- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: SDOH-Sensitive Adherence Strategies for MA Health Equity Index Success
The need for health equity spans the entire health care ecosystem, including the Medicare Advantage (MA) population. Neutralizing social determinants of health (SDOH) barriers, well-informed adherence strategies help MA plans navigate new CMS measurement frameworks, like the Health Equity Index.
The Medicare Advantage (MA) population spans the entire socioeconomic continuum, from financially secure individuals living in areas rich with health care choices, to those experiencing the negative side of the social determinants of health (SDOH).
MA plans are challenged to meet the needs of people at multiple points on the spectrum at the same time, including those facing health disparities—which can, in turn, result in worsened health outcomes for socially vulnerable members and poor experiences with the plan if left unaddressed.
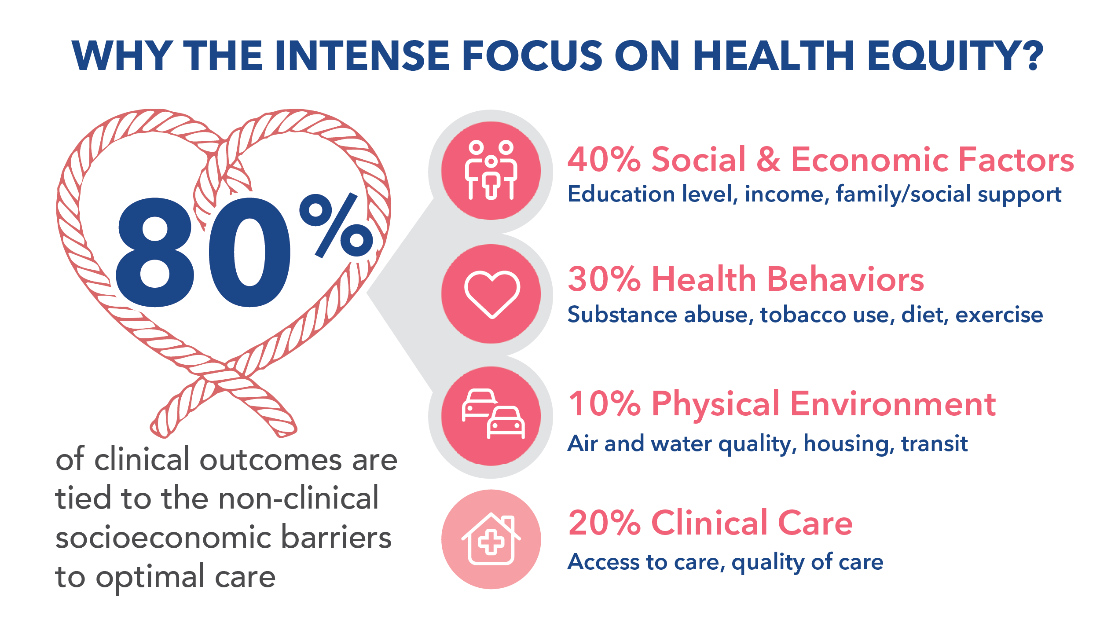
As the industry rallies around the recognition that up to 80% of clinical outcomes are tied to the non-clinical socioeconomic barriers to optimal care, CMS is taking a leading role in changing the equity equation.
Why the Intense Focus on Health Equity? | Image credit: AdhereHealth
By introducing the new Health Equity Index (HEI) for MA plans in 2024, CMS is leveraging the power of the Star Ratings system and its significant financial incentives to guide MA plans toward the delivery of more accessible, affordable, and culturally sensitive care.
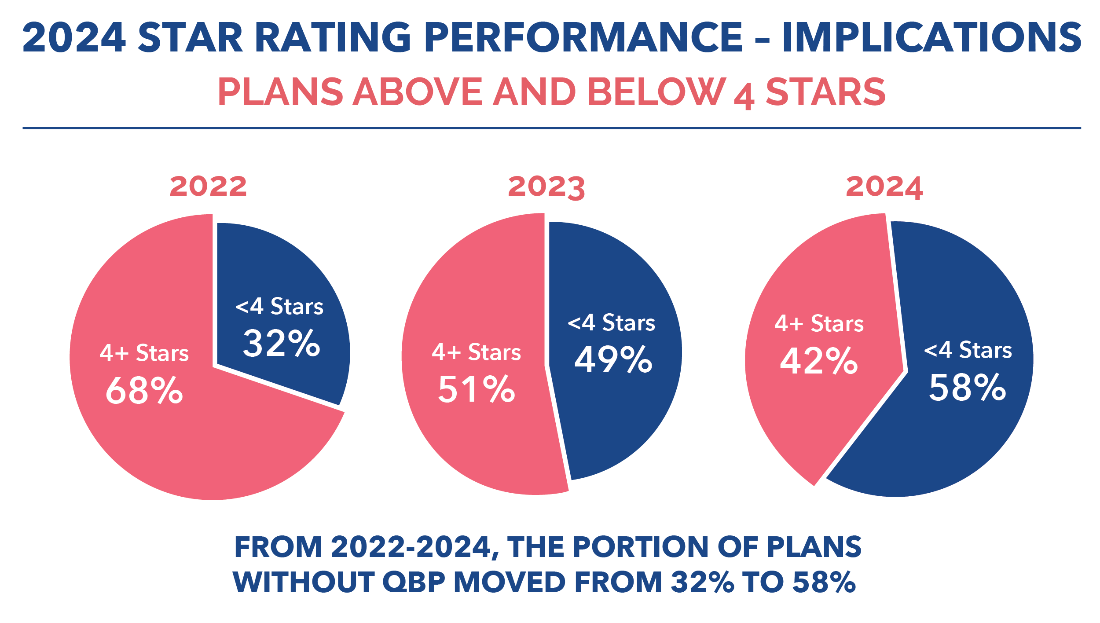
Eligible plans that perform well on the HEI can secure improved Star Ratings and the additional financial incentives of the Quality Bonus Payment (QBP) pool. Those that fall short will miss out on the opportunity to reinvest into plan benefits and drive increased member enrollment in upcoming years.
