborate during the prior authorization evaluation and approval process to coordinate drug selection based on patient phenotype and endotype. MCOs can optimize prior authorization processes to assist patients in accessing targeted asthma medications in a timely manner. Minimizing uncontrolled asthma symptoms with biologic therapy can improve patient outcomes and reduce healthcare resource utilization.
Author affiliation: Russell Spjut, PharmD, is the Director of Formulary Management at Magellan Rx Management, Salt Lake City, UT.
Funding source: This activity is supported by an educational grant from Novartis.
Author disclosure: Dr Spjut has no relevant financial relationships with commercial interests to disclose.
Authorship information: Substantial contributions to acquisition of data; analysis and interpretation of data; drafting of the manuscript; and critical revision of the manuscript for important intellectual content.
Address correspondence to: russellspjut@outlook.com
Medical writing and editorial support provided by: Ashley Ann Walsh, PharmD
REFERENCES
- National Heart, Lung, and Blood Institute (NHLBI). Learn more breathe better. Published March 2020. Accessed July 2, 2022. www.nhlbi.nih.gov/resources/lmbb-what-asthma
- National Heart, Lung, and Blood Institute (NHLBI). What is asthma? Updated March 24, 2022. Accessed June 20, 2022. www.nhlbi.nih.gov/health/asthma
- Côté A, Godbout K, Boulet LP. The management of severe asthma in 2020. Biochem Pharmacol. 2020;179:114112. doi:10.1016/j.bcp.2020.114112
- Dorey-Stein ZL, Shenoy KV. Tezepelumab as an emerging therapeutic option for the treatment of severe asthma: evidence to date. Drug Des Devel Ther. 2021;15:331-338. doi:10.2147/DDDT.S250825
- Kuruvilla ME, Vanijcharoenkarn K, Shih JA, Lee FE. Epidemiology and risk factors for asthma. Respir Med. 2019;149:16-22. doi:10.1016/j.rmed.2019.01.014
- Schoettler N, Strek ME. Recent advances in severe asthma: from phenotypes to personalized medicine. Chest. 2020;157(3):516-528. doi:10.1016/j.chest.2019.10.009
- American Lung Association. Severe asthma. Updated October 6, 2021. Accessed June 20, 2022. www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/learn-about-asthma/severe-asthma
- Pate CA, Zahran HS, Qin X, Johnson C, Hummelman E, Malilay J. Asthma Surveillance – United States, 2006-2018. MMWR Surveill Summ. 2021;70(5):1-32. doi:10.15585/mmwr.ss7005a1
- Global Initiative for Asthma. Global strategy for asthma management and prevention (2022 update). Accessed August 8, 2022. https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf
- Deeks LS, Kosari S, Boom K, et al. The Role of Pharmacists in General Practice in Asthma Management: a pilot study. Pharmacy (Basel). 2018;6(4):114. doi:10.3390/pharmacy6040114
- Agache I, Akdis CA, Akdis M, et al. EAACI biologicals guidelines–recommendations for severe asthma. Allergy. 2021;76(1):14-44. doi:10.1111/all.14425
- Pavlidis S, Takahashi K, Ng Kee Kwong F, et al; U-BIOPRED Study Group. “T2-high” in severe asthma related to blood eosinophil, exhaled nitric oxide and serum periostin. Eur Respir J. 2019;53(1):1800938. doi:10.1183/13993003.00938-2018
- Ricciardolo FLM, Sprio AE, Baroso A, et al. Characterization of T2-low and T2-high asthma phenotypes in real-life. Biomedicines. 2021;9(11):1684. doi:10.3390/biomedicines9111684
- Matsumoto H. Role of serum periostin in the management of asthma and its comorbidities. Respir Investig. 2020;58(3):144-154. doi:10.1016/j.resinv.2020.02.003
- Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343-373. doi:10.1183/09031936.00202013
- The National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. 2020 focused update to the asthma management guidelines. Published December 2020. Accessed June 20, 2022. www.nhlbi.nih.gov/health-topics/all-publications-and-resources/2020-focused-updates-asthma-management-guidelines
- Holguin F, Cardet JC, Chung KF, et al. Management of severe asthma: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2020;55(1):1900588. doi:10.1183/13993003.00588-2019
- Cinqair. Prescribing information. Teva Pharmaceuticals; 2020. Accessed June 26, 2022. www.cinqairhcp.com/globalassets/cinqair-hcp-redesign/prescribing-information.pdf
- Dupixent. Prescribing information. Regeneron; 2022. Accessed June 13, 2022. www.regeneron.com/downloads/dupixent_fpi.pdf
- Fasenra. Prescribing information. AstraZeneca; 2021. Accessed June 26. 2022. https://den8dhaj6zs0e.cloudfront.net/50fd68b9-106b-4550-b5d0-12b045f8b184/3647bed4-ce91-4fe7-9bc5-32dbee73f80a/3647bed4-ce91-4fe7-9bc5-32dbee73f80a_viewable_rendition__v.pdf
