- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Economic Burden of Illness in Opioid Use Disorder (OUD) and Medication-Assisted Treatments
Introduction
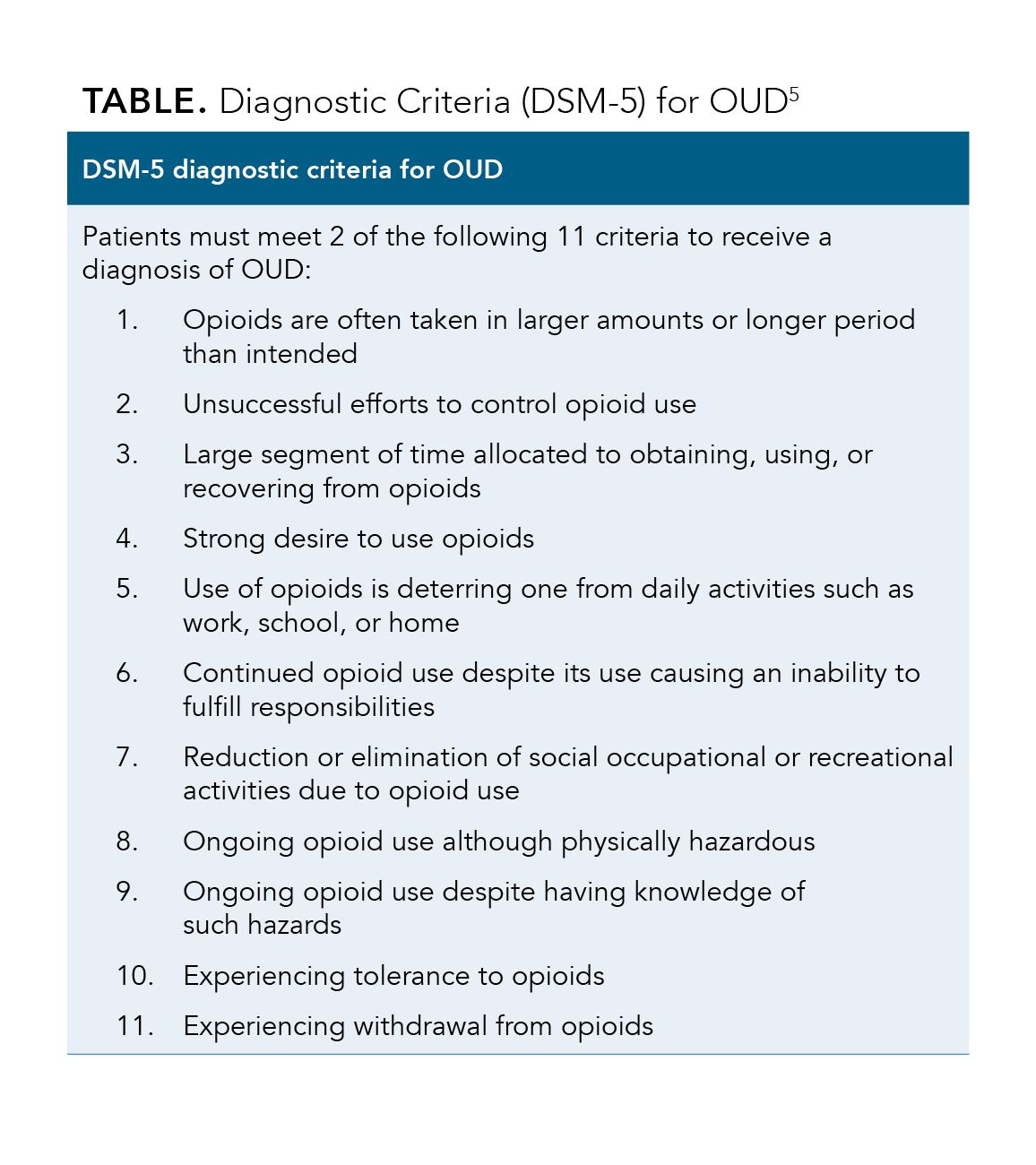
The opioid epidemic began in the 1990s and has become a major health crisis affecting many people in the United States (US).1 The Centers for Disease Control and Prevention (CDC) estimated that more than 700,000 people died in the US due to drug overdose from 1999 to 2017.1 Consequently, the US Department of Health and Human Services, declared the epidemic a public health emergency, as more than 130 individuals died per day due to opioid-related drug overdose in 2017.2 Opioids include heroin, synthetic opioids, and prescription pain relievers, namely hydrocodone, oxycodone, and morphine.3 Although prescription opioid use is legal and prescribed for individuals with chronic or acute pain, the prescribed or the illicit use of opioids can equally lead to opioid use disorder (OUD).4 OUD is a disease characterized by the chronic use of opioids leading to impairment or distress.5 In order to confirm a diagnosis of OUD, at least two of the 11 criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (Table) need to be observed within a 12-month period.5 The National Survey On Drug Use And Health estimated that 2.0 million people 12 years of age or older were diagnosed with OUD in 2018.6
Table
Concurrently, the opioid epidemic has impacted the US economy, with an estimated economic cost of $504 billion (2015) due to the opioid crisis.7 Similarly, the Society of Actuaries (SOA) reported a total economic burden of at least $631 billion (2015 to 2018) in the United States.8 Factors that contributed to the total economic burden included healthcare costs, mortality, criminal justice, family assistance, education, and lost productivity in the labor force.8 For the well-being of the US economy and the collective health of Americans, education, research, and support are needed to provide paths to effectively deal with the opioid epidemic.
Cost to Employers
The opioid epidemic clearly impacts both employers and employees. According to the National Safety Council (NSC), the opioid epidemic is affecting US companies across the country.9 A survey commissioned to determine the effects of opioids on businesses and how employers handle opioid-related issues determined that out of 526 employers surveyed, more employers were concerned with the ability to hire qualified workers (58%), employee benefit costs (53%), and worker compensation (44%) costs than the misuse of illicit opioids (42%) or illicit use/sale of opioids (36%).10 Even though 75% of US employers were affected by employee use of opioids, only 17% of US employers were well prepared to handle employees with opioid use in the workplace.10 Additionally, the NSC discovered that 38% of US employers acquired costs due to absenteeism and 31% of employees experienced either an opioid overdose, were detained for opioid-related crimes, or were injured on the job due to opioid misuse.10 While 60% of employers have policies that require employees to notify them of prescription opioid use, 79% of employers do not believe employees are able to recognize indications of opioid abuse and only about half of employers believe they have the resources to effectively handle opioid-related challenges.9
