- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Driving Persistence Among Patients Affected by Copay Accumulators With Patient-Centric Support
The authors, from RxCrossroads by McKesson, discuss the impact of copay accumulator and maximizer programs.
Steve Mink is vice president of Product Development and Arran Standring is director of Analytics & Insights, RxCrossroads by McKesson
Specialty therapies are an important treatment option for cancer and other complex diseases; however, they can also be expensive for patients. In an effort to contain costs associated with specialty drugs, pharmacy benefit managers (PBMs) and health plans have increasingly implemented copay accumulator plans which require patients with high-deductible health plans (HDHP) to pay a larger share of the cost for specialty medications.
As the financial burden shifts to patients, many rely on biopharma-sponsored copay programs to help afford their medication and stay adherent to the treatment regimen. However, copay accumulator plans often prevent copay savings benefits from counting towards a patient’s annual deductible and out-of-pocket maximum. This can have a significant impact on patient adherence to medication regimens.
Copay accumulators during the COVID-19 pandemic
Since copay accumulators typically affect patients in employer-based or commercial insurance plans, the impact of copay accumulators during the COVID-19 pandemic is more focused on access and choice. Patients who run out of biopharma copay assistance due to accumulator impacts are forced to decide between three tough options. First, they can try to bear the financial burden and pay full price for their medication. Second, they may discontinue taking the medication, which can have significant impact on their health. Finally, they may try to switch drugs but would not be able to without visiting their doctor to get a new prescription. However, access to care during COVID-19 is limited, and patients with compromised health or immune systems are likely not comfortable with the idea of going to the doctor’s office right now.
We have heard that some payers are suspending or eliminating copay accumulator programs to ensure patients have uninterrupted access to drugs during the COVID-19 pandemic. While we have not seen evidence of this in our data yet, we would certainly welcome that as an important step to help prescribers maintain the ability to choose the right medication for their patients during this pandemic.
Tools to help patients remain adherent
In 2017, health plan sponsors began launching copay accumulator programs, and the number of patients affected spiked in 2017 and 2018. While accumulator plans did not grow as rapidly in 2019, the number remained steady. As legislators and CMS tried to mitigate the impact of accumulator plans, copay maximizer plans grew significantly in 2019. Copay maximizer plan amounts are determined based on the value of biopharma-funded copay assistance rather than the list price of the drug.While these plans do not have the same impact on patient adherence as copay accumulators, they shift the financial burden from payers to the biopharma companies and do not offer relief to patients on their annual deductibles and out-of-pocket maximums. Products incorporated into maximizer plans have been deemed “non-essential health benefit specialty drugs” and have been removed from plan coverage instead requiring cash payments or fully burdening the biopharma copay programs. According to the National Business Group of Health, in the next 2 years, accumulators and maximizers are expected to expand from approximately 25% of US employers to as many as 50%.
The impact of copay accumulator and maximizer programs is real and significant. It forces painful choices on patients living with chronic and complex conditions who often have no comparable alternatives for their medications. For example, a mother of 2 was diagnosed with multiple sclerosis and tried two different therapies before switching to a sphingosine 1-phosphate receptor modulator, which finally slowed disease progression and gave her a better quality of life. Under the copay savings program she enrolled, the biopharma company covered costs up to $18,000 per year, applied directly toward her $10,000 pharmacy deductible. When a copay accumulator was implemented, and the copay savings no longer counted toward her deductible, she was responsible for the 20% copay and the $9000 deductible. If she wished to continue treatment, she would have to choose between paying for her medication and incurring huge debt or using her children’s college savings.
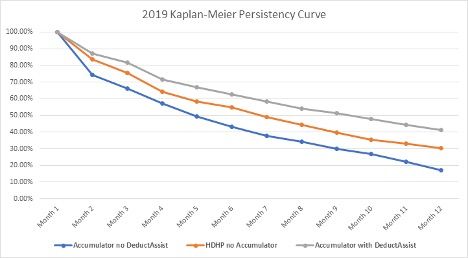
According to RxCrossroads by McKesson’s data and research, patients impacted by accumulator programs fill 1.5 times less than patients in HDHPs. More importantly, accumulator patients have a ~13% drop in persistence between month 3 and month 4, as they reach the cap for annual benefits and drop off therapy. Decreased persistency can lead to poorer health outcomes and push patients towards having to choose a therapy that may be less effective.
Ultimately, providers want their patients on medications that are essential for them, and patients need to be able to afford those medications to have better outcomes. For patients in a HDHP, biopharma sponsored co-pay programs are an essential part of affording the medicines that have been prescribed by their physician. Providing patient-centric support to those affected by an accumulator program, biopharma companies can uncover challenges the patient may be facing and help the patient with a variety of options for supporting patient affordability. Educating patients about their options could be critical to impacting adherence and helping patients increase their persistency.
