- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Detection and Management of Autoimmune Disease–Associated Interstitial Lung Diseases
ABSTRACT
Interstitial lung disease (ILD) causes significant morbidity and mortality in patients with systemic autoimmune rheumatic diseases. Patients at high risk of ILD should be screened using high-resolution CT (HRCT), but there is no consensus as to which risk factors—or combination of risk factors—should prompt referral for HRCT. The course of autoimmune disease–associated ILD is highly variable, and it may not mirror the activity of the underlying autoimmune disease. Patients require close monitoring with periodic pulmonary function testing and symptom assessment and with repeat HRCT considered based on clinical assessment. The relevance of clinical and radiologic signs of progression—and their implications for management—ideally should be discussed by a multidisciplinary team. Management of autoimmune disease–associated ILD may involve immunosuppressant and/or antifibrotic therapy in addition to supportive care. It is important that treatment decisions be individualized to the needs and wishes of the patient. Regular follow-up is important to monitor disease progression and manage the adverse effects related to treatment.
Am J Manag Care. 2024;30:S114-S121. https://doi.org/10.37765/ajmc.2024.89633
For author information and disclosures, see end of text.
Introduction
Interstitial lung disease (ILD) is a common complication of systemic autoimmune rheumatic diseases1-5 and a cause of significant morbidity and mortality in affected patients.1,6-8 Progression of ILD and the development of lung fibrosis is associated with particularly poor outcomes.1,6,9-11 It is important that ILD is detected promptly and that patients with this diagnosis are monitored closely and managed appropriately; however, ILD may be asymptomatic or present with nonspecific symptoms that are attributed to other manifestations of autoimmune disease or to comorbidities.2,6 This commonly results in delays in its identification,12-14 and lung function may be substantially impaired by the time that ILD is diagnosed.15,16
This article discusses the detection, monitoring, and management of autoimmune disease–associated ILDs with a particular focus on guidelines recently issued by professional associations.
Screening for ILD in Patients With Autoimmune Diseases
The poor outcomes associated with ILD have generated debate about the potential benefits of screening in patients with autoimmune diseases. The high prevalence of autoimmune diseases—particularly rheumatoid arthritis (RA)—limits the feasibility of screening all patients with autoimmune disease for ILD. Screening therefore must be guided by assessment of risk factors. The risk of ILD varies depending upon the autoimmune disease involved; the highest risk has been observed in patients with systemic sclerosis (SSc) and mixed connective tissue disease (MCTD).17 Several demographic, clinical, serologic, and genetic risk factors for the development of ILD have been identified4,18-20; however, the absolute risk associated with specific characteristics has not been established, and ILD may develop even when there are no obvious risk factors.
ILD may be present in the absence of respiratory symptoms,2,6,21 so waiting for patients to develop symptoms may result in delayed detection of ILD. Results from pulmonary function tests (PFTs) such as forced vital capacity (FVC) assist in identifying patients with impaired lung function; however, these tests are much less sensitive for detecting ILD than is high-resolution CT (HRCT).22-24
In a study of 212 patients with early diffuse cutaneous SSc, 37% of patients who had ILD on HRCT had an FVC of 80% or more of the predicted value23; however, detection of ILD solely by HRCT and in the absence of symptoms or evidence of recent progression raises the question of whether treatment is warranted. Close monitoring may be an appropriate course of action in some patients, but risk factors for progression and the patient’s preferences should considered. Of note, ILD may develop so early in the course of autoimmune disease that it is the first manifestation to be detected.25,26
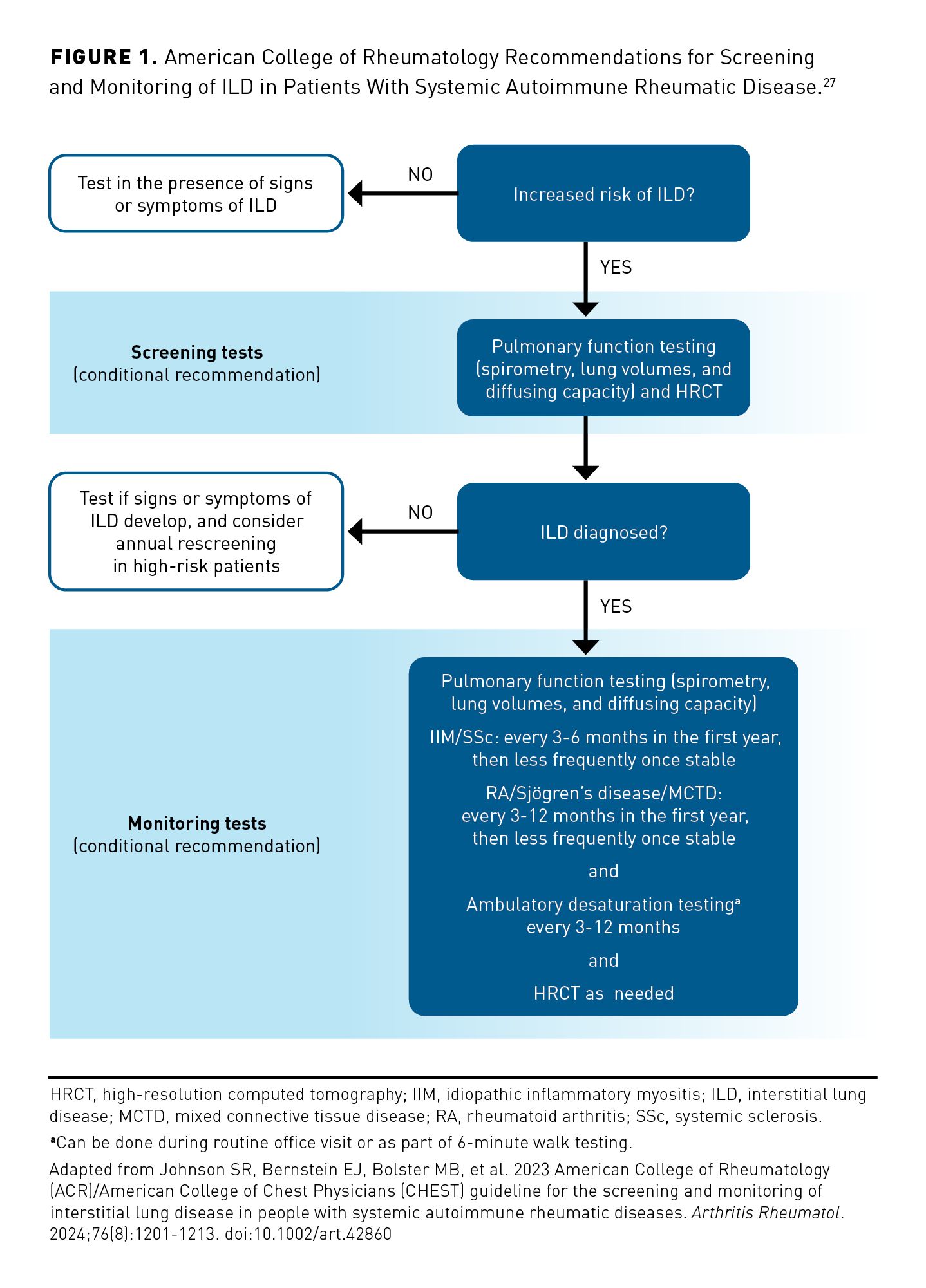
Practice guidelines recently issued by the American College of Rheumatology (ACR) conditionally recommended screening for ILD with both HRCT and PFTs (FVC, lung volume, diffusing capacity for carbon monoxide [DLCO]) in people with newly diagnosed autoimmune disease who are at increased risk of ILD (Figure 1).27 These guidelines provide a list of risk factors for ILD, but they do not specify which risk factors detected alone or in combination should prompt screening.28 Consensus statements issued by experts in Spain and Austria recommended screening for ILD using HRCT and PFTs in patients with RA who have risk factors or respiratory symptoms; again, however, they did not define risk factors that should lead to screening.29,30 Consensus statements issued by experts in Europe31 and the US32 have recommended that all patients with SSc be screened for ILD at diagnosis using HRCT, that PFTs also be performed, and that repeat HRCT be guided by risk factors, lung function, and symptoms.
