- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
COVID-19 Infection Associated With Risk of Autoimmune, Autoinflammatory Disorders
A retrospective, population-based study reveals a possible association between COVID-19 infection and autoimmune and autoinflammatory outcomes.
In a study recently published in JAMA Network Open, COVID-19 infection was linked to increased risks for developing autoimmune and autoinflammatory connective tissue disorders among people living in Korea.
Since the onset of the COVID-19 pandemic, SARS-CoV-2 infection has become increasingly associated with cardiovascular and respiratory issues. Among this growing body of literature, some studies have theorized that COVID-19 could also contribute to autoimmune or inflammatory disorders because of its proclivity to trigger degrees of autoimmune responses.
To date, however, no extensive investigation has been conducted to determine the validity of this relationship. To address this gap, researchers conducted a large, population-based analysis examining associations between post-acute COVID-19 sequelae and autoimmune disease.
Data were gathered from the Korea Disease Control and Prevention Agency COVID-19 National Health Insurance to identify individuals with a COVID-19 diagnosis between October 2020 through December of 2021. Additionally, researchers identified a control group of those who had no prior evidence of COVID-19 infection.
The COVID-19 group consisted of 354,527 people, and the control was included 6,134,940 people. Both cohorts had a fairly equal ratio of women to men and a median age of approximately 52 years. Average follow-up lengths for the COVID-19 group and controls were 119 and 121 days, respectively.
Researchers found that individuals with COVID-19 carried a significantly higher risk for multiple autoimmune conditions, such as: alopecia areata and totalis (adjusted hazard ratios [aHRs] of 1.12 and 1.74, respectively), Crohn disease (aHR, 1.68), antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (aHR, 2.76), and sarcoidosis (aHR, 1.59).
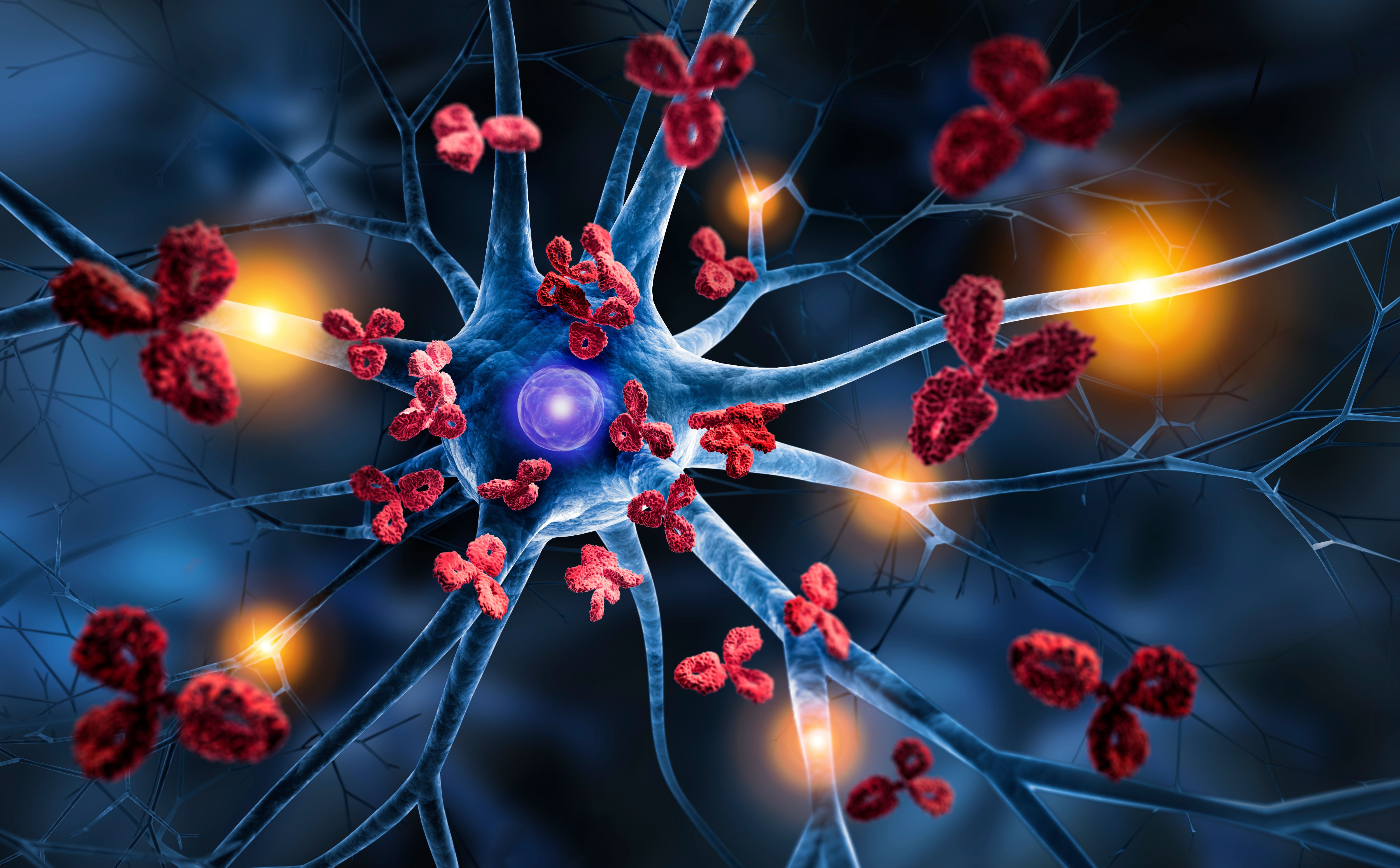
Autoimmune Disorder, Nerve Cell | peterschreiber.media - stock.adobe.com
A subgroup analysis also revealed age- and sex-specific risks in the COVID-19 group. Those under 40 were more susceptible to developing Crohn disease, sarcoidosis, adult-onset Still disease, and rheumatoid arthritis. Individuals over 40 experienced higher incidence of alopecia areata and totalis, as well as ANCA-associated vasculitis. Men were more vulnerable to alopecia totalis, Crohn disease, psoriasis, systemic sclerosis, adult-onset Still disease, and ankylosing spondylitis. Women demonstrated higher vulnerability for alopecia areata and totalis, ANCA-associated vasculitis, sarcoidosis, Crohn disease, and vitiligo.
The authors noted that the increased prevalence of these diseases correlated with more severe COVID-19 infection. Additionally, they noticed that the population vaccinated against COVID-19 exhibited lower risks for autoimmune outcomes while those who were unvaccinated carried increased risks for Crohn disease, and alopecia areata and totalis.
In the wake of their results, the authors touch and theorize on how COVID-19 influences autoimmunity. Cytokine production associated with SARS-CoV-2-related immune damage has been a topic of concern here that could explain inflammation spikes in affected patients.
Furthermore, they noted that “Patients with COVID-19 mount an early and robust defense through the activation of type 1 and 2 interferon (IFN) responses, which are pivotal against viral infections. Nevertheless, studies indicate that these IFN responses may also induce hyperinflammation, exacerbate the severity of COVID-19, and be associated with mortality.”
As their findings “suggest the existence of a common pathway” between COVID-19 and the underlying mechanisms of these diseases, the researchers advocate for long-term COVID-19 management that evaluates and considers these risks for autoimmune and autoinflammatory outcomes.
Reference
Lim SH, Ju HJ, Han JH, et al. Autoimmune and autoinflammatory connective tissue disorders following COVID-19. JAMA Netw Open. 2023 Oct 2:6(10). doi: 10.1001/jamanetworkopen.2023.36120