Employer Costs
Workers who are diagnosed with OUD pose a great economic burden on the healthcare system and workers on short-term disability with diagnosed opioid abuse have greater lost wages and time away from work than those without a diagnosis of OUD.11 The SOA states that lost productivity costs associated with employee incarceration for opioid abuse, short-term and long-term disability, and worker’s compensation to employees with OUD totaled an estimated $96 billion from 2015 to 2018.8 Within that time frame, lost productivity for nonmedical opioid use cost $78.6 billion in the US. Consequently, these individuals are at higher risk for incarceration because of opioid related crimes; therefore, approximately $13.6 billion in productivity was lost due to potential workers being incarcerated. Additionally, employees who suffer from work-related injuries are granted pay replacement through short- and long-term disability programs and worker’s compensation claims. The SOA found that worker’s compensation had the highest cost ($500 million), followed by short-term disability ($417 million), and lastly long-term disability ($38 million), with a total cost of $3.4 billion for employees with OUD.8
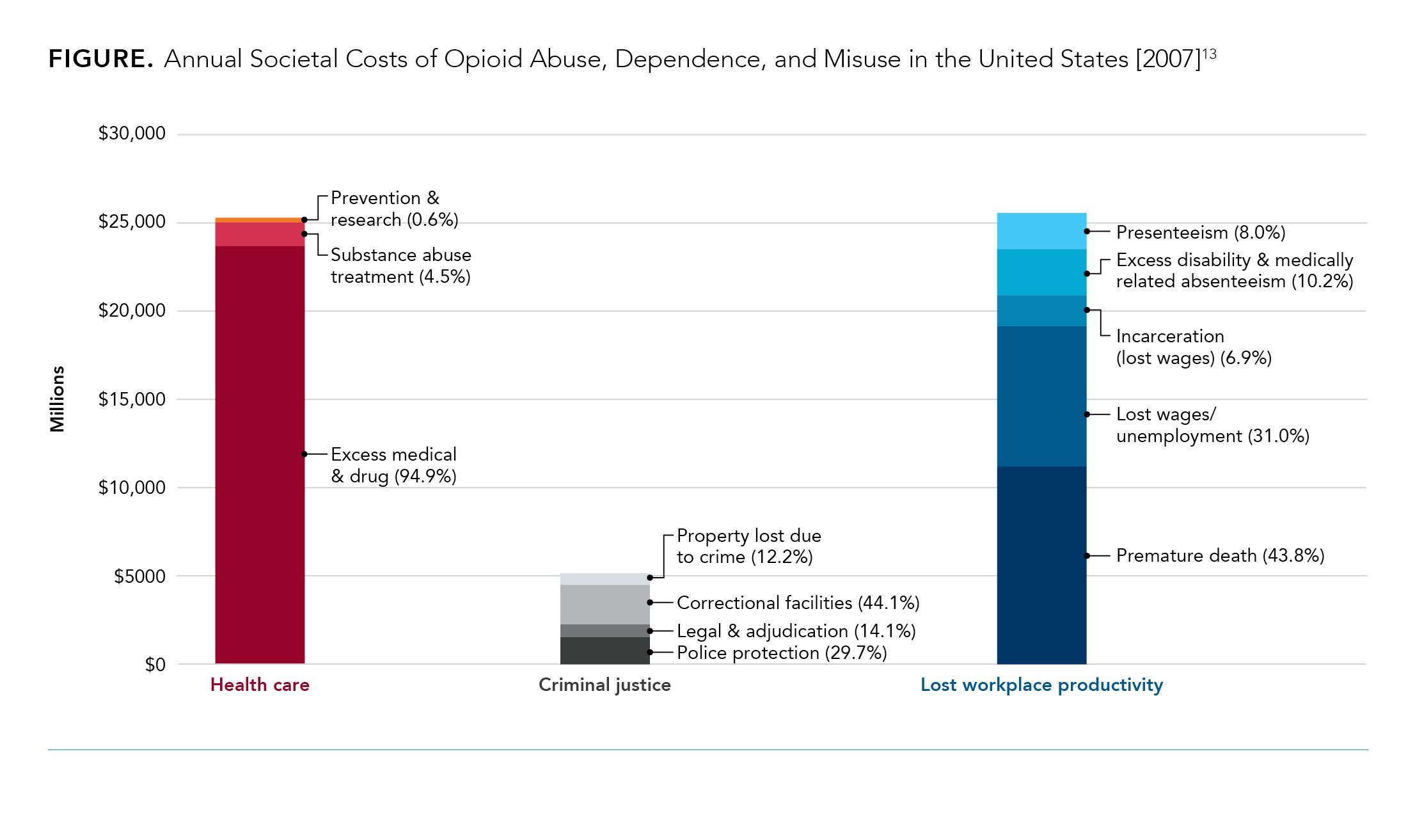
Individuals with OUD also missed an average of 6.3 more work days on disability leave (15.5 [standard deviation {SD} 51.7] versus 9.2 [SD 36.3]; P = .002); and 7.0 more work days due to medically related absenteeism (13.4 [SD 19.3] versus 6.4 [SD 7.2]; P < .001) totaling to an average of 13.3 more work days missed annually. This contributed to higher total work-loss costs than the average employee (US$3,773 [SD US$6,648] versus US$2,528 [SD US$4,612]).12 In 2011, an employee with OUD was estimated to have $10,627 annually in healthcare costs and $1244 in excess annual work-lost cost.12 This was largely due to disability or medically-related absenteeism, where it was estimated in 2007 that employees with OUD accounted for 90.1% and 64.5% of costs, respectively.13
Opioid Treatment Programs (OTPs) and Rehabilitation Costs
As reported by the Kaiser Family Foundation (KFF), large employer healthcare plans spent $1.4 billion on opioid prescriptions in 2016. Although the KFF data indicated a decline in opioid prescription rates, spending on treatment for OUD and overdose increased. For instance, opioid treatment costs surged from $0.3 billion in 2004 to $2.6 billion in 2016.14 This is in part because OTPs and treatments offered through rehabilitation centers are expensive, but costs can vary depending on employer healthcare plans—the average cost of drug rehabilitation in 2019 was anywhere from $5000 to $80,000.15
