- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Telehealth Shows Staying Power During COVID-19 Pandemic
Robin Gelburd, JD, president of FAIR Health, discusses consistent telehealth use throughout the coronavirus disease 2019 (COVID-19) pandemic.
The staying power of telehealth during the COVID-19 pandemic was evident in the August 2020 results of FAIR Health’s % Monthly Telehealth claim lines increased 3552% nationally from August 2019 to August 2020, rising from 0.17% of medical claim lines in August 2019 to 6.07% in August 2020 (Figure 1). From month to month, the telehealth share of medical claim lines stayed relatively the same nationally, rising 1.2 percent from 6.00% in July 2020 to 6.07% in August 2020. The data represent the privately insured population, excluding Medicare and Medicaid.
Figure 1. Monthly Telehealth Regional Tracker, August 2020, United States
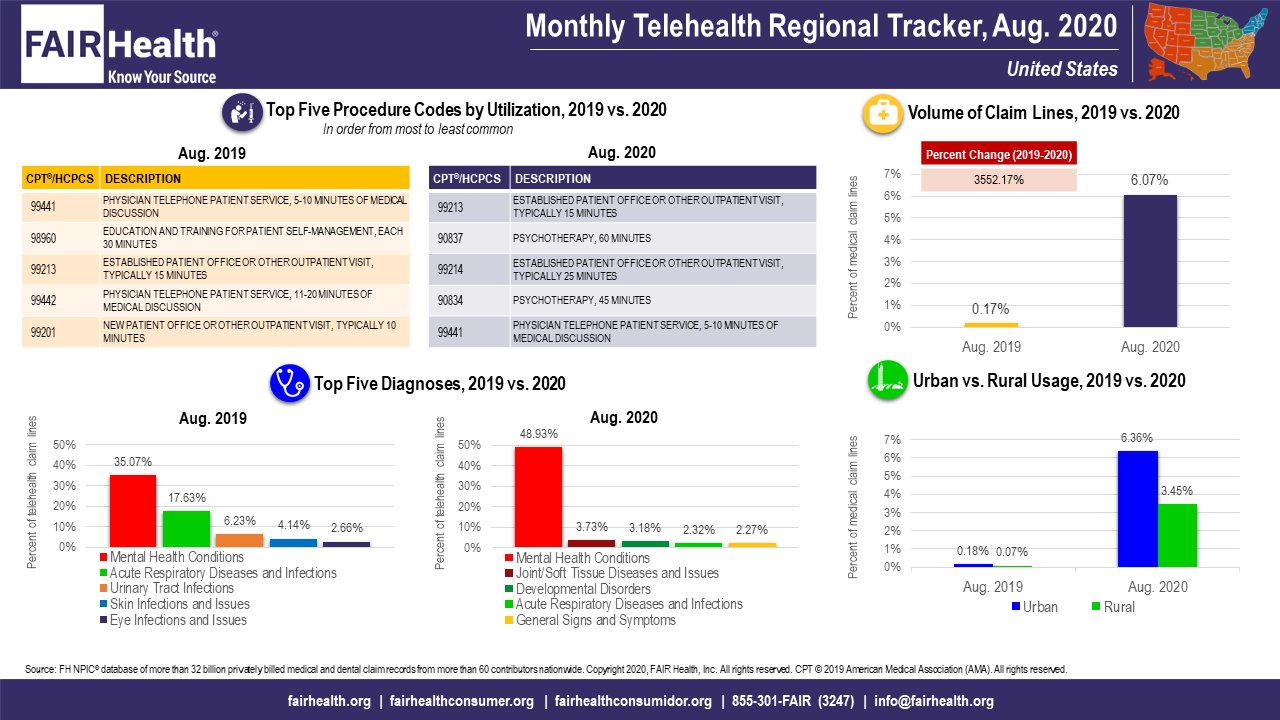
(Source: FAIR Health)
Trends in the 4 US census regions (Midwest, Northeast, South and West) were similar to those in the nation as a whole. In each region, there were large percent increases in volume of claim lines from August 2019 to August 2020, but small variations in volume of claim lines from July 2020 to August 2020. The variations were, to some degree, commensurate with changes in the pandemic—for example, rising the most (9.7%) in the South, which was particularly hard-hit in the summer; falling the most (7.7%) in the Northeast, which had experienced its peak of cases in the spring (Figure 2).