- Nucala. Prescribing information. GlaxoSmithKline; 2022. Accessed June 26, 2022. https://gskpro.com/content/dam/global/hcpportal/en_US/Prescribing_Information/Nucala/pdf/NUCALA-PI-PIL-IFU-COMBINED.PDF
- Xolair. Prescribing information. Genentech; 2021. Accessed June 26, 2022. www.gene.com/download/pdf/xolair_prescribing.pdf
- Tezspire. Prescribing information. AstraZeneca; 2021. Accessed August 8, 2022. https://den8dhaj6zs0e.cloudfront.net/50fd68b9-106b-4550-b5d0-12b045f8b184/e306dc06-d580-4457-b15f-9f28545ad63a/e306dc06-d580-4457-b15f-9f28545ad63a_viewable_rendition__v.pdf
- Food and Drug Administration (FDA). FDA approves maintenance treatment for severe asthma. Updated December 20, 2021. Accessed June 26, 2022. www.fda.gov/drugs/news-events-human-drugs/fda-approves-maintenance-treatment-severe-asthma
- Maddux JT, Inselman JW, Jeffery MM, Lam RW, Shah ND, Rank MA. Adherence to asthma biologics: implications for patient selection, step therapy, and outcomes. Chest. 2021;159(3):924-932. doi:10.1016/j.chest.2020.10.050
- Bleecker ER, FitzGerald JM, Chanez P, et al; SIROCCO study investigators. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting β2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2115-2127. doi:10.1016/S0140-6736(16)31324-1
- Harrison TW, Chanez P, Menzella F, et al; ANDHI study investigators. Onset of effect and impact on health-related quality of life, exacerbation rate, lung function, and nasal polyposis symptoms for patients with severe eosinophilic asthma treated with benralizumab (ANDHI): a randomised, controlled, phase 3b trial. Lancet Respir Med. 2021;9(3):260-274. doi:10.1016/S2213-2600(20)30414-8
- Nair P, Wenzel S, Rabe KF, et al; ZONDA trial investigators. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376(25):2448-2458. doi:10.1056/NEJMoa1703501
- FitzGerald JM, Bleecker ER, Nair P, et al; CALIMA study investigators. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128-2141. doi:10.1016/S0140-6736(16)31322-8
- Ortega HG, Liu MC, Pavord ID, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371(13):1198-1207. doi:10.1056/NEJMoa1403290
- Busse W, Corren J, Lanier BQ, et al. Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J Allergy Clin Immunol. 2001;108(2):184-190. doi:10.1067/mai.2001.117880
- Hanania NA, Alpan O, Hamilos DL, et al. Omalizumab in severe allergic asthma inadequately controlled with standard therapy: a randomized trial. Ann Intern Med. 2011;154(9):573-582. doi:10.7326/0003-4819-154-9-201105030-00002
- Solèr M, Matz J, Townley R, et al. The anti-IgE antibody omalizumab reduces exacerbations and steroid requirement in allergic asthmatics. Eur Respir J. 2001;18(2):254-261. doi:10.1183/09031936.01.00092101
- Corren J, Parnes JR, Wang L, et al. Tezepelumab in adults with uncontrolled asthma. N Engl J Med. 2017;377(10):936-946. doi:10.1056/NEJMoa1704064
- Menzies-Gow A, Corren J, Bourdin A, et al. Tezepelumab in adults and adolescents with severe, uncontrolled asthma. N Engl J Med. 2021;384(19):1800-1809. doi:10.1056/NEJMoa2034975
- Extension study to evaluate the safety and tolerability of tezepelumab in adults and adolescents with severe, uncontrolled asthma (DESTINATION). ClinicalTrials.gov. Updated May 26, 2022. Accessed July 3, 2022. https://clinicaltrials.gov/ct2/show/NCT03706079?term=NCT03706079&draw=2&rank=1
- Cataldo D, Louis R, Michils A, et al. Severe asthma: oral corticosteroid alternatives and the need for optimal referral pathways. J Asthma. 2021;58(4):448-458. doi:10.1080/02770903.2019.1705335
- Chastek B, Korrer S, Nagar SP, et al. Economic burden of illness among patients with severe asthma in a managed care setting. J Manag Care Spec Pharm. 2016;22(7):848-861. doi:10.18553/jmcp.2016.22.7.848
- Song HJ, Blake KV, Wilson DL, Winterstein AG, Park H. Medical costs and productivity loss due to mild, moderate, and severe asthma in the United States. J Asthma Allergy. 2020;13:545-555. doi:10.2147/JAA.S272681
- Centers for Disease Control and Prevention (CDC). Asthma-related missed school days among children aged 5-17 years. Updated October 5, 2015. Accessed June 28, 2022. www.cdc.gov/asthma/asthma_stats/missing_days.htm
- Porsbjerg CM, Menzies-Gow AN, Tran TN, et al. Global variability in administrative approval prescription criteria for biologic therapy in severe asthma. J Allergy Clin Immunol Pract. 2022;10(5):1202-1216.e23. doi:10.1016/j.jaip.2021.12.027
- Dudiak GJ, Popyack J, Grimm C, Tyson S, Solic J, Ishmael FT. Prior authorization delays biologic initiation and is associated with a risk of asthma exacerbations. Allergy Asthma Proc. 2021;42(1):65-71. doi:10.2500/aap.2021.42.200101
- Campbell JD. Implications for asthma treatment strategies in managed care. Am J Manag Care. 2017;23:S12-S19.
