- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Providers and Patients Push Back, Payers Push Forward—Co-pay Mitigation Programs
Research shows how commercial health plans impact payer trends in the co-pay landscape and provides key areas that pharmaceutical and biotech manufacturers can explore to ensure patient access.
The Cost of Rising Health Care Costs and Role of Mitigation Programs
As the list prices of drugs are rising, in many instances patients’ out-of-pocket (OOP) spending is also increasing, leading to concerns with maintaining patient access to medically necessary treatments. Manufacturers have introduced co-pay assistance programs to help offset the financial burden associated with treatment costs. However, payers have subsequently implemented co-pay accumulator and maximizer programs, hereinafter referred to as “co-pay mitigation programs,” in reaction to the manufacturer activity to lower patient cost exposure for expensive drugs. Co-pay mitigation programs prevent co-pay assistance funds from being counted toward patient OOP costs or yearly deductibles. Notable examples include UnitedHealthcare’s (UHC) Coupon Adjustment, CVS Caremark’s Specialty Copay Card Program, and Express Scripts’ Out of Pocket Protection Program.1-3 Furthermore, CVS and Express Scripts have partnered with independent companies to operate specialty drug maximizer programs for their beneficiaries.4 These programs consequently increase patient OOP expenses and negatively affect therapy initiation and adherence.
Stakeholders Push Back
In October 2020, the American College of Rheumatology (ACR) petitioned UHC to cancel a proposed co-pay accumulator initiative that would require providers to submit information on their patients’ utilization of manufacturer co-pay assistance programs.5 Following pushback from healthcare professionals, UHC announced they would delay implementation of the program.6 Additionally, in November 2020, the American Medical Association (AMA) passed a resolution sponsored by ACR calling for federal and state laws that would ban co-pay accumulator policies, including in federally regulated health plans. In both efforts, ACR was joined by specialities in dermatology, neurology, gastroenterology, and oncology.7
In the wake of these comments, 16 health plans consisting of different payer archetypes—national plans, regional plans, integrated delivery networks, and pharmacy benefit managers (PBMs)—and representing nearly 100 million commercially insured lives (~65% of all commercial beneficiaries) were surveyed to understand the current and future utilization of co-pay mitigation programs and the impact to patient access services, including manufacturer sponsored co-pay and patient assistance programs.
What Health Plans Are Saying: Payers Push Forward
Currently, most health plans require co-pay mitigation programs for their commercially insured beneficiaries. In fact, of the sampled payers, 83% of sampled lives have implemented co-pay accumulator programs and 73% have implemented co-pay maximizer programs (see Figure 1). Additionally, while products covered under pharmacy benefit are the focus of co-pay mitigation programs, some payers described using these programs for products covered under medical benefit as well, expanding the volume of affected drugs (see Figure 2).
Figure 1: Current Utilization of Co-pay Mitigation by Sampled Commercial Lives
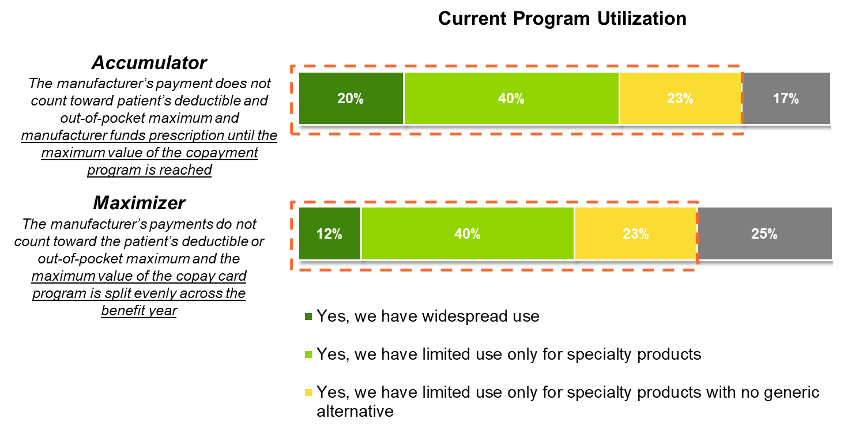
Source: Guidehouse Primary Research Analysis (2020), N=16 representing 65% of commercial lives adjusted to 100%
Figure 2: Co-pay Mitigation Program Product Types by Sampled Commercial Lives
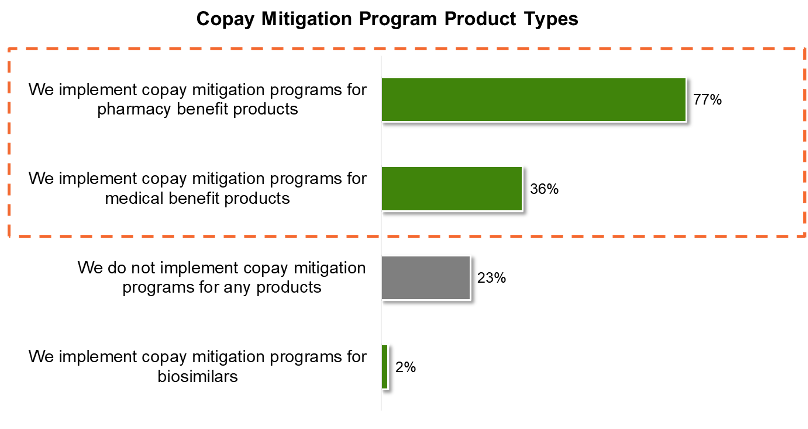
Source: Guidehouse Primary Research Analysis (2020), N=16 representing 65% of commercial lives adjusted to 100%