ILD is associated with distinct sounds on chest auscultation, which often are described as Velcro-like crackles.33 Experts have recommended that auscultation of the chest be performed at diagnosis in patients with SSc32 and RA.29,31 A case could also be made for chest auscultation on diagnosis of other autoimmune diseases, particularly in patients with risk factors for ILD; nevertheless, chest auscultation was not included in the recommendations recently issued by the ACR.27
Concerns over the cost and radiation exposure associated with HRCT have generated interest in lung ultrasound as a risk stratification tool for identifying patients who should undergo HRCT. Recent study results have demonstrated that lung ultrasound has high specificity and sensitivity for the detection of ILD compared with HRCT in patients with SSc34-37 and RA.38,39 In a study of 180 patients with autoimmune diseases, the sensitivity and specificity of ultrasound performed by an experienced examiner to detect ILD relative to HRCT were 99% and 96%, respectively.40 However, the use of lung ultrasound to detect ILD requires training, and guidelines for its use to detect ILD in patients with autoimmune diseases have not yet been issued by any professional association.
Monitoring Patients With Autoimmune Disease–Associated ILDs
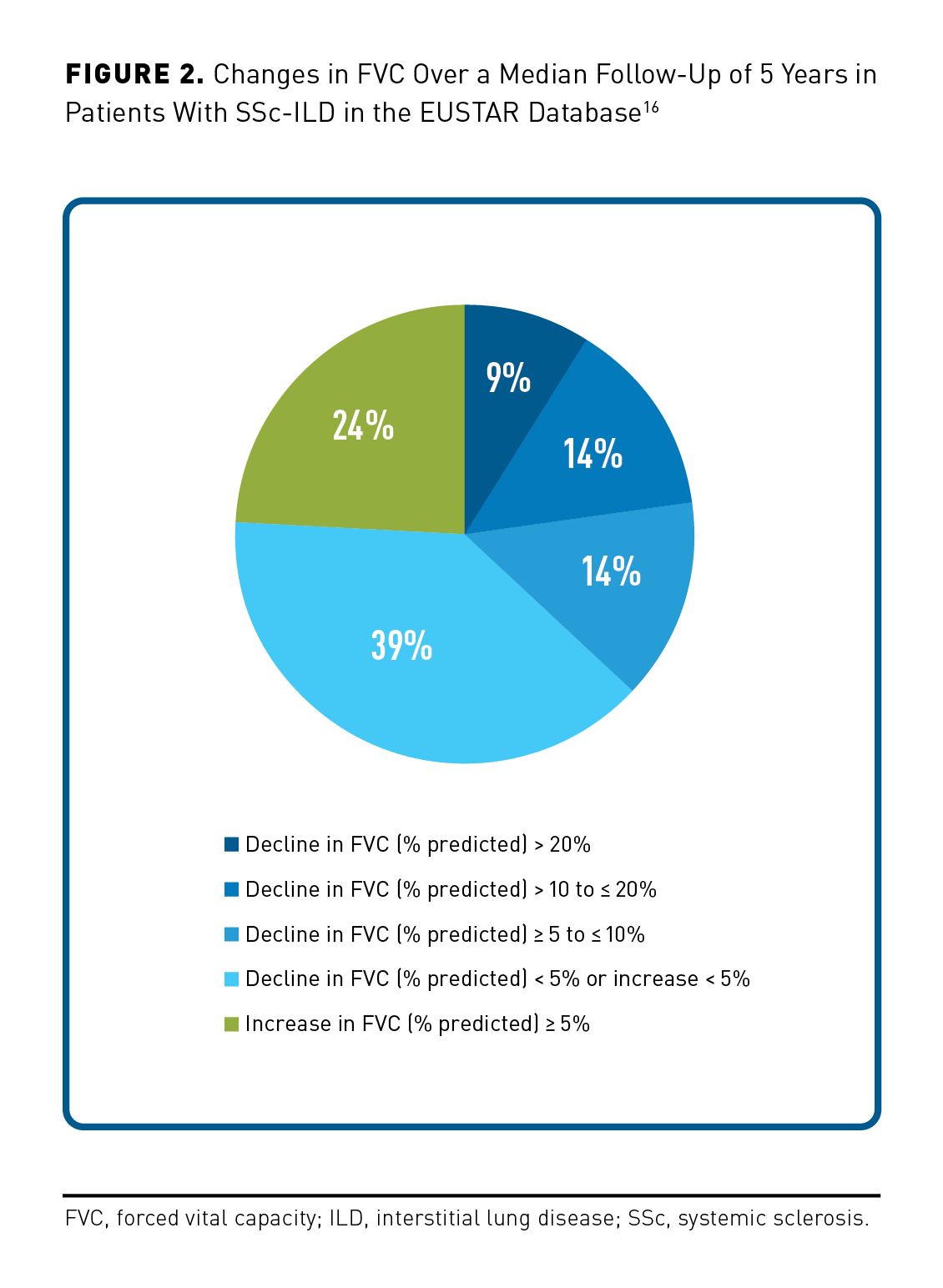
The course of autoimmune disease–associated ILDs varies greatly between patients. Some decline slowly, whereas others exhibit rapid progression.16,41,42 Over several years of follow-up, a patient may experience periods of deterioration, stability, or even improvement in lung function (Figure 2).16,42,43 Progression of ILD may not mirror the activity of the underlying autoimmune disease42; thus, stable or improving joint or skin disease does not necessarily indicate that a patient’s ILD is stable.
