- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Medication Adherence Is Not a Zero-Sum Game
Mitigating the high cost of prescription drugs is a win-win to address the complex, multipronged problem of getting patients to take their medications as advised.
Medication adherence remains an important yet vexing issue in American health care. According to the World Health Organization, medication adherence can have a more direct impact on patient outcomes than a specific treatment itself. Still, it is estimated that a staggering 50% of Americans don’t take their chronic long-term therapy medications as prescribed.1 Statistics show that each year, poor adherence contributes to more than $500 billion in avoidable health care costs, around 125,000 potentially preventable deaths, and up to 25% of hospitalizations in the United States.2
Different Types of Nonadherence
There’s a misperception that patients either take their medications or don’t; but medication adherence is not a black-and-white problem—it is painted in different shades of grey. In some cases, patients take a medication, but not per evidence-based guidelines and doctor’s orders. Instead, they might split pills or miss doses. In other cases, patients don't discontinue taking drugs when advised. For example, if they’re prescribed a statin drug, then later prescribed a replacement statin, they might not realize they should stop taking the first drug.
There is also a scenario in which patients never take a prescribed medication. This particular type of nonadherence is actually quite common, especially among patients prescribed drugs for chronic conditions that can have serious health consequences. Results of a study published in Journal of General Internal Medicine showed that 28% to 31% of new prescriptions for diabetes, high blood pressure, or high cholesterol went unfilled.3
Influencing Factors
Why do so many patients not fill their prescriptions? The answers are complex and multifaceted. Some people misunderstand their chronic diagnosis or aren’t clear on the need for taking medication. Others may be struggling with social determinants of health, such as food insecurity, transportation, poor health literacy, and lack of access to pharmacies. All of these things correlate with nonadherence. They also contribute to the $500 billion in annual medical costs, as nonadherent patients often need hospitalization, emergency treatment, or other interventions. In other words, medication adherence is much more than a zero-sum game.
One of the more significant barriers to medication adherence is high prescription drug costs. According to IQVIA Institute for Human Data Science's 2020 report, prescription abandonment rates are less than 5% when the prescription carries no out-of-pocket cost; it rises to 45% when the cost is over $125 and to 60% when the cost is more than $500.
Recent statistics show that more than half of Medicare Part D drug prices are outpacing inflation, forcing millions of consumers to make difficult choices between purchasing prescriptions and covering other basic living costs. I refer to this as the Maslow Hierarchy of Needs (for health care). When people face the no-win choice between buying food and paying for their medication, they’ll inevitably cover their most basic needs like food, water, and shelter before they get to the prescribed drug.
Where Policy Solutions Fall Short
Lawmakers and regulators have been trying to get ahead of cost-related adherence issues to improve outcomes and reduce overall health care spending by implementing policy solutions. These initiatives aim to curb costs primarily by making medication price information more accessible to consumers. Specifically, the CMS drug transparency rule, which went into effect in January 2022, requires all Medicare Advantage and Part D plans to offer a drug price transparency tool that can be integrated into physician electronic health records (EHRs).
While many of these actions push the market in the right direction, experts question whether EHRs are a viable channel to convey drug price information and stimulate patient-doctor dialog about care costs. In the traditional prescribing workflow, identifying what medication is best for a patient is usually done outside the EHR. Furthermore, it’s typically only done the first time a drug is prescribed.
These policy solutions fall short in other vital areas as well. For example, they do little to address the significant segment of patients who never fill their medications, as previously described. These patients will remain overlooked because of a data disconnect between pharmacy benefit managers (PBMs), providers, and patients. PBMs do not have 2-way access to medical data in EHRs that show when a medical condition was diagnosed that requires new medication. So, there’s no way of knowing when drug prescriptions go unfilled.
What’s more, PBMs rely on general, nonspecific formularies when conveying information on lower-cost alternatives, such as generic drugs and biosimilars. As a result, the information is often wrong or out of date. Encouraging the use of generic drugs and biosimilar medications instead of comparable brand name options is a promising way to improve affordability for patients. This strategy has already created savings topping $338 billion in 2020 alone, including $109.6 billion in savings for Medicare alone. More than 90% of generics are filled for less than $20 in out-of-pocket costs, with an average co-pay of just over $6.60, according to the Association for Accessible Medicines.
