- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Medicare Advantage Plans Can’t Get Complacent About Artificially Inflated 2022 Star Ratings Results
COVID-19 prompted CMS to make major adjustments to the Medicare Advantage (MA) Star Ratings System, resulting in better-than-average performance for nearly all plans. However, these changes were temporary, and MA plans will have to reset their strategies for 2023 and beyond.
In early 2020, CMS sprang into action as the COVID-19 pandemic adversely impacted elderly and disabled populations. With flexibilities in clinical care delivery and significant relaxations of Medicare Advantage (MA) plan quality measurement, CMS provided much-needed relief in a time of uncertainty and strained resources.
These concessions included expanding measure-level disaster adjustments, removing the downside impact of any decrease in measure performance, and delaying the implementation of cut-point guardrails until the 2021 performance year.
The changes allowed plans to focus on caring for their members during an unprecedented crisis. But they also made it easier for MA plans to score better than normal on key Star Ratings measures, creating an artificial bubble of high performance in the 2020 performance period.
As such, for the 2020 performance year, the average 2022 Star Ratings across a sample of 471 Medicare Advantage prescription drug plans increased dramatically to 4.37, compared to just 4.06 in 2021. This analysis excluded health plans that were not yet rated or not required to report.
Seventy-four plans earned a 5-star rating in 2022, CMS notes. In the previous period, just 21 plans reached that enviable threshold. Moreover, 60 plans receiving the high-performing icon for 2022 did not do so in 2021 Star Ratings.
Now, 68% of plans serving nearly 90% of MA beneficiaries are at or above the 4-star threshold. The relaxed rubric has brought a surge of quality bonus payments and new marketing opportunities to these new top performers.
Many MA plans are pleasantly surprised by these results, but they must temper their excitement. Lower performance thresholds and the lack of downside adjustments may have resulted in higher ratings and welcome access to additional subsidies, but this is emphatically not a new normal.
As the scoring adjustments end and additional methodology changes come into play, plans will have to work twice as hard on patient experiences, medication adherence, and holistic care delivery if they hope to make these temporary rewards permanent.
Exploring the Impact of Changes to the 2022 Medicare Advantage Star Ratings
The 2022 Star Ratings largely reflect actions taken in 2020, the first year of the COVID-19 pandemic. Due to the devastating increase in illnesses and deaths among the population 65 years and older during this time, CMS deemed it unfair to hold MA plans to the same standards of accountability as before the pandemic.
Specifically, CMS expanded the Measure-Level Disaster Adjustments and Hold Harmless provisions, thereby removing the downside of decreasing measure performance for the vast majority of measures. As a result, most plans with a measure-level Star Rating decrease reverted to the prior year’s Star Rating for that measure, effectively eliminating any vulnerability to performance decrease. Some MA plans that entered the market in 2020 were negatively impacted because they had no prior year scores to fall back on.
Because plans are also rated on year-over-year performance improvement—representing up to 10 quality points for MA Prescription Drug (MAPD) plans—these 2 adjustments will lead to a compounding effect as protections are removed and performance returns to prepandemic levels.
The federal agency also delayed the implementation of cut-point guardrails until the performance year 2021, which will be reflected in the 2023 Star Ratings. CMS feared that the guardrails – bidirectional caps that restrict upward or downward volatility to within 5% of the prior year’s measure-level cut-point thresholds—would unfairly penalize health plans for quality measure performance as they responded to the COVID-19 public health emergency. This allowed for several lowered thresholds that would not normally have occurred.
For example, the minimum cut point for a 3-star score on diabetic eye exams fell from 69% to 62%, a 7% absolute decrease from 2021 to 2022. This made it easier for plans to achieve a 3-star rating for 2022. If the guardrails had been implemented, the year-over-year absolute decrease could not have exceeded 5%.
As health plans return to more stringent measurements, they will need to recalibrate to account for upcoming changes, including the rising importance of medication measures and Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey results.