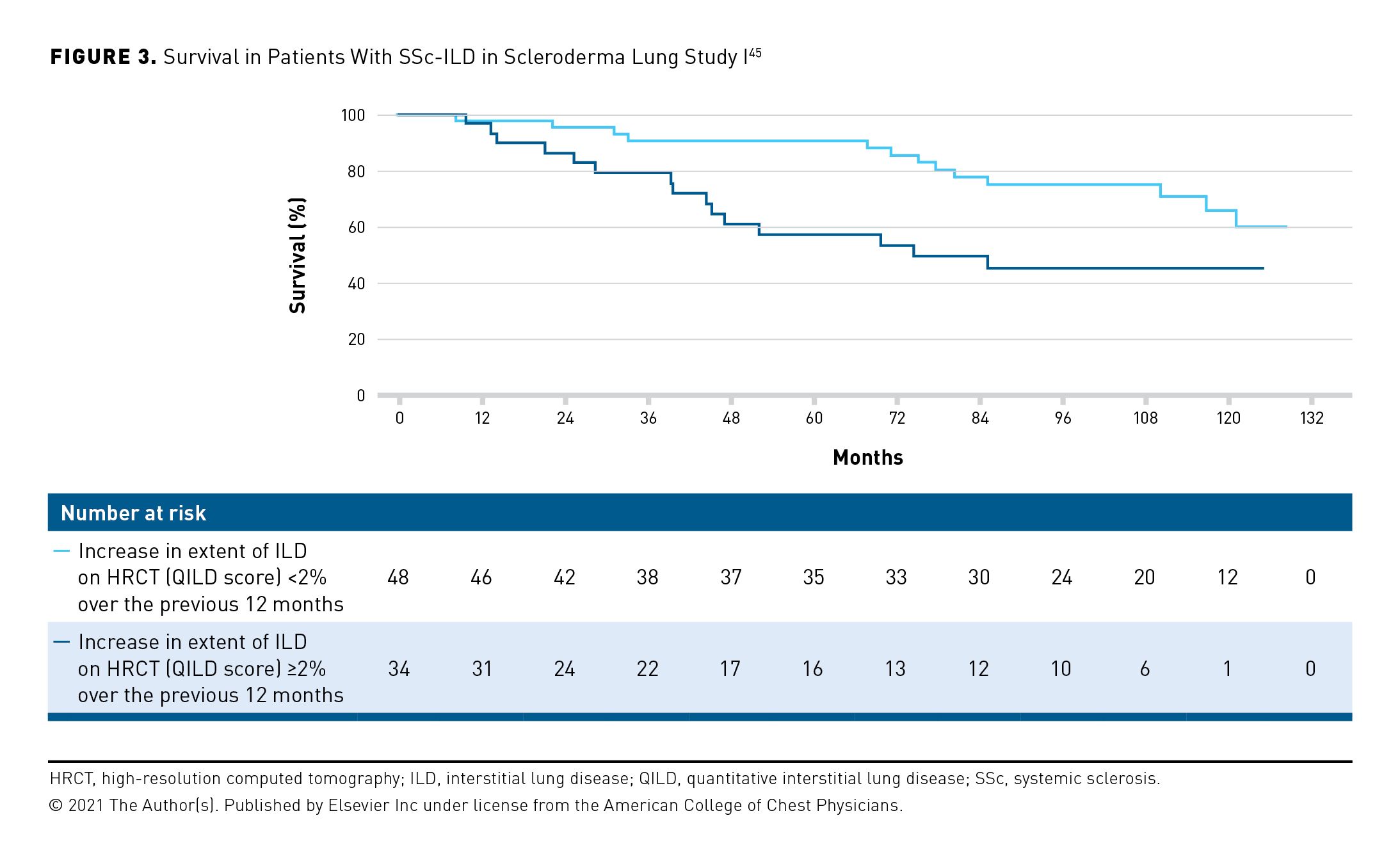
A decline in FVC or DLCO or an increase in the extent of ILD on HRCT indicates progression and is associated with an increased risk of mortality.6,9,10,44,45 In a retrospective analysis of data from 137 patients with RA-ILD followed for a median of 5 years, a decline in FVC (% predicted) of at least 10% was associated with a 2.5-fold increased risk of mortality (P <.0001).9 In a retrospective analysis of data from 162 patients with SSc-ILD followed for 15 years, a decline in FVC (mL) of 10% or more over 12 months was associated with a 1.8-fold greater risk of subsequent mortality (P = .01).10 In Scleroderma Lung Study I, patients who had an increase in the extent of ILD on HRCT (assessed using the quantitative ILD [QILD] score) of at least 2% at 12 months had a greater risk of mortality over the following 12 years than did those with smaller increases in QILD score (P = .01) (Figure 3).45
Patients with autoimmune disease–associated ILDs require close monitoring so that progression can be identified promptly.27,31,32,46 The guidelines issued by the ACR conditionally recommended monitoring with PFTs every 3 to 6 months in patients with myositis-ILD or SSc-ILD and every 3 to 12 months in patients with ILD associated with RA, Sjögren disease, or MCTD for the first year and then less frequently if the disease is stable.27 Experts have recommended monitoring patients with SSc-ILD using multiple measures, including PFTs, HRCT, and symptom assessment.31,32 PFTs are also useful to detect pulmonary hypertension, which is associated with high mortality if not treated.47 Exercise tests such as the 6-minute walk and ambulatory desaturation testing (including uptitration of supplemental oxygen as necessary) can provide valuable additional information but should not be the sole tool used for monitoring autoimmune disease–associated ILDs.27,31,32 HRCT scans should be repeated as clinically indicated.27,31,32 Worsening in lung function or radiologic abnormalities may not be straightforward to interpret, and there may not be a close relationship between decline in FVC and worsening of features observed on HRCT.48,49 Ideally, the relevance of clinical and radiologic signs of progression and their implications for management should be discussed by a multidisciplinary team.50,51
In May 2022, international thoracic societies published criteria for the definition of progressive pulmonary fibrosis (PPF) in patients with fibrosing ILDs other than idiopathic pulmonary fibrosis (IPF).46 Different criteria have been used to select patients with progressive fibrosing ILDs for enrollment into clinical trials,52-54 yet criteria for the identification of PPF are generally based on categorical declines in lung function (FVC and/or DLCO [percentage predicted]), increase in radiological abnormalities, and worsening of respiratory symptoms. Patients identified based upon these criteria exhibit progressive decline in lung function and high mortality.55-57 Importantly, progression of lung fibrosis is a self-perpetuating and irreversible process.58 Evidence of progression should prompt a discussion with the patient about the worsening of their disease and consideration of initiation or escalation of treatment.
Management of Autoimmune Disease–Associated ILDs
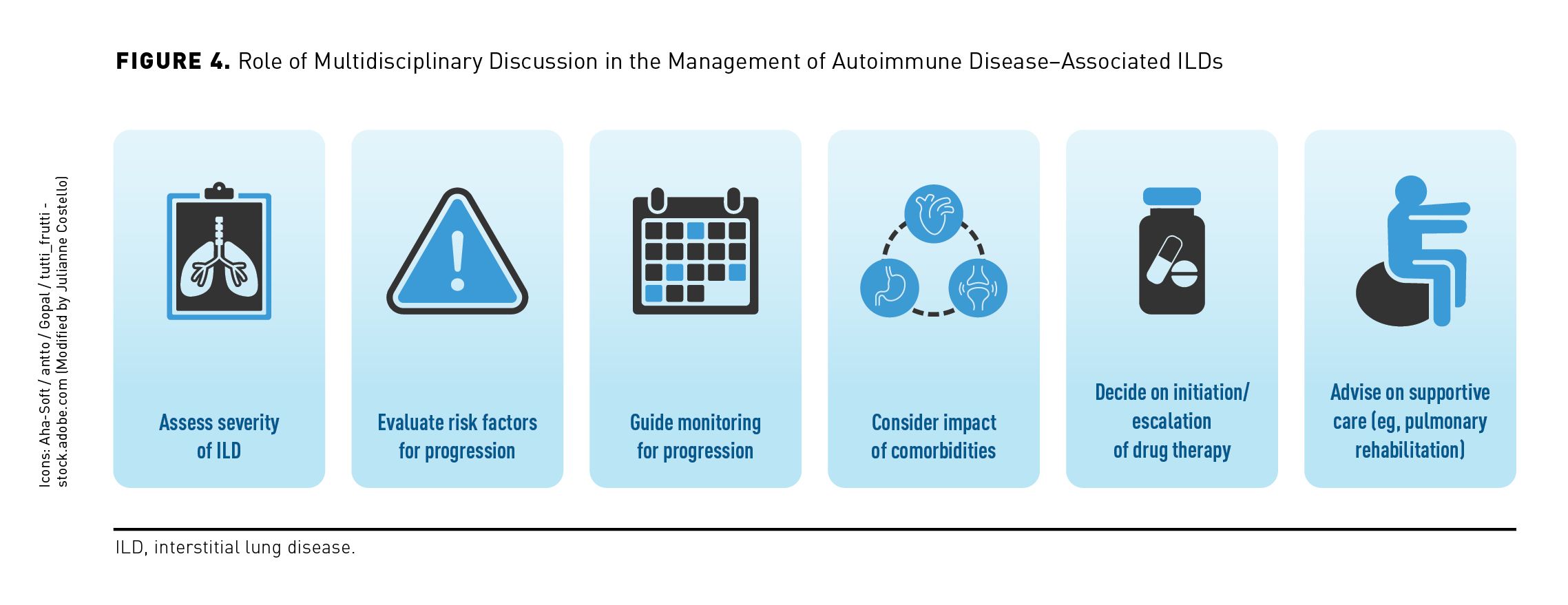
Managing autoimmune disease–associated ILDs requires a multidisciplinary approach that considers the type of autoimmune disease, the severity of the ILD and evidence of its progression, risk factors for further progression, comorbidities, and the patient’s preferences (Figure 4).59,60 Close collaboration between pulmonologists and rheumatologists is essential, whereas input from a radiologist may help identify patients at greater risk of progression.50 Specialist nurses/nurse practitioners and physical therapists can make an important contribution to the provision of patient information and supportive care.61 In deciding on a therapeutic regimen, the benefits of slowing ILD progression and potentially preventing acute exacerbations should be weighed against the risk of adverse effects (AEs).
