- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Eating Disorder Claim Lines Rose 65% Across Nation From 2018 to 2022
A white paper from FAIR Health found that claim lines and telehealth usage for eating disorders had increased in a span of 4 years.
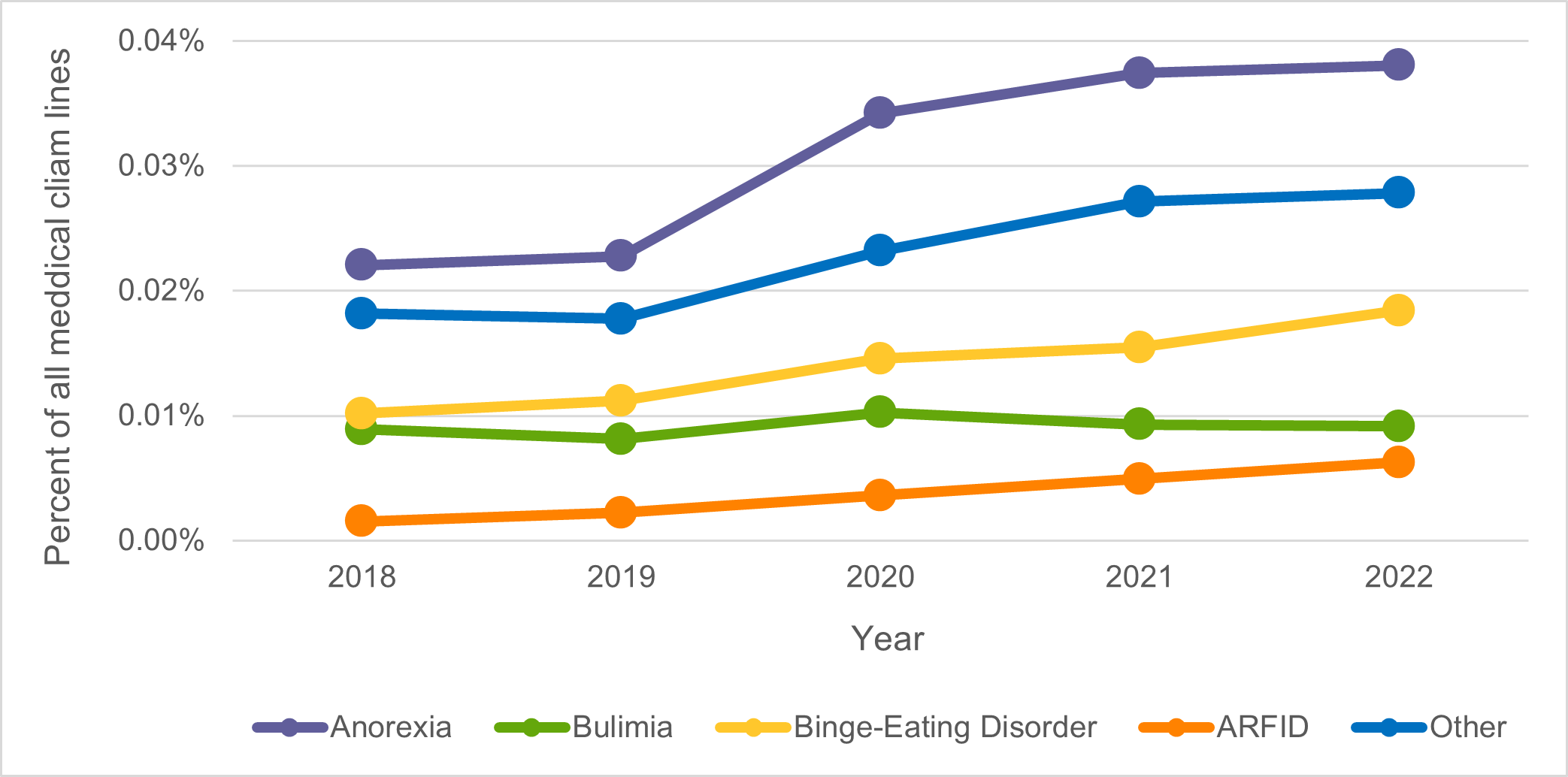
From 2018 to 2022, eating disorder claim lines increased 65% nationally as a percentage of all medical claim lines. All eating disorders studied increased during this period, but at different rates: avoidant/restrictive food intake disorder (ARFID) by 305%, binge-eating disorder by 81%, anorexia nervosa (anorexia) by 73%, and bulimia nervosa (bulimia) by 3%. These and other findings on eating disorders are reported in a FAIR Health white paper released today: Spotlight on Eating Disorders: An Analysis of Private Healthcare Claims.
Figure 1. Claim Lines for Specific Eating Disorders as a Percentage of All Medical Claim Lines, 2018-2022
Eating disorders are a diverse group of mental health conditions associated with severe disturbances in eating behaviors. In this white paper, FAIR Health delves into its repository of over 43 billion private health care claim records—the largest such database in the nation—to shed new light on eating disorders from 2018 to 2022. The study examines changes in the percentage of claim lines for eating disorders over time at national and regional levels, as well as states, age and gender, places of service, specialties and co-occurring mental health conditions. Among the key findings:
In the period 2018-2022, 72% of patients with eating disorders were also diagnosed with 1 or more co-occurring mental health conditions that were not eating disorders. This ranged from 65% of ARFID patients to 78% of bulimia patients, the highest such percentage with 1 or more co-occurring mental health conditions. Over 20% of patients with eating disorders also had a substance use disorder.