In addition to providing individually-designed programs with psychological therapies and supportive services that focus on the various factors affecting OUD patients,16 OTPs also provide medication-assisted treatment (MAT) for individuals with OUD.17 MAT has improved patient survival, increased work stability, sustained retention in treatment, and has been shown to reduce opioid misuse and decrease opioid-related criminal activity.17 TRICARE, a healthcare program of the US Department of Defense, determined treatment costs for three medications (methadone, buprenorphine, and naltrexone) used in OTPs; the estimated annual costs for methadone, buprenorphine, and naltrexone per beneficiaries as of 2018 were $6500, $5900, and $14,112, respectively.16,18 Although MATs seem costly, to place them in perspective, the Agency for Healthcare Research and Quality estimated that the average cost per person for any service for diabetes mellitus or kidney disease was $3560 and $5624, respectively, in 2014.19 Thus, the cost of MAT use by OTPs is a small portion of costs compared to the total healthcare costs associated with opioids; to this end opioid treatment accounted for only 2.0% of the total $25.6 billion societal costs spent on health care in 2007 (Figure).13
Figure
The Opioid Epidemic Has Hit Certain Workforces Hard
In the US workplace, drug overdose deaths were determined from the Bureau of Labor Statistics (BLA) Census of Fatal Occupational Injuries database.20 Between 2011 to 2016, 760 overdose deaths occurred in US workplaces.20 The transportation and warehousing industry, the construction industry, and the healthcare and social assistance industry experienced the highest number of workplace overdose fatalities.20 In addition, the BLA reported in 2018 that overdose deaths that occurred at work increased by 12%, making it the 6th time these deaths have increased annually.21 Further, the NSC states that employees who abuse opioids are a safety threat to not only themselves, but also their coworkers; OUD causes impairment, can cause errors, work-related injury, inhibit transportation to and from work, and decrease the ability to focus/pay attention to detail.4
Although OUD is prevalent across the US, construction, mining, and other industrial services have higher rates of OUD than the national workforce average.22 A study describing the chronic opioid use in an industrial cohort found that between 2003 and 2013 there was more than a 10-fold increase in workers diagnosed with OUD (2013, n = 11, 0.02%; 2013, n = 67, 0.28%; P < .001). For example, in 2003, 0.69% of industrial workers had chronic opioid prescriptions compared to 2.9% in 2013.23 Furthermore, workers had a higher chance of being prescribed opioids if they were experiencing symptoms such as back, neck, or head pain, or were diagnosed with osteoarthritis, depression, or diabetes.23 These symptoms aided in the number of opioids prescribed chronically which increased from 6.6% in 2003 to 16% in 2013.23
Expanded Guidance For Employee Drug Use/Testing are Needed