There is no established treatment algorithm for autoimmune disease–associated ILDs, but initial standard of care employs immunosuppression. Glucocorticoids are commonly used, but their efficacy has not been demonstrated. In the guidelines issued by the ACR, conditional recommendations were made for the use of mycophenolate, azathioprine, rituximab, and cyclophosphamide as first-line treatment for autoimmune ILDs.62 The immunosuppressant mycophenolate is commonly used in the treatment of SSc-ILD based on the results of Scleroderma Lung Study II, which showed that it had similar efficacy to cyclophosphamide in preserving lung function but with a better safety profile.63 The tyrosine kinase inhibitor nintedanib and the interleukin-6 receptor antagonist tocilizumab have been approved by the FDA for slowing decline in lung function in patients with SSc-ILD. In the randomized, placebo-controlled SENSCIS trial, nintedanib therapy reduced the rate of decline in FVC (mL/year) over 52 weeks by 44% (−52.4 vs −93.3 mL/year; difference, 41.0 mL/year; 95% CI, 2.9-79.0; P = .04).64 The absolute effect of nintedanib versus placebo was numerically lower in patients taking mycophenolate at baseline than in those not taking mycophenolate (difference, 26.3 vs 55.4 mL/year), but the relative reduction was similar between these subgroups (40% and 46%, respectively).65 In the subgroup of patients with SSc-ILD in the focuSSced trial, FVC was preserved over 48 weeks in the tocilizumab group (least squares mean change in FVC % predicted, –0.1 with tocilizumab vs –6.3% with placebo; P < .0001).66 In the RECITAL trial conducted in patients with various autoimmune disease–associated ILDs, similar increases in FVC over 24 weeks were observed with rituximab and cyclophosphamide (97 and 99 mL, respectively; P = .49).67 In the EvER-ILD trial in patients with ILD and a nonspecific interstitial pneumonia pattern who were on background therapy with mycophenolate, FVC (% predicted) increased over 6 months in the rituximab group and decreased in the placebo group (1.6 vs –2.0; difference, 3.6; 95% CI, 0.41-6.80; P = .0273).68 Guidelines for the treatment of SSc-ILD recently issued by the American Thoracic Society (ATS) included a strong recommendation for the use of mycophenolate and conditional recommendations for the use of cyclophosphamide, nintedanib, tocilizumab, rituximab, and the combination of nintedanib and mycophenolate.69 In addition, autologous hematopoietic stem cell transplantation is a treatment option for a select group of patients with severe and treatment-refractory SSc. This procedure has shown benefits on long-term survival.70,71 However, it is associated with a risk of short-term mortality, and it should only be performed at experienced centers.72
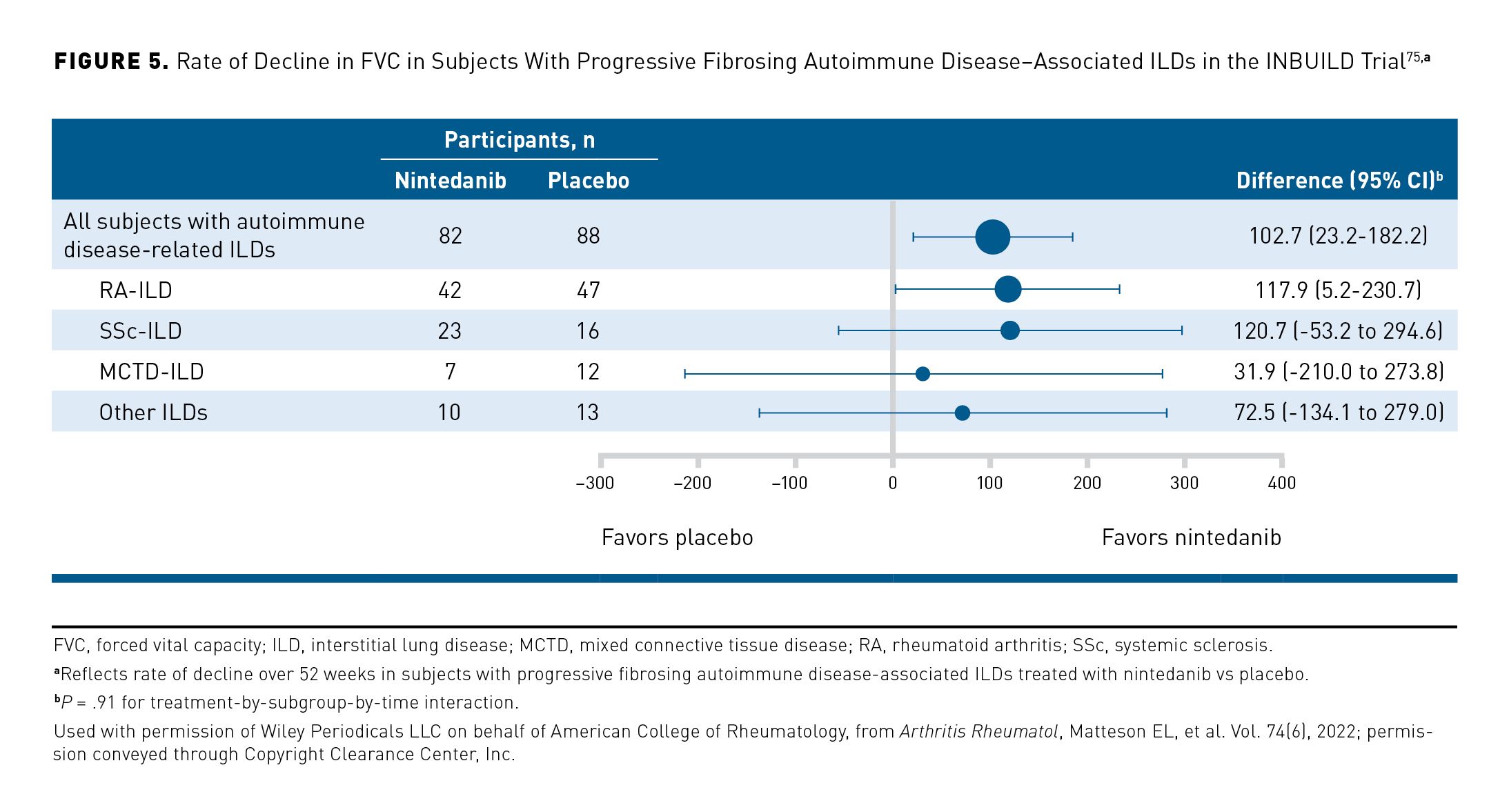
In the US, the only drug approved for the treatment of autoimmune disease–associated ILDs other than SSc-ILD is nintedanib, which is approved for the treatment of progressive fibrosing ILDs (PPF) irrespective of etiology. Nintedanib received a conditional recommendation for the treatment of PPF in patients who have failed standard management in a clinical practice guideline issued by thoracic societies including the ATS.46 In the INBUILD trial in patients with PPF, nintedanib slowed the rate of decline in FVC (mL/year) over 52 weeks by 57% versus placebo (−80.8 vs −187.8 mL/year; difference, 107.0 mL/year; 95% CI, 65.4-148.5; P <.001),52 with a consistent effect noted across patients with different disease severities73 and diagnoses (Figure 5).74,75 In the subgroup of patients with RA-ILD, nintedanib slowed the rate of decline in FVC by 59% vs placebo (difference, 116.7 mL/year; 95% CI, 7.4-226.1; nominal P = .037). AEs led to treatment discontinuation in 24% of the nintedanib group versus 17% of the placebo group; the most frequent AE leading to treatment discontinuation was an increase in alanine aminotransferase, which led to discontinuation in 7.1% of the nintedanib group and none of the placebo group.76 Data collected using the Living with Pulmonary Fibrosis questionnaire suggested that over 52 weeks, treatment with nintedanib reduced dyspnea, cough, fatigue, and the impact of ILD on patients’ lives, although these benefits were less pronounced in patients with autoimmune disease–related ILDs than in those with other ILDs.77 Data collected in real-world settings are providing more information on the utility of antifibrotic therapies in patients with autoimmune disease–associated ILDs in clinical practice.78