To benefit from the HEI—and recover from the overall Star Ratings stumble in 2024—MA plans will need to implement a “whole person,” SDOH-first approach to identifying high-risk members, connecting with these individuals, and resolving their socioeconomic barriers.
2024 Star Rating Performance - Implications | Image credit: AdhereHealth
By deeply integrating SDOH-focused programs and technologies into the care process, plans can improve adherence and health outcomes to unlock incentive opportunities via improved health equity, member experience, and Stars performance.
What is the Health Equity Index (HEI)?
The HEI is designed to provide a structured way to gauge and incentivize MA plans’ efforts to reduce health disparities for Part C and D members facing specific social risk factors (SRFs), initially focused on those who receive a low-income subsidy, are dual eligible for Medicaid, and are disabled (defined in this case by CMS as Medicare members aged 65 years and younger who enrolled in Medicare due to a disability).
Using data from measurement years 2024–2025, the HEI will be calculated from a subset of existing Stars measures that will be announced annually, including the triple-weighted adherence measures (RAS, Statin, and Diabetes).
CMS will determine eligibility for the HEI incentive reward by comparing plans with their peers and ranking them into 3 tiers, each of which will receive a score: a positive point for the top third of scores, 0 points for the middle third, or a negative point for the bottom third. Plans must have a total HEI score greater than 0 to qualify for any reward.
The new reward factor is 0.4, which will be multiplied by the plan’s HEI score and added to the plan’s overall Star Rating, which can have a substantial effect on overall scores. For example, a plan that earns a score of 1, multiplied by 0.4, could earn almost half a Star to boost their overall rating and increase the potential to earn QBP incentives.
Because not all contracts will qualify to participate in the HEI, plans will need to carefully assess their member populations to determine eligibility and perform detailed analytics to predict their likelihood of adequate performance for relevant contracts.
Implementing an SDOH-first approach to equitable care delivery
To prepare for success with the HEI, as well as improve their overall Star Rating, MA plans will need to invest in data-driven analytics solutions to understand their members, develop an accurate risk profile, and jumpstart engagement initiatives to support members throughout their health care journey.
Applying analytics strategies to identify members for outreach
The first step for determining contract eligibility is understanding the member population and their socioeconomic risk factors. Plans should consider using a patient relationship management solution that can generate reports identifying members by risk level—and, for the benefit of the HEI, clearly identify individuals by relevant SRF.
Once plans have a clear view of their targeted member list, the platform should be able to use near–real time, multisource data to prioritize members for outreach and engagement based on their unique risk factors and needs. This data should include prescription claims (enriched by other utilization data sources, when possible), as well as available federal, state, and local data (such as the CDC’s Social Vulnerability Index) to give outreach staff deeper, more personalized insight into likely issues to address during interactions using a variety of modalities throughout the care continuum.
For plans that don’t currently have access to this comprehensive, integrated data, partnering with a health care technology and data analytics expert could be the key to jumpstarting success in 2024 to meet CMS’s ambitious timeframe for the HEI.
Resolving socioeconomic challenges in an actionable, personalized manner
SDOH factors, such as lack of transportation, housing and food instability, low health literacy, or social isolation, have a profound impact on a member’s ability to achieve and maintain adherence to their medications and care plans. Simply identifying that these factors exist isn’t enough. Plans must take action to resolve them in both the short term and the long term.
While regional social vulnerability data is a helpful starting point, plans will need to learn from members themselves about the full scope of their challenges. Using motivational interviewing techniques that focus on open, empathetic and judgment-free discussion will be crucial to build relationships with members and generate trust.
Through respectful dialogue and tailored guidance, clinicians can help members understand the importance of adherence with medication and treatment protocols, connect them with community resources in real time, and follow up on a regular schedule to ensure continued adherence and longitudinal maintenance for long-term positive health outcomes.
To scale up SDOH initiatives that meet the requirements of the HEI, plans will need to invest in technologies that streamline workflows for outreach clinicians and include intuitive access to community referrals and health benefit information so staff can resolve issues during the engagement, instead of forcing members into playing phone tag with multiple entities.
Monitor adherence to anticipate HEI and Stars performance
Establishing adherence at the start of the year does not guarantee that a member will remain adherent 3, 6, or 9 months later. Plans will need to follow up on a regular basis with members to ensure they remain engaged throughout the performance period to meet certain heavily weighted, time-sensitive measures, such as those tied to medication adherence.
Frequent ingestion of data provides plans with performance metrics (the nearer to real-time, the better) to track successful member adherence and performance on the Stars measures related to the HEI.
Access to dashboard visualizations and reports of this critical information enable plans to continually project HEI scoring and prepare for end-of-the-year Star Ratings performance. When performance wavers, portal access to key metrics allows the plan to reengage patients with appropriate clinical and non-clinical services and maintain continuous program effectiveness.
As high performance on the Star Ratings system becomes even more crucial to overall success in the market, MA plans will need to quickly and comprehensively invest in a year-round, data-driven, SDOH-first approach to addressing health equity. Using these strategies, MA plans can better understand how to meet the requirements of the HEI and outperform their peers to access financial incentive opportunities.