A total of 41% of patients with an eating disorder also had a diagnosis for generalized anxiety disorder, and 39% had a diagnosis for major depressive disorder. They are not exclusive categories; 1 person could have both diagnoses.
Patients with eating disorders in the period 2018-2022 were over 5 times as likely to have a mental health condition (that was not an eating disorder) and over 4 times as likely to have a substance use disorder as all patients who received medical services.
In 2022, binge-eating disorder was the eating disorder most commonly diagnosed without other accompanying eating disorders; 24.3% of all eating disorder patients were diagnosed with binge-eating disorder as the only eating disorder. This was closely followed by anorexia only, which accounted for 24.1%. Bulimia, without any other eating disorder, accounted for 6.2% of all eating disorder patients, and ARFID for 5.3%. Multiple eating disorders were diagnosed in 10.1% of patients.
The increase in eating disorder claim lines as a percentage of all medical claim lines varied by US census region from 2018 to 2022. The largest increase was in the South (84%), where eating disorders accounted for the lowest percentages of medical claim lines among all regions in both 2018 and 2022. The smallest increase was in the Northeast (51%), where eating disorders accounted for the highest percentage of medical claim lines in 2018, but the second highest percentage in 2022, when the West had the highest percentage.
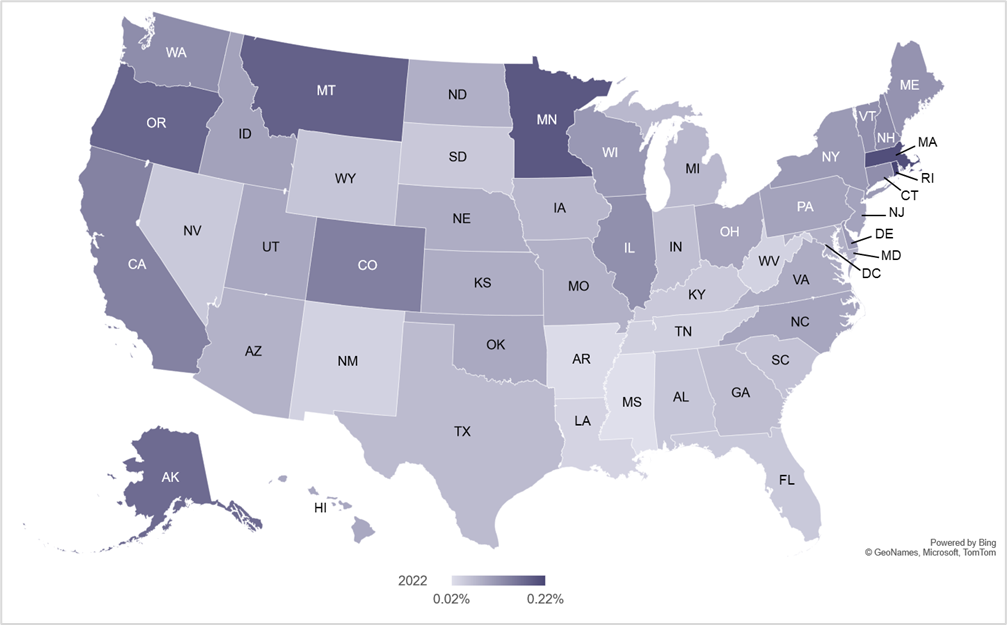
In 2022, eating disorder claim lines as a percentage of all medical claim lines varied by state. The top 5 states, highest to lowest, were all states in northern latitudes: Rhode Island, Massachusetts, Minnesota, Montana and Oregon. The bottom five states, lowest to highest, were all states in southern latitudes: Mississippi, Arkansas, Louisiana, New Mexico and West Virginia.
Figure 2. Eating Disorder Claim Lines as a Percentage of Medical Claim Lines by State, 2022
From 2018 to 2022, the age distribution of eating disorder claim lines changed. The largest share in 2018 was accounted for by the age group 19-24 and the second largest by the age group 14-18; in 2022, those positions were reversed, with the largest share associated with individuals 14-18 and the second largest with those 19-24.
Different eating disorders had different age distributions in the period 2018-2022. For example, ARFID was the eating disorder that most affected the youngest age groups (0-9 and 10-13), while binge-eating disorder most affected older age groups (31-40, 41-50 and 51-65).
In every year from 2018 to 2022, females accounted for more than 89% of eating disorder claim lines, compared with less than 11% for males. In 2022, the age group 0-9 was the only age group that had more males than females associated with eating disorder claim lines. Gender disparities for specific eating disorders in 2022 ranged from 94% female, 6% male for anorexia, to 68% female, 32% male for ARFID.
Telehealth utilization for treatment of eating disorders increased by over 10,000% from 2018 to 2022, making telehealth the most common place of service for eating disorders in 2022. During the same period, office-based health care utilization for eating disorders fell by 55%, and offices declined from the number 1 place of service in 2018 to number 2 in 2022.
Among the top 10 specialties treating patients with eating disorders, the greatest increase from 2018 to 2022 was for services by psychiatric nurses, which rose by 108%. This increase was part of a larger trend of increases in the percentage of services for eating disorders rendered by nonphysician professionals.
For the complete white paper, click here.