Exploring Data-Driven Solutions
To help overcome cost-related nonadherence, we must equip pharmacists and clinical care providers with up-to-date insights about lower-cost alternatives based on formularies for each individual’s health plan. Plans must also ensure that members at the greatest risk of cost-related nonadherence are given the option to choose lower-cost prescriptions.
Analytics tools can help accomplish these goals. Advanced risk stratification solutions can identify members with known socioeconomic challenges that may predispose them to cost-related medication adherence issues. Additional analytics capabilities can conduct automated reviews of these members’ medication lists and scan for plan-specific opportunities to make lower-cost swaps. Providing these insights to clinicians at the point of care can encourage timely conversations about affordability and empower members to make decisions that fit their budgets without compromising their health.
A Clear Return on Investment
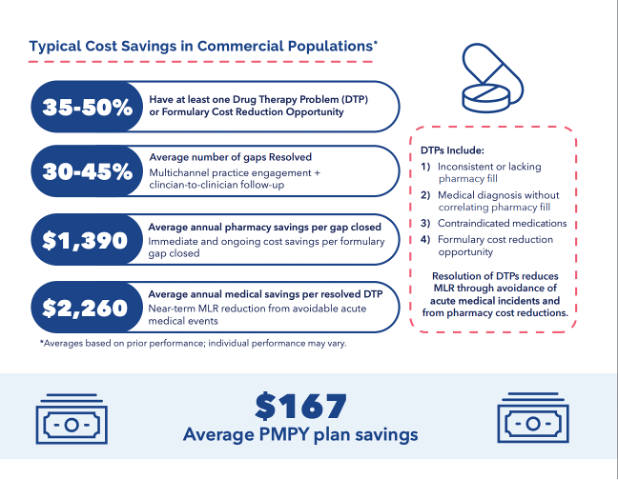
Insurers have a lot to gain by adding prescription formulary opportunity analytics into data-driven medication optimization workflows. First, they are more likely to reduce overall spending on prescription drugs. AdhereHealth analyses have consistently identified 10% to 20% total annual prescription savings opportunities, which can significantly improve a payer’s financial profile. Insurers may also save on preventable health care utilization if patients improve their adherence and keep their chronic conditions under control. Further, resolving medication gaps has the potential to reduce medical claims expenses by millions of dollars. AdhereHealth analyses show that the resolution of drug therapy problems (DTPs) reduces the medical loss ratio by an average of $167 per member per year through avoidance of acute medical incidents and pharmacy cost reductions.
Simply put, health plans can no longer afford to have avoidably high out-of-pocket costs on prescription drugs. Reducing or eliminating out-of-pocket costs can produce remarkable increases in adherence and bring corresponding decreases in per member per month costs for insurers. Adopting digital solutions that live outside the EHR to support cost-effective decision-making at the point of care can help members access their medications while creating favorable conditions for medication cost savings.
Modern tools can also intelligently create personalized reports for physician groups based on medical and pharmacy claims combined with up-to-date medication pricing information. They automatically identify medication optimization gaps for each patient and provide direct proactive outreach to resolve identified DTPs for medical cost avoidance and drug cost savings opportunities. What’s more, new solutions engage physician groups and members intuitively—giving health care consumers the information they need at the point of care, using any device, to keep costs low, avoid prescription rewrites, and prevent nonadherence based on price.
With analytics-driven strategies and actionable insights, insurers can start to turn the tide on prescription drug costs and get ahead of cost-related medication adherence challenges.
References
1. DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40(9):794-811. doi:10.1097/00005650-200209000-00009
2. McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331-1336. doi:10.1345/aph.1A333
3. Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25(4):284-290. doi:10.1007/s11606-010-1253-9
Author Information
Jason Z. Rose, MHSA, is CEO of AdhereHealth.