In addition to drug therapy, patients with autoimmune disease–associated ILDs may benefit from supportive care such as symptom management, pulmonary rehabilitation,79 and advice on strategies to minimize the impact of the disease on their lives.80 Patient support groups can be highly valuable in helping patients to manage the physical and emotional challenges of living with ILD.81 Regular follow-up is needed to manage AEs of treatment and assist patients in remaining on therapy. Patients with hypoxemia may benefit from supplemental oxygen,82 but they need support to manage the impact that oxygen therapy has on their daily lives.83 Lung transplantation should be considered for patients who meet eligibility criteria.84 Recent evidence suggests that outcomes after lung transplantation in patients with autoimmune disease–associated ILDs are similar to those in patients with IPF.85,86 Palliative and end-of-life care should be discussed with the patient as appropriate, and it should be individualized to their needs.87
Conclusions
ILD is a common complication of autoimmune disease that can cause significant morbidity and mortality. Detection of ILD is often delayed, as it may be asymptomatic or nonspecific in presentation during its early stages. Prompt detection is important to assess the severity of ILD and risk factors for its progression. Monitoring should include regular PFTs, symptom assessment, and HRCT as clinically indicated. Management of autoimmune disease–associated ILDs requires a multidisciplinary approach that depends upon the type of autoimmune disease, the severity and progression of the ILD, and the patient’s preferences. Antifibrotic and immunosuppressant therapies slow the progression of autoimmune disease–associated ILDs; however, there is no established treatment algorithm to guide the clinician. Symptom relief, pulmonary rehabilitation, and patient information and support are important elements of a holistic approach to patient care.
Acknowledgments
The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors. Editorial support was provided by Elizabeth Ng and Wendy Morris of Fleishman-Hillard, London, United Kingdom, which was contracted and funded by Boehringer Ingelheim Pharmaceuticals, Inc. Boehringer Ingelheim was given the opportunity to review the article for medical and scientific accuracy as well as intellectual property considerations.
Author Affiliations: Division of Rheumatology, Wexner Medical Center, The Ohio State University (AA), Columbus, OH; Department of Medicine, Division of Pulmonary and Critical Care, Feinberg School of Medicine, Northwestern University (AJE), Chicago, IL.
Source of Funding: This article is part of a supplement that was supported by Boehringer Ingelheim Pharmaceuticals, Inc. The authors did not receive any payment for their work on the articles. Boehringer Ingelheim was given the opportunity to review the article for medical and scientific accuracy as well as intellectual property considerations.
Author Disclosures: Dr Ajam reports participating in consultancies or paid advisory boards for Boehringer Ingelheim. Dr Esposito reports no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this supplement.
Authorship Information: Concept and design (AA, AJE); analysis and interpretation of data (AA); drafting of the manuscript (AA, AJE); critical revision of the manuscript for important intellectual content (AA, AJE).
