- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Medication Adherence as a Journey—A Year-Round Strategy for Medicare Advantage Success
Adherence can lead to better outcomes, higher starts for Medicare Advantage plans, and stronger financial performance.
Adherence is Not a Checkbox—It’s a Journey
Medication adherence is not a box to be checked—it’s an ongoing journey that directly shapes member health, Star Ratings performance, and the financial strength of Medicare Advantage (MA) plans.
When plans embed adherence into daily operations, they are better positioned to reduce avoidable utilization, capture quality bonus payments, and strengthen member loyalty. Those that treat adherence as a short-term project risk missing opportunities for both clinical improvement and competitive advantage.
The Stubborn Challenge of Nonadherence
Despite the advances in medical science and care delivery, nonadherence remains one of the most persistent problems in health care. Nearly 89% of US adults aged 65 years and older take at least 1 prescription medication, yet as many as half do not take them as directed.
The consequences ripple across the system:
- 50% of treatment failures are linked to nonadherence.
- It drives 25% of annual hospitalizations.
- It contributes to 125,000 preventable deaths each year.
Financially, avoidable costs are estimated between $100 billion and $300 billion annually—rising to $528 billion when downstream complications are included. By contrast, members who stay adherent experience one-third fewer emergency department visits and nearly half as many hospitalizations.
Image credit: AdhereHealth
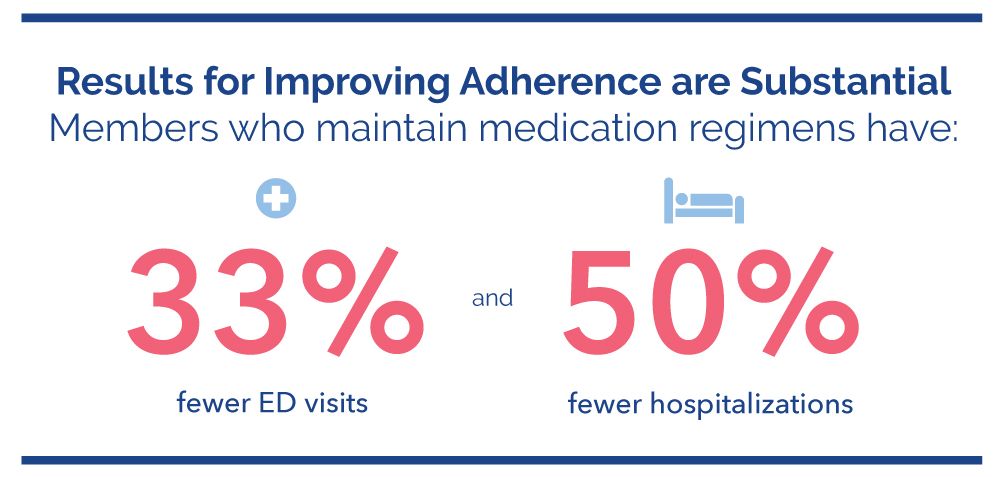
The potential for both clinical and financial gain is clear. What’s needed is an approach that treats adherence not as a point-in-time metric, but as a sustained commitment across the entire member journey.
Why the Problem Persists
Many adherence strategies still rely on one-time touchpoints or predictable, routine efforts—asking about medication use during an annual visit or sending refill reminders. These efforts help in the moment, but fail to account for adherence as a moving target.
A member adherent today may be nonadherent tomorrow. Life circumstances shift:
- A $10 copay becomes prohibitive after an income change.
- Recent transportation challenges can make the pharmacy inaccessible.
- Side effects to a new treatment can convince a member that a medication is “doing more harm than good.”
- Caregiving duties can crowd out time for self-care.
Every member is more than a set of diagnoses or claims data. Members have unique preferences, personal beliefs, and evolving life circumstances that shape their ability—and willingness—to stay on therapy. Factors such as limited health literacy, limited numeracy skills, and eroded trust in the health care system shape whether a prescription gets filled, refilled, and taken as directed. Because these realities are dynamic, interventions must be equally adaptable. Static and prescriptive outreach—like annual check-ins and 30-day refill reminders—simply can’t keep pace with members’ evolving needs.
