- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Early Relapse Shows Powerful Prognostic Value in Multiple Myeloma
Researchers identified an optimal early relapse time point to incorporate into traditional risk features and formed a novel prognostic classification utilizing both static and dynamic risk.
While survival outcomes in multiple myeloma have improved in recent years, patients with newly diagnosed multiple myeloma (MM) nearly always relapse. Deep remission, or undetectable minimal residual disease (MRD), is a prognostic factor in overall survival (OS), and so is the length of remission.
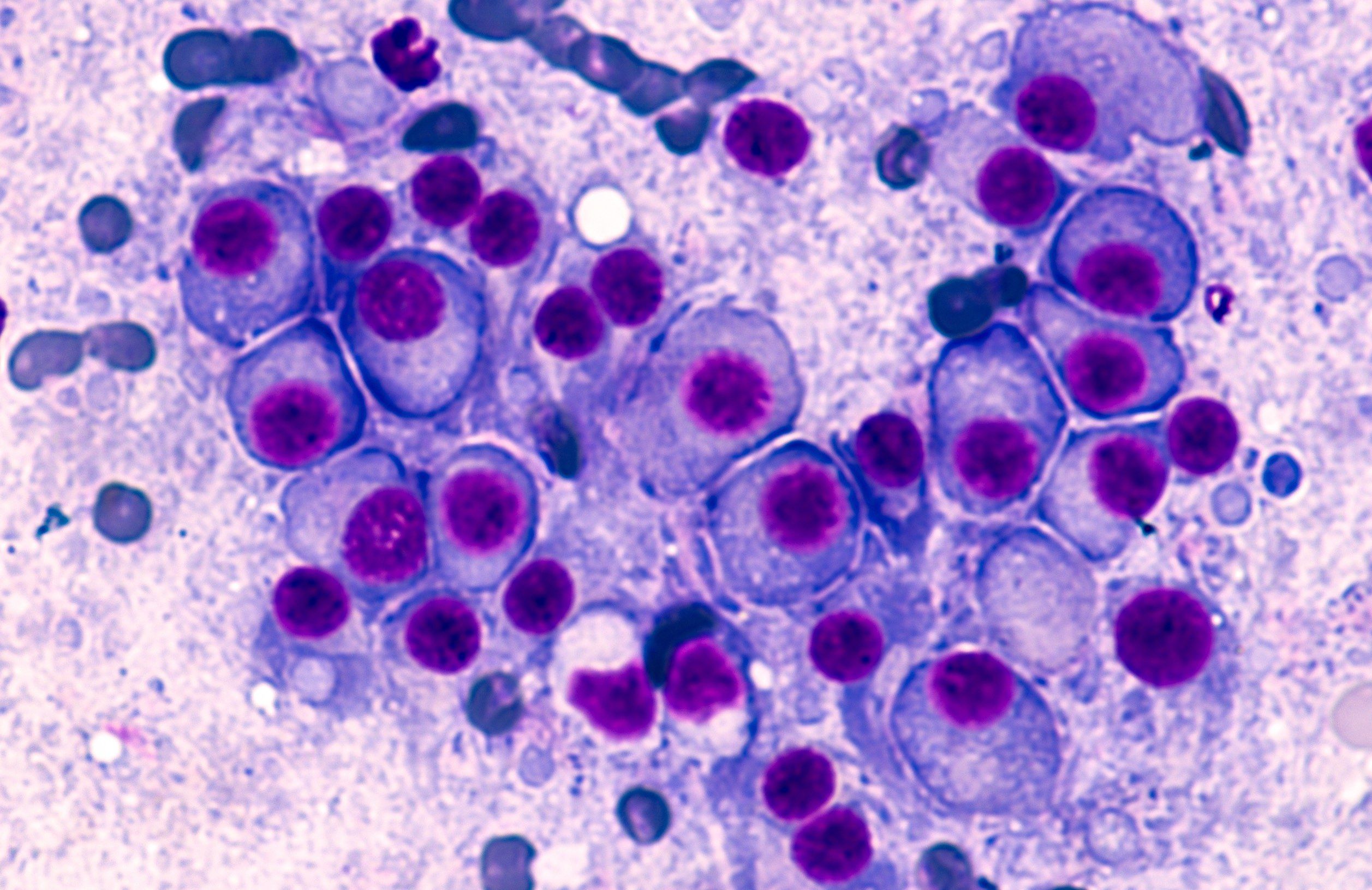
Multiple myeloma cells | Image credit: David A Litman - stock.adobe.com
Several studies have indicated early relapse (ER) is associated with shorter survival after stem cell transplantation (SCT) or novel agents, but the definitions of ER have varied. In a recent study published in Cancer, researchers sought to determine the optimal ER time point to incorporate into traditional risk features and form a novel prognostic classification utilizing both static and dynamic risk.