In accordance with the American College of Occupational and Environmental Medicine guidelines, industries such as railroad, public transit, and aircraft do not recommend opioid use for workers in machine-operating positions.24 An employee taking any medication that has the capacity to impair their ability to work must be evaluated by the medical review officer and the prescribing physician, but while this is their responsibility, they don’t have the expertise for this, nor is the evaluation well-structured under current regulations.25 The NSC advises employers to work with human resources and legal counsel to develop such policies surrounding prescription medications.26
Education on OUD Is Needed for Employers
Education is vital for employers who are learning how to handle the challenges associated with OUD. The US Senate passed the “Preventing Opioid and Drug Impairment in Transportation Act,” a bill to facilitate drug testing for transportation-related activities. The bill states, “the National Railroad Passenger Corporation (commonly known as Amtrak) shall submit a report to the Committee on Commerce, Science, and Transportation of the Senate… that describes the methods used by Amtrak to ensure that supervisors of employees in safety-sensitive positions receive the required training on how to detect drug and alcohol use.” Thus, according to regulation, it is mandatory for employers to have drug testing methods in place for employees in safety-sensitive jobs (eg, drivers, heavy machinery operators). 27
Effective Management of OUD Is Essential for Successful Employee Rehabilitation
To combat the current crisis, NSC recently introduced their free Opioids at Work Employer Toolkit, which employers can use to reduce costs and help employees with OUD.28 As stated in this document, some of the key steps for employers include educating employees on safety and misuse of opioids, training employees on how to handle OUD in the workplace, providing a safe and inclusive environment for all employees, staying up to date on health care and pharmacy benefit plans, and creating a welcoming and supportive work setting.4 Interestingly, if an employee seeks rehabilitation for opioid abuse, 41% of employers state they would allow the employee back to work.9 The NSC developed a Substance Use Cost Calculator that allows companies to estimate OUD-associated costs affiliated with substance abuse (eg, absenteeism, turnover, health care costs). The CDC Foundation used the calculator and found that a construction company with 450 employees could save $166,409 annually.29 Thus, for the collective health of the nation, support of the US workforce, and for the sustainability of the US economy, educating employers, employees, and all those influenced by OUD is important for finding solutions to the opioid epidemic.4
Conclusions
The opioid crisis has become a major economic burden in the US, and as the crisis progresses, the number of cases and associated costs of OUD have become substantially greater. Treatments for OUD such as MAT, are economical when compared to the costs associated with lost productivity, absenteeism, and health care expenses. Increased awareness of OTPs can potentially help alleviate the burden of this epidemic and help employees return to the workforce and employers manage costs and productivity.
References