Rethinking Adherence: From Reactive Outreach to Proactive Systems
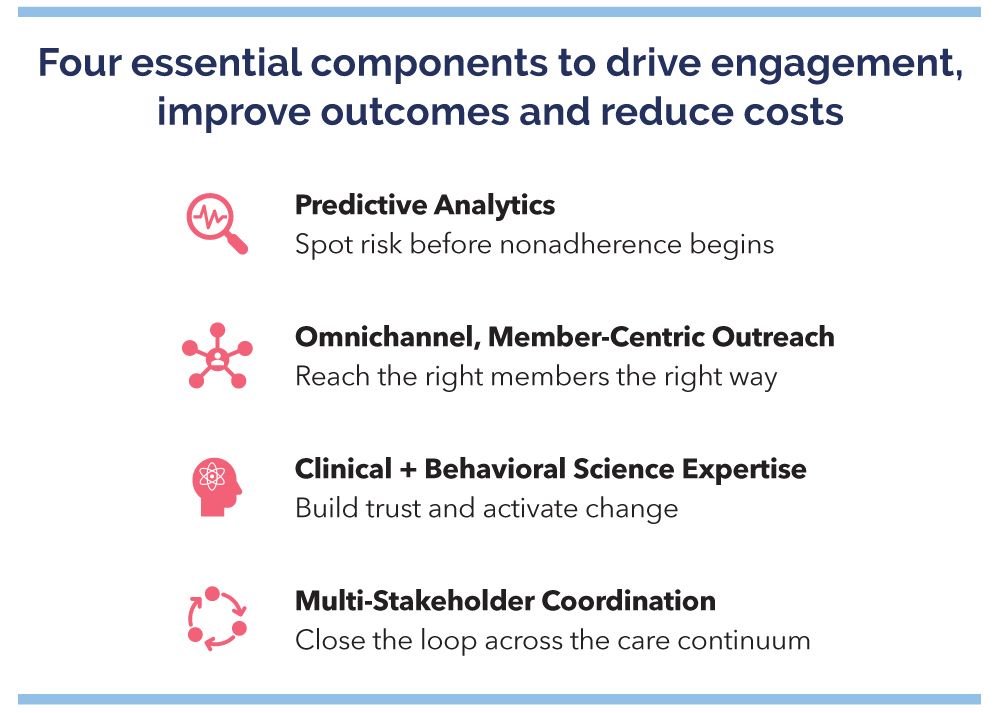
Viewing adherence as a journey means planning for the full arc of the member experience, from the moment a prescription is written to daily medication-taking decisions and adherence. For MA plans, that requires shifting from reactive interventions to a proactive, coordinated system that integrates 4 essential capabilities:
1. Anticipating risk before adherence slips. Predictive analytics identify members trending toward nonadherence—through patterns like delayed refills or gaps in medication possession—so interventions occur before proportion of days covered (PDC) rates fall below the 80% threshold.
2. Engaging in ways members respond best. No single communication channel works for everyone every time. A pharmacist’s call, supportive nurse outreach, a personalized text message or a mailed letter may all be effective, depending on member preferences and life circumstances. Outreach must be omnichannel and adaptive.
3. Applying clinical and behavioral science expertise. Data reveals who is at risk, but only science-backed communications and skilled conversations uncover why. At AdhereHealth, care teams combine clinical knowledge with proven behavioral science strategies—such as motivational interviewing and concepts like the Information-Motivation-Behavioral Skills model. This integrated approach closes members’ knowledge gaps, strengthens motivation, and builds the practical skills members need to start and sustain adherence. It also uncovers social determinants of health—like food insecurity or transportation issues—that may stand in the way of adherence, giving care teams the insight to resolve them.
4. Coordinating across the care continuum. Adherence becomes easier when the system removes friction. Providers simplify regimens and address adverse effects, pharmacies synchronize pickups and offer 90-day fills and delivery, and plans close adherence gaps with proactive prescription renewals. These operational steps make adherence the default choice.
Image credit: AdhereHealth
The Overlooked Costs—and the True Return On Investment
The value of adherence goes far beyond avoided medical claims. Lost productivity, missed workdays, caregiver strain, and reduced quality of life carry both significant human burden and economic weight.
For example, a member missing 15 workdays a year at $250 per day incurs $3,750 in lost productivity. Multiply that across a population, and the financial implications are substantial.
- Every $1 invested in improving adherence can generate $2.28 in savings from avoided health care costs and productivity losses.
- For high-burden chronic conditions such as diabetes, hypertension, and high cholesterol, annual cost avoidance per adherent member can approach $3000 per year.
- Savings come from reduced diabetes complications (~$1350), fewer heart failure hospitalizations (~$800), fewer strokes and myocardial infarctions (~$625), and less ER visits (~$200).