Address Correspondence To: Anthony J. Esposito, MD. Email: anthony.esposito@northwestern.edu
REFERENCES
1. Hoffmann-Vold AM, Fretheim H, Halse AK, et al. Tracking impact of interstitial lung disease in systemic sclerosis in a complete nationwide cohort. Am J Respir Crit Care Med. 2019;200(10):1258-1266. doi:10.1164/rccm.201903-0486OC
2. Esposito AJ, Sparks JA, Gill RR, et al. Screening for preclinical parenchymal lung disease in rheumatoid arthritis. Rheumatology (Oxford). 2022;61(8):3234-3245. doi:10.1093/rheumatology/keab891
3. Samhouri BF, Vassallo R, Achenbach SJ, et al. Incidence, risk factors, and mortality of clinical and subclinical rheumatoid arthritis-associated interstitial lung disease: a population-based cohort. Arthritis Care Res (Hoboken). 2022;74(12):2042-2049. doi:10.1002/acr.24856
4. Berardicurti O, Marino A, Genovali I, et al. Interstitial lung disease and pulmonary damage in primary Sjögren’s syndrome: a systematic review and meta-analysis. J Clin Med. 2023;29;12(7):2586. doi:10.3390/jcm12072586
5. Hum RM, Lilleker JB, Lamb JA, et al. Comparison of clinical features between patients with antisynthetase syndrome and dermatomyositis: results from the MYONET registry. Rheumatology (Oxford). 2023:kead481. doi:10.1093/rheumatology/kead481
6. Marie I, Hatron PY, Dominique S, Cherin P, Mouthon L, Menard JF. Short-term and long-term outcomes of interstitial lung disease in polymyositis and dermatomyositis: a series of 107 patients. Arthritis Rheum. 2011;63(11):3439-3447. doi:10.1002/art.30513
7. Huang H, Xie W, Geng Y, Fan Y, Zhang Z. Mortality in patients with primary Sjögren’s syndrome: a systematic review and meta-analysis. Rheumatology (Oxford). 2021;60(9):4029-4038. doi:10.1093/rheumatology/keab364
8. Hyldgaard C, Bendstrup E, Pedersen AB, Pedersen L, Ellingsen T. Interstitial lung disease in connective tissue diseases: survival patterns in a population-based cohort. J Clin Med. 2021;10(21):4830. doi:10.3390/jcm10214830
9. Solomon JJ, Chung JH, Cosgrove GP, et al. Predictors of mortality in rheumatoid arthritis-associated interstitial lung disease. Eur Respir J. 2016;47(2):588-596. doi:10.1183/13993003.00357-2015
10. Goh NS, Hoyles RK, Denton CP, et al. Short-term pulmonary function trends are predictive of mortality in interstitial lung disease associated with systemic sclerosis. Arthritis Rheumatol. 2017;69(8):1670-1678. doi:10.1002/art.40130
11. Oh JH, Kim GHJ, Cross G, et al. Automated quantification system predicts survival in rheumatoid arthritis-associated interstitial lung disease. Rheumatology (Oxford). 2022;61(12):4702-4710. doi:10.1093/rheumatology/keac184
12. Alhamad EH, Cal JG, Alrajhi NN, et al. Clinical characteristics and outcomes in patients with primary Sjogren’s syndrome-associated interstitial lung disease. Ann Thorac Med. 2021;16(2):156-164. doi:10.4103/atm.atm_632_20
13. Cano-Jiménez E, Vázquez Rodríguez T, Martín-Robles I, et al. Diagnostic delay of associated interstitial lung disease increases mortality in rheumatoid arthritis. Sci Rep. 2021;11(1):9184. doi:10.1038/s41598-021-88734-2
14. Hoffmann-Vold AM, Bendstrup E, Dimitroulas T, et al. Identifying unmet needs in SSc-ILD by semi-qualitative in-depth interviews. Rheumatology (Oxford). 2021;60(12):5601-5609. doi:10.1093/rheumatology/keab154
15. Zamora-Legoff JA, Krause ML, Crowson CS, Ryu JH, Matteson EL. Patterns of interstitial lung disease and mortality in rheumatoid arthritis. Rheumatology (Oxford). 2017;56(3):344-350. doi:10.1093/rheumatology/kew391
16. Hoffmann-Vold AM, Allanore Y, Alves M, et al; EUSTAR Collaborators. Progressive interstitial lung disease in patients with systemic sclerosis-associated interstitial lung disease in the EUSTAR database. Ann Rheum Dis. 2021;80(2):219-227. doi:10.1136/annrheumdis-2020-217455
17. Joy GM, Arbiv OA, Wong CK, et al. Prevalence, imaging patterns and risk factors of interstitial lung disease in connective tissue disease: a systematic review and meta-analysis. Eur Respir Rev. 2023;32(167):220210. doi:10.1183/16000617.0210-2022
18. Zhang L, Wu G, Gao D, et al. Factors associated with interstitial lung disease in patients with polymyositis and dermatomyositis: a systematic review and meta-analysis. PLoS One. 2016;11(5):e0155381. doi:10.1371/journal.pone.0155381
19. Matteson EL, Matucci-Cerinic M, Kreuter M, et al. Patient-level factors predictive of interstitial lung disease in rheumatoid arthritis: a systematic review. RMD Open. 2023;9(3):e003059. doi:10.1136/rmdopen-2023-003059
20. Doyle TJ, Juge PA, Peljto AL, et al. Short peripheral blood leukocyte telomere length in rheumatoid arthritis-interstitial lung disease. Thorax. 2024;79(2):182-185. doi:10.1136/thorax-2023-220022
21. Volkmann ER, Kreuter M, Hoffmann-Vold AM, et al. Dyspnoea and cough in patients with systemic sclerosis-associated interstitial lung disease in the SENSCIS trial. Rheumatology (Oxford). 2022;61(11):4397-4408. doi:10.1093/rheumatology/keac091
22. Suliman YA, Dobrota R, Huscher D, et al. Brief report: pulmonary function tests: high rate of false-negative results in the early detection and screening of scleroderma-related interstitial lung disease. Arthritis Rheumatol. 2015;67(12):3256-3261. doi:10.1002/art.39405
23. Bernstein EJ, Jaafar S, Assassi S, et al. Performance characteristics of pulmonary function tests for the detection of interstitial lung disease in adults with early diffuse cutaneous systemic sclerosis. Arthritis Rheumatol. 2020;72(11):1892-1896. doi:10.1002/art.41415
24. Hoffmann T, Oelzner P, Franz M, et al. Assessing the diagnostic value of a potential screening tool for detecting early interstitial lung disease at the onset of inflammatory rheumatic diseases. Arthritis Res Ther. 2022;24(1):107. doi:10.1186/s13075-022-02786-x
25. Mohning MP, Amigues I, Demoruelle MK, et al. Duration of rheumatoid arthritis and the risk of developing interstitial lung disease. ERJ Open Res. 2021;7(1):00633-2020. doi:10.1183/23120541.00633-2020
26. Assassi S, Shao N, Yin Z, Volkmann ER, Zoz DF, Leonard TB. Understanding diagnostic pathways in systemic sclerosis and systemic sclerosis-associated interstitial lung disease: a retrospective cohort study. Medicine (Baltimore). 2022;101(32):e29993. doi:10.1097/MD.0000000000029993
27. Johnson SR, Bernstein EJ, Bolster MB, et al. 2023 American College of Rheumatology (ACR)/American College of Chest Physicians (CHEST) guideline for the screening and monitoring of interstitial lung disease in people with systemic autoimmune rheumatic diseases. Arthritis Rheumatol. 2024;76(8):1201-1213. doi:10.1002/art.42860
28. Johnson S. Presentation of the systemic autoimmune rheumatic disease-interstitial lung disease screening, monitoring, and treatment guidelines. Oral presentation at: American College of Rheumatology (ACR) Convergence 2023, November 12, 2023; San Diego, CA.