Co-pay mitigation programs are largely used for high-cost specialty products as they are most often associated with manufacturer sponsored co-pay assistance programs. In fact, almost all sampled payers ranked rising pharmaceutical cost as a top 3 factor in the adoption or potential adoption of co-pay mitigation programs. Payers rely on provider or patient reporting to track prescription cost contribution, with limited coordination with the manufacturer. As such, these programs raise ethical concerns as reporting cost contribution can “threaten patients’ access to treatment” leading to “discontinuation of treatment, often with disastrous consequences” as suggested by ACR in its petition to UHC.8
Even with the rising pushback from patients and providers, payers anticipate increasing their utilization of co-pay mitigation programs in the future to combat rising costs of care and introduction of new forms of co-pay support. Additionally, despite the introduction of laws in four states (Illinois, Virginia, West Virginia, and Arizona) requiring payers to count manufacturer assistance toward patient OOP costs and deductibles, our research found that 52% of payers by commercial lives do not anticipate legislation to impact their use of co-pay mitigation programs and 28% are not aware of any co-pay legislation. This is expected to shift as additional states are in the process of introducing co-pay legislation.9 As these programs become more prevalent, payers anticipate both an increase in patient inquiry and manufacturer contribution to prescription cost (see Figure 3) as the growing complexity of obtaining medically necessary drugs impedes patient access.
Figure 3: Anticipated Activity from Increase in Co-pay Mitigation Programs by Sampled Commercial Lives
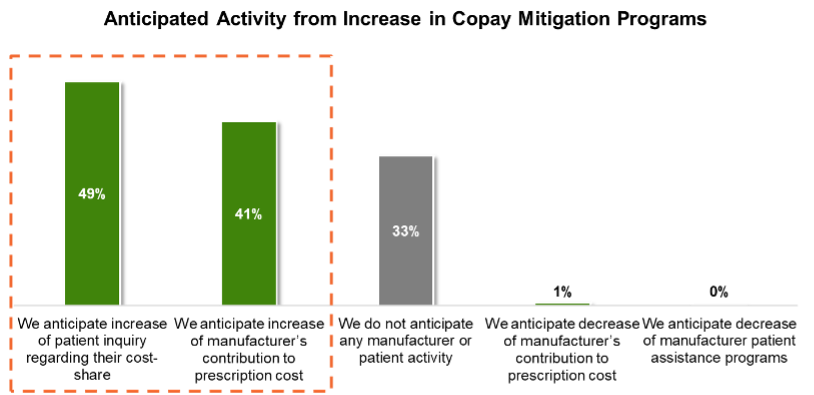
Source: Guidehouse Primary Research Analysis (2020), N=16 representing 65% of commercial lives adjusted to 100%
Manufacturers Push for Patient Access
While this research shows a trend toward increased payer implementation of co-pay mitigation programs, state legislation and advocacy efforts may suppress the actual utilization of these programs. Based on these findings, there are multiple key areas to explore:
- Monitoring the legislative and health plan landscape to understand state level exposure to these programs
- Guidance to patient support services and field reimbursement managers on communicating impact
- Assessment of implications on government pricing (eg, Medicaid Best Price, Average Sales Price calculations)
Though the future of the co-pay landscape remains uncertain, communication and collaboration across all stakeholders will be required to prevent increasing pharmaceutical OOP burden from hurting those they were meant to help: the patients.
Author Information
Joyce Wang is a Consultant in the Guidehouse Life Sciences practice.
Kathryne Kirk is a Managing Consultant in the Guidehouse Life Sciences practice.
Chance Scott is a Partner in the Guidehouse Life Sciences practice.
References
- https://www.uhc.com/individual-and-family/member-resources/pharmacy-benefits/pharmacy-support-programs
- https://payorsolutions.cvshealth.com/programs-and-services/specialty/specialty-cost-management
- https://www.express-scripts.com/corporate/articles/copay-accumulator-programs-level-out-pocket-playing-field
- https://www.drugchannels.net/2020/05/why-do-cvs-and-express-scripts-rely-on.html
- https://www.newswise.com/articles/eleven-provider-and-patient-organizations-join-the-american-college-of-rheumatology-to-oppose-unitedhealthcare-copay-accumulator-initiative
- https://www.uhcprovider.com/en/resource-library/news/featured-news/accumulator-adjustment.html
- https://www.the-rheumatologist.org/article/acr-authors-resolution-to-address-copay-accumulator-policies-at-ama-house-of-delegates-meeting/
- https://www.rheumatology.org/Portals/0/Files/Provider-Patient-Group-Letter-UHC-Copay-Accumulator-Policy.pdf
- http://www.theaidsinstitute.org/sites/default/files/attachments/AI_CoPay_Accumulator_Adjustment_Brochure_w%20Appendix_FINAL.pdf