- 2019 Annual surveillance report of drug-related risks and outcomes — United States. Surveillance special report. CDC website. Published November 1, 2019. Accessed October 8, 2020. cdc.gov/drugoverdose/pdf/pubs/2019-cdc-drug-surveillance-report.pdf
- What is the U.S. opioid epidemic? U.S. Department of Health and Human Services website. Updated September 4, 2019. Accessed October 8, 2020. hhs.gov/opioids/about-the-epidemic/index.html
- Opioids. National Institute on Drug Abuse (NIDA) website. Accessed October 8, 2020. drugabuse.gov/drug-topics/opioids
- Opioids at work employer toolkit. NSC website. Accessed October 8, 2020. nsc.org/opioidsatwork
- Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358-367. doi: 10.1097/ADM.0000000000000166
- Key substance use and mental health indicators in the United States: results from the 2018 national survey on drug use and health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Published August 2019. Accessed October 8, 2020. samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf
- Council of Economic Advisors. The underestimated cost of the opioid crisis. White House website. Published November 2017. Accessed October 8, 2020. whitehouse.gov/sites/whitehouse.gov/files/images/The%20Underestimated%20Cost%20of%20the%20Opioid%20Crisis.pdf
- Davenport S, Weaver A, Caverly M. Economic impact of non-medical opioid use in the United States. SOA website. Published October 2019. Accessed February 7, 2020. soa.org/globalassets/assets/files/resources/research-report/2019/econ-impact-non-medical-opioid-use.pdf
- Poll: 75% of employers say their workplace impacted by opioid use. NSC website. Published March 17, 2019. Accessed October 8, 2020. nsc.org/in-the-newsroom/poll-75-of-employers-say-their-workplace-impacted-by-opioid-use
- National employer survey 2019. Opioid usage in the workplace. NSC website. Published February 2019. Accessed October 8, 2020. nsc.org/Portals/0/Documents/NewsDocuments/2019/PPW-survey-methodology.pdf?ver=2019-03-18-174024-837
- Johnston SS, Alexander AH, Masters ET, et al. Costs and work loss burden of diagnosed opioid abuse among employees on workers compensation or short-term disability. J Occup Environ Med. 2016;58(11):1087-1097. doi: 10.1097/JOM.0000000000000865
- Rice JB, Kirson NY, Shei A, et al. Estimating the costs of opioid abuse and dependence from an employer perspective: a retrospective analysis using administrative claims data. Appl Health Econ Health Policy. 2014;12(4):435-446. doi: 10.1007/s40258-014-0102-0
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657-667. doi: 10.1111/j.1526-4637.2011.01075.x
- Cox C, Rae M, Sawyer B. A look at how the opioid crisis has affected people with employer coverage. Peterson-Kaiser Family Foundation Health System Tracker website. Published April 5, 2018. Accessed October 8, 2020. healthsystemtracker.org/brief/a-look-at-how-the-opioid-crisis-has-affected-people-with-employer-coverage/
- The cost of drug and alcohol rehab in 2019. National Drug Helpline website. Accessed October 8, 2020. drughelpline.org/rehab-cost/
- US Federal Statues. TRICARE; Mental Health and Substance Use Disorder Treatment. Volume 81, Number 20. DOD-2015-HA-0109, p 5061-5085. RIN 0720-AB65, October 3, 2016.