29. Narváez J, Aburto M, Seoane-Mato D, et al. Screening criteria for interstitial lung disease associated to rheumatoid arthritis: expert proposal based on Delphi methodology. Reumatol Clin (Engl Ed). 2023;19(2):74-81. doi:10.1016/j.reumae.2021.12.003
30. Hackner K, Hütter L, Flick H, et al. Screening for rheumatoid arthritis-associated interstitial lung disease—a Delphi-based consensus statement. Z Rheumatol. 2024;83:160-168. doi:10.1007/s00393-023-01464-w
31. Hoffmann-Vold AM, Maher TM, Philpot EE, et al. The identification and management of interstitial lung disease in systemic sclerosis: evidence-based European consensus statements. Lancet Rheumatol. 2020;2:e71-e83. doi:10.1016/S2665-9913(19)30144-4
32. Rahaghi FF, Hsu VM, Kaner RJ, et al. Expert consensus on the management of systemic sclerosis-associated interstitial lung disease. Respir Res. 2023;24(1):6. doi:10.1186/s12931-022-02292-3
33. Sgalla G, Walsh SLF, Sverzellati N, et al. “Velcro-type” crackles predict specific radiologic features of fibrotic interstitial lung disease. BMC Pulm Med. 2018;18(1):103. doi:10.1186/s12890-018-0670-0
34. Fairchild R, Chung M, Yang D, Sharpless L, Li S, Chung L. Development and assessment of novel lung ultrasound interpretation criteria for the detection of interstitial lung disease in systemic sclerosis. Arthritis Care Res (Hoboken). 2021;73(9):1338-1342. doi:10.1002/acr.24338
35. Reyes-Long S, Gutierrez M, Clavijo-Cornejo D, et al. Subclinical interstitial lung disease in patients with systemic sclerosis. A pilot study on the role of ultrasound. Reumatol Clin (Engl Ed). 2021;17(3):144-149. doi:10.1016/j.reuma.2019.05.004
36. Gargani L, Romei C, Bruni C, et al. Lung ultrasound B-lines in systemic sclerosis: cut-off values and methodological indications for interstitial lung disease screening. Rheumatology (Oxford). 2022;61(SI):SI56-SI64. doi:10.1093/rheumatology/keab801
37. Beigi MRD, Pellegrino G, Loconte M, et al. Lung ultrasound compared to computed tomography detection and automated quantification of systemic sclerosis-associated interstitial lung disease: preliminary study. Rheumatology (Oxford). 2023:kead324. doi:10.1093/rheumatology/kead324
38. Mena-Vázquez N, Jimenez-Núñez FG, Godoy-Navarrete FJ, et al. Utility of pulmonary ultrasound to identify interstitial lung disease in patients with rheumatoid arthritis. Clin Rheumatol. 2021;40(6):2377-2385. doi:10.1007/s10067-021-05655-1
39. Gutierrez M, Ruta S, Clavijo-Cornejo D, Fuentes-Moreno G, Reyes-Long S, Bertolazzi C. The emerging role of ultrasound in detecting interstitial lung disease in patients with rheumatoid arthritis. Joint Bone Spine. 2022;89(6):105407. doi:10.1016/j.jbspin.2022.105407
40. Buda N, Wojteczek A, Masiak A, Piskunowicz M, Batko W, Zdrojewski Z. Lung ultrasound in the screening of pulmonary interstitial involvement secondary to systemic connective tissue disease: a prospective pilot study involving 180 patients. J Clin Med. 2021;10(18):4114. doi:10.3390/jcm10184114
41. Kim YJ, Choe J, Kim HJ, Song JW. Long-term clinical course and outcome in patients with primary Sjögren syndrome-associated interstitial lung disease. Sci Rep. 2021;11(1):12827. doi:10.1038/s41598-021-92024-2
42. Chang SH, Lee JS, Ha YJ, et al. Lung function trajectory of rheumatoid arthritis-associated interstitial lung disease. Rheumatology (Oxford). 2023;62(9):3014-3024. doi:10.1093/rheumatology/kead027
43. Dsouza KG, Alexander AS, Watts JR Jr, Kulkarni T. Management of interstitial lung disease in patients with autoimmune disease-related interstitial lung disease. Multidiscip Respir Med. 2023;18(1):890. doi:10.4081/mrm.2023.890
44. Khanna D, Mittoo S, Aggarwal R, et al. Connective tissue disease-associated interstitial lung diseases (CTD-ILD) - report from OMERACT CTD-ILD Working Group. J Rheumatol. 2015;42(11):2168-2171. doi:10.3899/jrheum.141182
45. Volkmann ER, Tashkin DP, Roth MD, Goldin J, Kim GHJ. Early radiographic progression of scleroderma: lung disease predicts long-term mortality. Chest. 2022;161(5):1310-1319. doi:10.1016/j.chest.2021.11.033
46. Raghu G, Remy-Jardin M, Richeldi L, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2022;205(9):e18-e47. doi:10.1164/rccm.202202-0399ST
47. Rahaghi FF, Kolaitis NA, Adegunsoye A, et al. Screening strategies for pulmonary hypertension in patients with interstitial lung disease: a multidisciplinary Delphi study. Chest. 2022;162(1):145-155. doi:10.1016/j.chest.2022.02.012
48. Forestier A, Le Gouellec N, Béhal H, et al. Evolution of high-resolution CT-scan in systemic sclerosis-associated interstitial lung disease: description and prognosis factors. Semin Arthritis Rheum. 2020;50(6):1406-1413. doi:10.1016/j.semarthrit.2020.02.015
49. Carnevale A, Silva M, Maietti E, et al. Longitudinal change during follow-up of systemic sclerosis: correlation between high-resolution computed tomography and pulmonary function tests. Clin Rheumatol. 2021;40(1):213-219. doi:10.1007/s10067-020-05375-y
50. Cottin V, Martinez FJ, Smith V, Walsh SLF. Multidisciplinary teams in the clinical care of fibrotic interstitial lung disease: current perspectives. Eur Respir Rev. 2022;31(165):220003. doi:10.1183/16000617.0003-2022
51. Walsh SLF, Lafyatis RA, Cottin V. Imaging features of autoimmune disease-related interstitial lung diseases. J Thorac Imaging. 2023;38(suppl 1):S30-S37. doi:10.1097/RTI.0000000000000734
52. Flaherty KR, Wells AU, Cottin V, et al; INBUILD Trial Investigators. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med. 2019;381(18):1718-1727. doi:10.1056/NEJMoa1908681
53. Maher TM, Corte TJ, Fischer A, et al. Pirfenidone in patients with unclassifiable progressive fibrosing interstitial lung disease: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med. 2020;8(2):147-157. doi:10.1016/S2213-2600(19)30341-8
54. Behr J, Prasse A, Kreuter M, et al; RELIEF investigators. Pirfenidone in patients with progressive fibrotic interstitial lung diseases other than idiopathic pulmonary fibrosis (RELIEF): a double-blind, randomised, placebo-controlled, phase 2b trial. Lancet Respir Med. 2021;9(5):476-486. doi:10.1016/S2213-2600(20)30554-3
55. Kwon BS, Choe J, Chae EJ, Hwang HS, Kim YG, Song JW. Progressive fibrosing interstitial lung disease: prevalence and clinical outcome. Respir Res. 2021;22(1):282. doi:10.1186/s12931-021-01879-6
56. Khor YH, Farooqi M, Hambly N, Kolb M, Ryerson CJ; Austin ILD Registry and CARE-PF Investigators. Patient characteristics and survival for progressive pulmonary fibrosis using different definitions. Am J Respir Crit Care Med. 2023;207(1):102-105. doi:10.1164/rccm.202205-0910LE
57. Lee JK, Ahn Y, Noh HN, et al. Clinical effect of progressive pulmonary fibrosis on patients with connective tissue disease-associated interstitial lung disease: a single center retrospective cohort study. Clin Exp Med. 2023;23(8):4797-4807. doi:10.1007/s10238-023-01212-z
58. Distler JHW, Györfi AH, Ramanujam M, Whitfield ML, Königshoff M, Lafyatis R. Shared and distinct mechanisms of fibrosis. Nat Rev Rheumatol. 2019;15(12):705-730. doi:10.1038/s41584-019-0322-7
59. Castelino FV, Moua T. Detection and management of interstitial lung diseases associated with connective tissue diseases. ACR Open Rheumatol. 2021;3(5):295-304. doi:10.1002/acr2.11253