Image credit: AdhereHealth
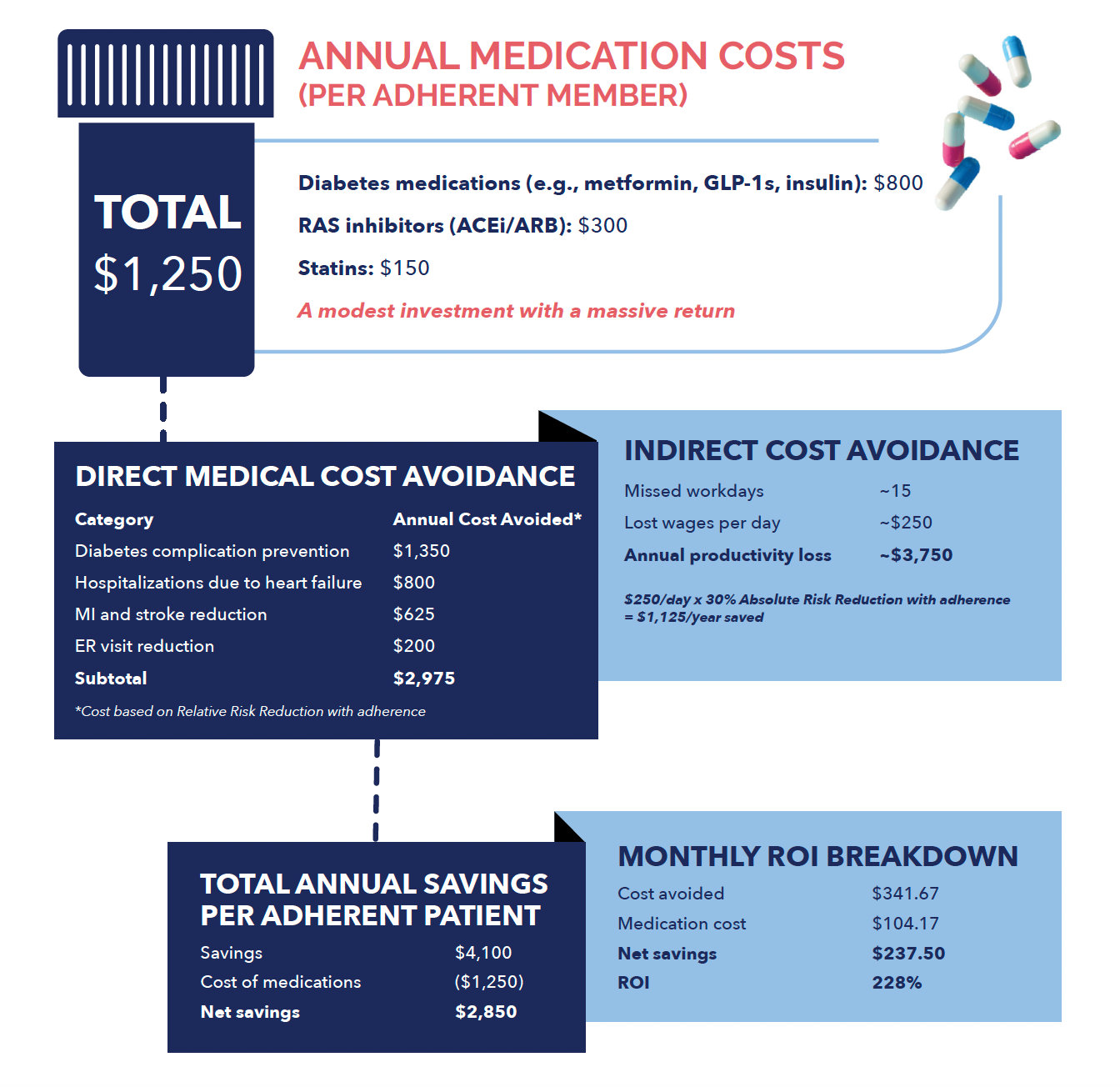
In a value-based environment, these savings can be amplified by higher Star Ratings, improved Consumer Assessment of Healthcare Providers and Systems (CAHPS) scores and year-over-year member retention.
These savings are not hypothetical. In a real-world MA population, more than half of targeted nonadherent members at mid-year became end-of-year adherent through an integrated, whole-team programincorporating omnichannel capabilities, and clinical and behavioral science intervention. Nearly 70% of those adherence gains were directly attributed to the program. Overall, 81% of triple-weighted medication measures reached the PDC ≥80% threshold—boosting both quality scores and financial performance.
A Strategic Imperative
For MA plans, the lesson is clear: improving adherence isn’t about doing more outreach—it’s about doing the right outreach, continuously, in ways that are personalized, relevant to each member’s circumstances, and sustainable.
That means:
- Year-round monitoring and engagement.
- Tailored communication to member preferences and life circumstances, rooted in clinical and behavioral science expertise.
- Coordination across providers, pharmacies, and plans.
In today’s competitive MA market, the cost of inaction is steep: missed Star Ratings, lost revenue, preventable utilization, and weakened member loyalty. Plans that embrace adherence as a journey—and invest in systems that support members throughout it—not only safeguard, but position themselves as leaders in value-based care.
Bottom Line
Every journey toward adherence is a journey toward:
- Better outcomes for members.
- Higher Stars and CAHPS scores for plans.
- Stronger financial performance in value-based care.
The smartest plans will make that journey central to their mission. With the right partner, it’s not only possible—it’s sustainable.