Figure 2. Monthly Telehealth Regional Tracker, August 2020, South
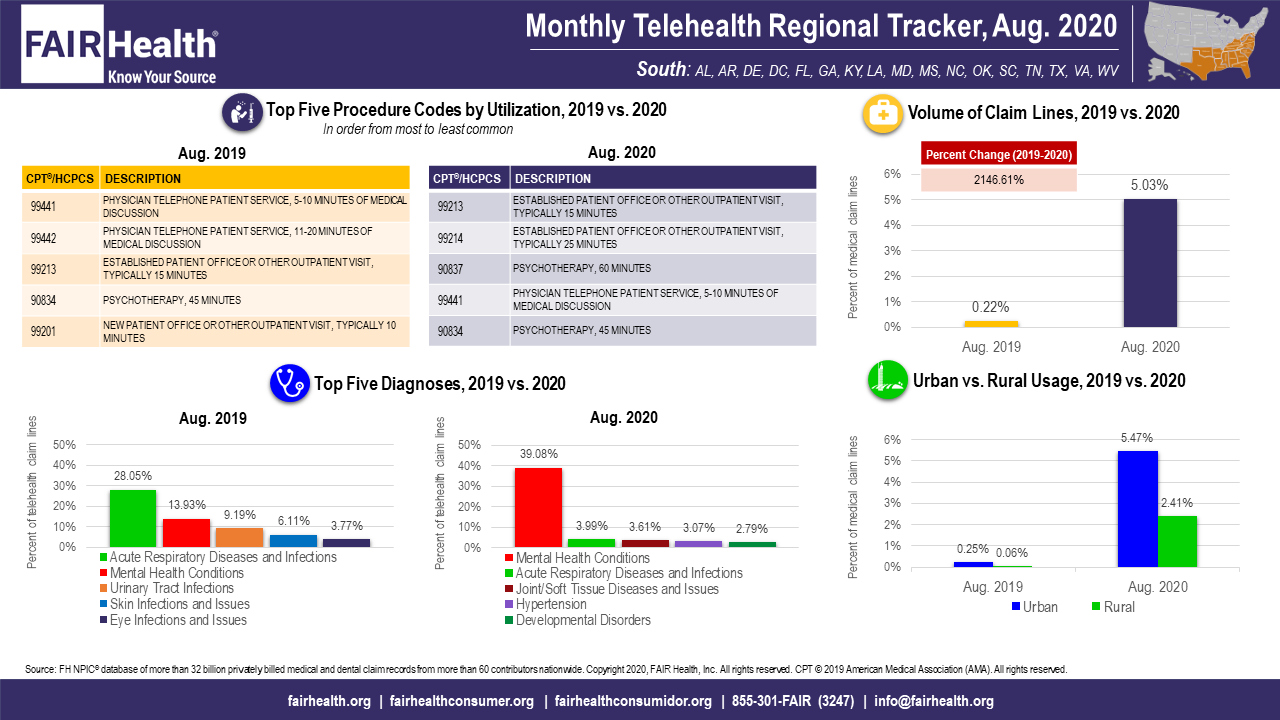
(Source: FAIR Health)
Higher telehealth utilization from March to August 2020 in comparison with the same months in 2019 is likely a result of the COVID-19 pandemic. In March and April 2020, many states prohibited in-person rendering of elective procedures, making telehealth an attractive alternative. Many of these prohibitions expired in May as states began to open up. But despite some decline from month to month, telehealth usage remained high by comparison with 2019.
Other notable findings of the August Monthly Telehealth Regional Tracker concern the top 5 telehealth diagnoses:
- Mental health conditions, the number one telehealth diagnosis nationally and in every region since March 2020, continued to rise as a share of all telehealth diagnoses, growing nationally from 45.39% to 48.93% from July to August 2020. An increase of similar size occurred across regions—four percent in every region but the Midwest, which saw three percent growth.
- From July to August 2020, acute respiratory diseases rose from the fifth most common diagnosis in telehealth nationally (at 2.37%) to the fourth most common (at 2.32%). Even so, acute respiratory diseases accounted for a much smaller share of telehealth in August 2020 than they did in August 2019 (17.63%), due to the diversity of other diagnoses that became more common in telehealth as a result of the pandemic.
Launched in May as a free service, the Monthly Telehealth Regional Tracker uses FAIR Health data to track how telehealth is evolving. An interactive map of the four US census regions allows the user to view an infographic on telehealth in a specific month in each region, or in the nation as a whole. In addition to data on the volume of claim lines and on diagnoses, each infographic includes findings on urban versus rural usage and the top five telehealth procedure codes.
FAIR Health is a national, independent nonprofit organization dedicated to bringing transparency to healthcare costs and health insurance information.
After several months of the COVID-19 pandemic, telehealth has persisted in showing high utilization across the country. FAIR Health’s Monthly Telehealth Regional Tracker will continue to provide a window into how this venue of care is evolving.
About the Author
Robin Gelburd, JD, is the President of FAIR Health, a national, independent nonprofit organization with the mission of bringing transparency to healthcare costs and health insurance information. FAIR Health possesses the nation’s largest collection of private healthcare claims data, which includes over 32 billion claim records and is growing at a rate of over 2 billion claim records a year. Certified by CMS as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D; FAIR Health includes among the private claims data in its database, data on Medicare Advantage enrollees. Gelburd is a nationally recognized expert on healthcare policy, data and transparency.