- Medication and counseling treatment. SAMHSA website. Updated February 12, 2020. Accessed October 8, 2020. samhsa.gov/medication-assisted-treatment/treatment
- Medications to treat opioid use disorder. National Institute on Drug Abuse (NIDA) website. Updated June 2018. Accessed October 8, 2020. drugabuse.gov/publications/research-reports/medications-to-treatopioid-addiction/overview
- How much does opioid treatment cost? National Institute on Drug Abuse (NIDA) website. Updated June 2018. Accessed October 8, 2020. drugabuse.gov/publications/research-reports/medications-to-treat-opioid-addiction/how-much-does-opioid-treatment-cost
- Tiesman HM, Konda S, Cimineri L, Castillo DN. Drug overdose deaths at work, 2011-2016. Inj Prev. 2019;25(6):577-580. doi: 10.1136/injuryprev-2018-043104
- National census of fatal occupational injuries in 2018. Bureau of Labor Statistics (BLS) website. Published December 17, 2019. Accessed October 8, 2020. bls.gov/news.release/pdf/cfoi.pdf
- Goplerud E, Hodge S, Benham T. A substance use cost calculator for US employers with an emphasis on prescription pain medication misuse. J Occup Environ Med. 2017;59(11):1063-1071. doi: 10.1097/JOM.0000000000001157
- Pensa MA, Galusha DH, Cantley LF. Patterns of opioid prescribing and predictors of chronic opioid use in an industrial cohort, 2003 to 2013. J Occup Environ Med. 2018;60(5):457-461. doi: 10.1097/JOM.0000000000001231
- Hegmann KT, Weiss MS, Bowden K, et al. ACOEM practice guidelines: opioids and safety-sensitive work. J Occup Environ Med. 2014;56(7):e46-e53. doi: 10.1097/JOM.0000000000000237
- Reisfield GM, Shults T, Demery J, Dupont R. A protocol to evaluate drug-related workplace impairment. J Pain Palliat Care Pharmacother. 2013;27(1):43-48. doi: 10.3109/15360288.2012.753975
- The proactive role employers can take: opioids in the workplace. NSC website. Updated March 24, 2019. Accessed October 8, 2020. nsc.org/Portals/0/Documents/RxDrugOverdoseDocuments/RxKit/The-Proactive-Role-Employers-Can-Take-Opioids-in-the-Workplace.pdf
- Preventing opioid and drug impairment in transportation act, S.2979. Congress.gov website. Published December 4, 2019. Accessed October 8, 2020. congress.gov/bill/116th-congress/senate-bill/2979/text
- NSC releases new employer opioid toolkit, calls on employers to take major action to address opioid overdose. NSC website.Published September 18, 2019. Accessed February 10, 2020. nsc.org/in-the-newsroom/-nsc-releases-new-employer-opioid-toolkit-calls-on-employers-to-take-major-action-to-address-opioid-overdose
- Opioid misuse impacts employees’ lives, costs, business big bucks. CDC Foundation website. Updated August 1, 2017. Accessed October 8, 2020. cdcfoundation.org/blog-entry/opioid-misuse-impacts-employees-lives-costs-business-big-bucks