60. Teoh AKY, Holland AE, Morisset J, et al; ILD MDM Delphi Collaborators. Essential features of an interstitial lung disease multidisciplinary meeting: an international Delphi survey. Ann Am Thorac Soc. 2022;19(1):66-73. doi:10.1513/AnnalsATS.202011-1421OC
61. McLean AEB, Webster SE, Fry M, et al. Priorities and expectations of patients attending a multidisciplinary interstitial lung disease clinic. Respirology. 2021;26(1):80-86. doi:10.1111/resp.13913
62. Johnson SR, Bernstein EJ, Bolster MB, et al. 2023 American College of Rheumatology (ACR)/American College of Chest Physicians (CHEST) guideline for the treatment of interstitial lung disease in people with systemic autoimmune rheumatic diseases. Arthritis Rheumatol. 2024;76(8):1182-1200. doi:10.1002/art.42861
63. Tashkin DP, Roth MD, Clements PJ, et al; Scleroderma Lung Study II Investigators. Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease (SLS II): a randomised controlled, double-blind, parallel group trial. Lancet Respir Med. 2016;4(9):708-719. doi:10.1016/S2213-2600(16)30152-7
64. Distler O, Highland KB, Gahlemann M, et al; SENSCIS Trial Investigators. Nintedanib for systemic sclerosis-associated interstitial lung disease. N Engl J Med. 2019;380(26):2518-2528. doi:10.1056/NEJMoa1903076
65. Highland KB, Distler O, Kuwana M, et al; SENSCIS trial investigators. Efficacy and safety of nintedanib in patients with systemic sclerosis-associated interstitial lung disease treated with mycophenolate: a subgroup analysis of the SENSCIS trial. Lancet Respir Med. 2021;9(1):96-106. doi:10.1016/S2213-2600(20)30330-1
66. Roofeh D, Lin CJF, Goldin J, et al; focuSSced Investigators. Tocilizumab prevents progression of early systemic sclerosis-associated interstitial lung disease. Arthritis Rheumatol. 2021;73(7):1301-1310. doi:10.1002/art.41668
67. Maher TM, Tudor VA, Saunders P, et al; RECITAL Investigators. Rituximab versus intravenous cyclophosphamide in patients with connective tissue disease-associated interstitial lung disease in the UK (RECITAL): a double-blind, double-dummy, randomised, controlled, phase 2b trial. Lancet Respir Med. 2023;11(1):45-54. doi:10.1016/S2213-2600(22)00359-9
68. Mankikian J, Caille A, Reynaud-Gaubert M, et al; EVER-ILD investigators and the OrphaLung network. Rituximab and mycophenolate mofetil combination in patients with interstitial lung disease (EVER-ILD): a double-blind, randomised, placebo-controlled trial. Eur Respir J. 2023;61(6):2202071. doi:10.1183/13993003.02071-2022
69. Raghu G, Montesi SB, Silver RM, et al. Treatment of systemic sclerosis-associated interstitial lung disease: evidence-based recommendations. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2024;209(2):137-152. doi:10.1164/rccm.202306-1113ST
70. van Laar JM, Farge D, Sont JK, et al; EBMT/EULAR Scleroderma Study Group. Autologous hematopoietic stem cell transplantation vs intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis: a randomized clinical trial. JAMA. 2014;311(24):2490-2498. doi:10.1001/jama.2014.6368
71. Sullivan KM, Goldmuntz EA, Keyes-Elstein L, et al; SCOT Study Investigators. Myeloablative autologous stem-cell transplantation for severe scleroderma. N Engl J Med. 2018;378(1):35-47. doi:10.1056/nejmoa1703327
72. Kanate AS, Majhail NS, Savani BN, et al. Indications for hematopoietic cell transplantation and immune effector cell therapy: guidelines from the American Society for Transplantation and Cellular Therapy. Biol Blood Marrow Transplant. 2020;26(7):1247-1256. doi:10.1016/j.bbmt.2020.03.002
73. Kolb M, Flaherty KR, Silva RS, et al; INBUILD trial investigators. Effect of nintedanib in patients with progressive pulmonary fibrosis in subgroups with differing baseline characteristics. Adv Ther. 2023;40(12):5536-5546. doi:10.1007/s12325-023-02668-x
74. Wells AU, Flaherty KR, Brown KK, et al; INBUILD trial investigators. Nintedanib in patients with progressive fibrosing interstitial lung diseases-subgroup analyses by interstitial lung disease diagnosis in the INBUILD trial: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Respir Med. 2020;8(5):453-460. doi:10.1016/S2213-2600(20)30036-9
75. Matteson EL, Kelly C, Distler JHW, et al; INBUILD Trial Investigators. Nintedanib in patients with autoimmune disease-related progressive fibrosing interstitial lung diseases: subgroup analysis of the INBUILD trial. Arthritis Rheumatol. 2022;74(6):1039-1047. doi:10.1002/art.42075
76. Matteson EL, Aringer M, Burmester GR, Mueller H, Moros L, Kolb M. Effect of nintedanib in patients with progressive pulmonary fibrosis associated with rheumatoid arthritis: data from the INBUILD trial. Clin Rheumatol. 2023;42(9):2311-2319. doi:10.1007/s10067-023-06623-7
77. Wijsenbeek M, Swigris JJ, Inoue Y, et al; INBUILD Trial Investigators. Effects of nintedanib on symptoms in patients with progressive pulmonary fibrosis. Eur Respir J. 2023:2300752. doi:10.1183/13993003.00752-2023
78. Juge PA, Hayashi K, McDermott GC, et al. Effectiveness and tolerability of antifibrotics in rheumatoid arthritis-associated interstitial lung disease. Semin Arthritis Rheum. 2024;64:152312. doi:10.1016/j.semarthrit.2023.152312
79. Rochester CL, Alison JA, Carlin B, et al. Pulmonary rehabilitation for adults with chronic respiratory disease: an official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2023;208(4):e7-e26. doi:10.1164/rccm.202306-1066ST
80. Hoffmann-Vold AM, Allanore Y, Bendstrup E, et al. The need for a holistic approach for SSc-ILD - achievements and ambiguity in a devastating disease. Respir Res. 2020;21(1):197. doi:10.1186/s12931-020-01459-0
81. Vick B, Vick P, Hoy H. Living with lung fibrosis: knowledge is power. Future Rare Dis. 2023;3(4). doi:10.2217/frd-2023-0003
82. Jacobs SS, Krishnan JA, Lederer DJ, et al. Home oxygen therapy for adults with chronic lung disease. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2020;202(10):e121-e141. doi:10.1164/rccm.202009-3608ST
83. Tikellis G, Hoffman M, Mellerick C, Burge AT, Holland AE. Barriers to and facilitators of the use of oxygen therapy in people living with an interstitial lung disease: a systematic review of qualitative evidence. Eur Respir Rev. 2023;32(169):230066. doi:10.1183/16000617.0066-2023
84. Crespo MM, Lease ED, Sole A, et al. ISHLT consensus document on lung transplantation in patients with connective tissue disease: part I: epidemiology, assessment of extrapulmonary conditions, candidate evaluation, selection criteria, and pathology statements. J Heart Lung Transplant. 2021;40(11):1251-1266. doi:10.1016/j.healun.2021.07.014
85. Prieto-Peña D, Martínez-Meñaca A, Calderón-Goercke M, et al. Long-term survival of lung transplantation for interstitial lung disease associated with connective tissue diseases: a study of 26 cases from a referral centre. Clin Exp Rheumatol. 2020;38(4):615-620.
86. Yang X, Wei D, Liu M, et al. Survival and outcomes after lung transplantation for connective tissue disease-associated interstitial lung diseases. Clin Rheumatol. 2021;40(9):3789-3795. doi:10.1007/s10067-021-05704-9
87. Cassidy N, Fox L, Love M, et al. Fibrotic interstitial lung disease – palliative care needs: a World-Café qualitative study. BMJ Support Palliat Care. 2021;bmjspcare-2021-003249. doi:10.1136/bmjspcare-2021-003249