- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Private Claims Data Reveal Marked Increase in Lyme Disease Diagnoses
FAIR Health published the findings of their 15-year analysis of Lyme disease, including an increase in private insurance claim lines in rural and urban areas from 2007 to 2021.
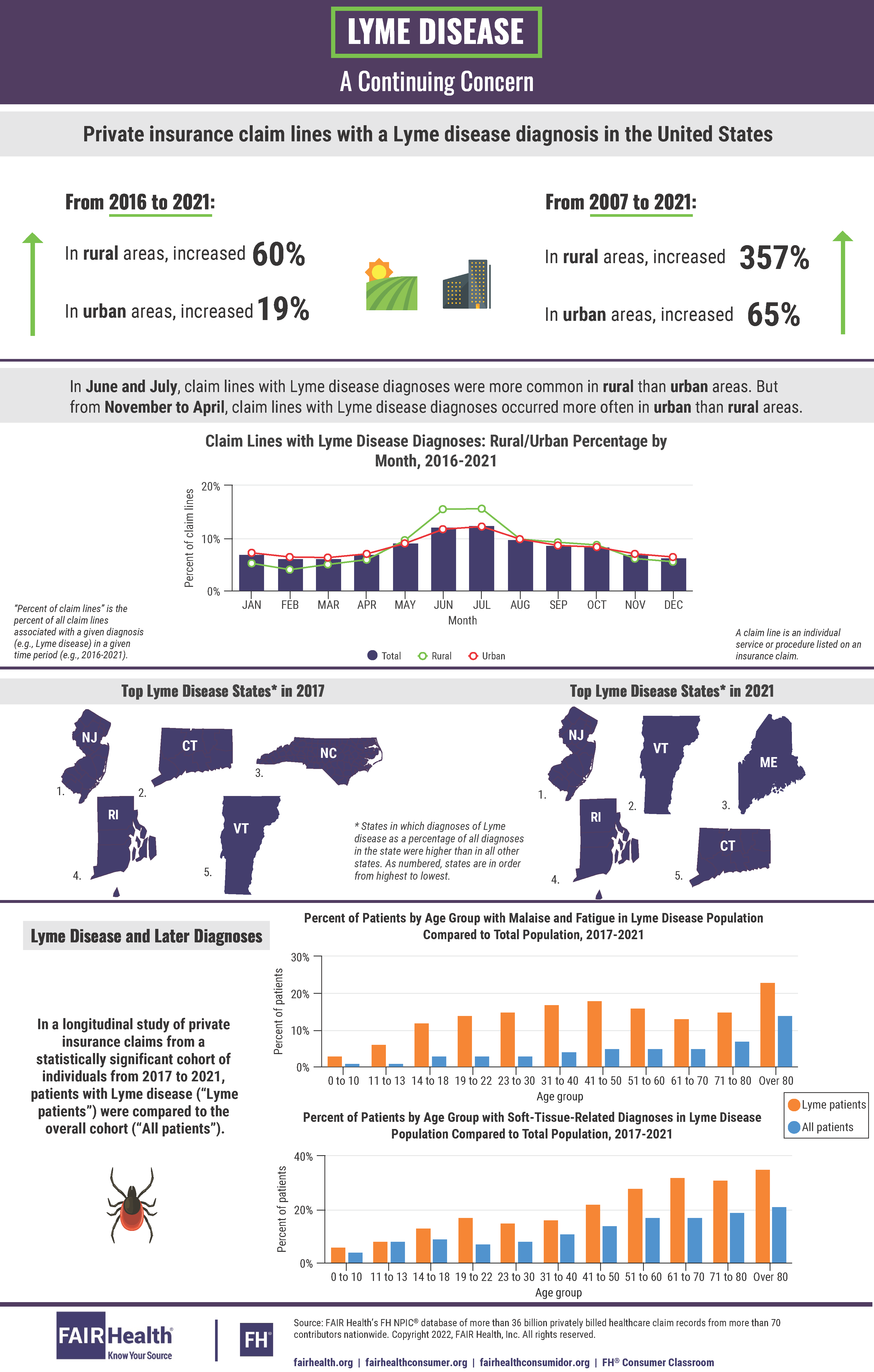
Lyme disease has experienced notable growth in the United States over the past 15 years and, as a result, has become an illness of increasing national concern. From 2007 to 2021, private insurance claim lines with Lyme disease diagnoses rose 357% in rural areas and 65% in urban areas. These and other findings on this tick-borne, bacterial illness were captured in an infographic just released by FAIR Health. The national, independent organization used its database of over 36 billion privately billed health care claims to conduct its 15-year analysis of Lyme disease; this analysis builds upon a previous FAIR Health infographic that studied 10 years of Lyme disease data.
Credit: FAIR Health
Rural and Urban Differences
The infographic reveals key differences in prevalence of Lyme disease when comparing rural and urban areas. From 2016 to 2021, claim lines with Lyme disease diagnoses increased 60% in rural areas and 19% in urban areas, with diagnoses peaking nationally in June and July of each year. During these summer months, rural areas, on average, had a greater share of claim lines associated with Lyme disease diagnoses than urban areas. From November to April, however, claim lines with Lyme disease diagnoses occurred more often in urban than rural areas.
Geographic Distribution
In 2017, the states with the greatest proportion of claim lines with Lyme disease diagnoses as a percentage of all diagnoses in the state, from highest to lowest, were New Jersey, Connecticut, North Carolina, Rhode Island, and Vermont. Given that Lyme disease has been historically associated with the Northeast and upper Midwest, the status of North Carolina as the state with the third highest percentage of Lyme disease claim lines in 2017 suggested marked expansion to a new region. By 2021, however, North Carolina had dropped from the list.
The top states in 2021, from highest to lowest, were New Jersey, Vermont, Maine, Rhode Island, and Connecticut. Maine, which was not previously on the list of top 5 states for Lyme disease claim lines, assumed third place in 2021, suggesting a growing presence of the tick-borne illness in the state. Connecticut and Vermont switched places, with Vermont emerging as number 2 and Connecticut dropping to number 5.
Later Diagnoses
Although Lyme disease is treatable with antibiotics, some Lyme patients later develop conditions with long-term symptoms, such as fatigue, muscle and joint pain, and cognitive issues. Such conditions have been linked to post-treatment Lyme disease syndrome, sometimes called chronic Lyme disease.
To identify later diagnoses associated with Lyme disease, FAIR Health examined a statistically significant cohort of individuals in its private insurance claims database from 2017 to 2021, comparing the prevalence of certain diagnoses among Lyme patients to all patients in the cohort. The analysis found that diagnoses such as malaise and fatigue and soft-tissue-related issues were more common among Lyme patients than among the total patient population. Across all age groups, patients with Lyme disease were generally more likely to have these apparently associated diagnoses than all patients in the cohort.
Lyme disease remains a growing public health concern. FAIR Health will continue to use its repository of claims data to provide actionable and relevant insights to health care stakeholders seeking to better understand the ongoing rise of Lyme disease cases.
This is the third study FAIR Health has conducted on Lyme disease, the first appearing in an infographic released in 2017 and the second in a white paper published in 2019.
For the new infographic, click here.