“Regarding the huge heterogeneity of MM, many risk staging systems for prognosis had been developed and validated to discriminate NDMM patients with distinct prognoses. Nevertheless, all of these predictive models are still based on static risk features at diagnosis including tumor burden index and cytogenetic abnormalities,” the authors wrote. “Importantly, risk distribution should be considered as a dynamic concept in MM. In fact, initial and dynamic risk profiles have not yet been integrated effectively in MM.”
A total of 629 patients with newly diagnosed MM were included in the analysis. Data from the National Longitudinal Cohort of Hematological Diseases in China were used in the study, with patients who had primary refractory disease and those without follow-up data excluded.
First, the authors summarized available data and determined that relapse within 18 months from initial treatment or 12 months from SCT were the typical definitions of ER in most studies. Then, they assessed 3 time points—12 months (ER12), 18 months (ER18), and 24 months (ER24)—in the study population and discriminated risk of death after different induction treatments.
The data showed that 18 months was the best time point to balance the bias of ER definitions for patients with or without SCT and was best for identifying early progression and dynamic high risk based on several findings:
- The discrimination ratio of ER18 (19.4%) was higher and more reasonable than that of ER12 (10.3%) and ER24 (28.0%)
- Estimated hazard curves showed a peak risk of relapse between 12 to 18 months after initial treatment in the cohort
- Median time from diagnosis to SCT was 6.6 months, and patients whose disease relapsed within 12 months after SCT were integrated into the ER18 population
In the study population overall, the median age was 58 years. The median follow-up was 38.8 months, and the median OS was 72.3 months. High‐risk cytogenetic abnormalities (HRCAs) were noted in 27.9% of patients, 45.1% were classified as International Staging System (ISS) stage III, and 19.5% were classified as Revised ISS (R‐ISS) stage III. All of the patients included in the study were treated with novel agents as induction treatment, and 182 (28.9%) underwent autologous SCT.
Patients in the ER18 cohort showed more aggressive disease features and worse responses compared with a reference population. These patients also showed a shorter median OS of 28.9 months compared with 85.6 months in the reference population (P < .001). Those in the ER18 group were also at a higher risk of death, with a hazard ratio (HR) of 6.32 (95% CI, 4.603-8.739; P < .001).
A multivariate analysis that included R18, ISS stages, elevated LDH, thrombocytopenia, HRCAs, upfront ASCT, and best response to the first‐line treatment as variables, the researchers confirmed that the most significant time point in terms of OS prognostic value in the cohort was ER18 (HR, 4.467; P < .001).
“These data indicate that the dynamic high‐risk factor during treatment (ER18) plays a vital role in the survival of patients with newly diagnosed MM,” the authors wrote.
The correlation between ER18 and R-ISS–determined risk was explored, and the frequency of ER18 was found to increase with poorer R-ISS stage. Furthermore, the investigators found that even patients who were classified as stage I or II by R-ISS standards were likely to experience ER18 and have worse OS outcomes.
“These findings underscore the intrinsic prognostic heterogeneity among patients in different R‐ISS stages and highlight the limitations of relying solely on single risk stratification at diagnosis,” the authors wrote.
A second-state model, a combination of the ER18 and R-ISS, was proposed to predict dynamic risk changes, highlighting the potential role of ER18 as a complementary measure to R-ISS risk classification that could facilitate more individualized care.
The study was limited by its retrospective nature, although the patient cohort was large and heterogeneous, the authors noted. The induction treatments also did not include monoclonal antibodies, which might extend prognosis based on clinical trials. Further studies are also needed to evaluate the proposed multi-state risk model.
“Collectively, integration of R‐ISS with ER18 represents a static and dynamic assessment of patient prognosis to more accurately identify those patients with poor prognosis who are in urgent need of novel therapeutic strategies,” the authors concluded.
Reference
Yan W, Xu J, Fan H, et al. Early relapse within 18 months (ER18) is a powerful dynamic predictor for prognosis and could revise static risk distribution in multiple myeloma. Cancer. Published online October 17, 2023. doi:10.1002/cncr.35056
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