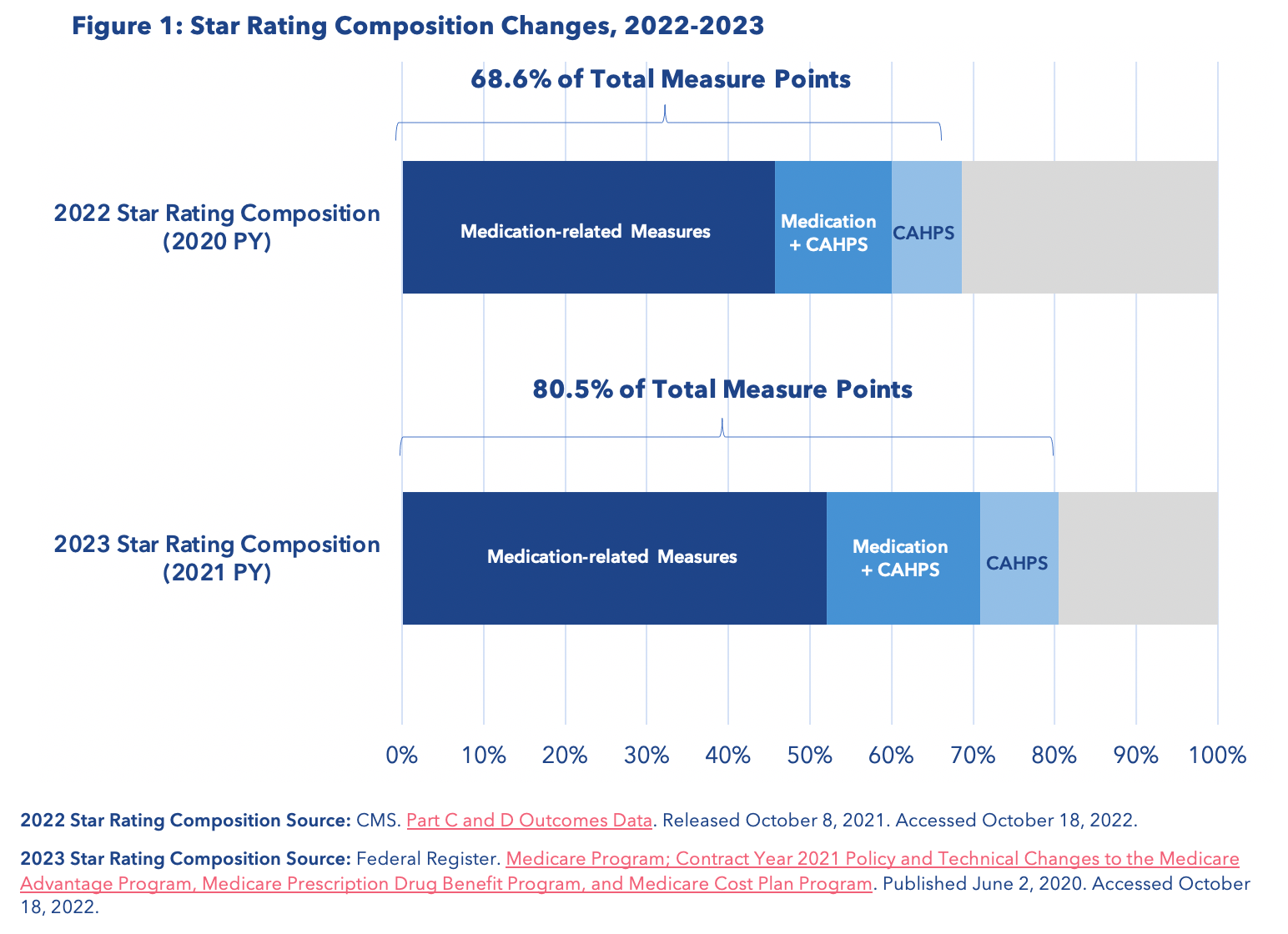
For 2023 Star Ratings, medication-related measures and CAHPS measures will combine to comprise more than 80 percent of total measure points (Figure 1). This will include the newly redesigned Transitions of Care measure that takes on a much heavier medication management component.
CAHPS measures will increase from double-weighted to quadruple-weighted in contract year 2021, comprising 32 percent of the aggregate Star Rating. Unfortunately, 2022 saw a year-over-year decline in several patient experience measures, including complaints, the ability to get needed care, and timely appeals.
Figure 1. Star Rating Composition Changes, 2022-2023
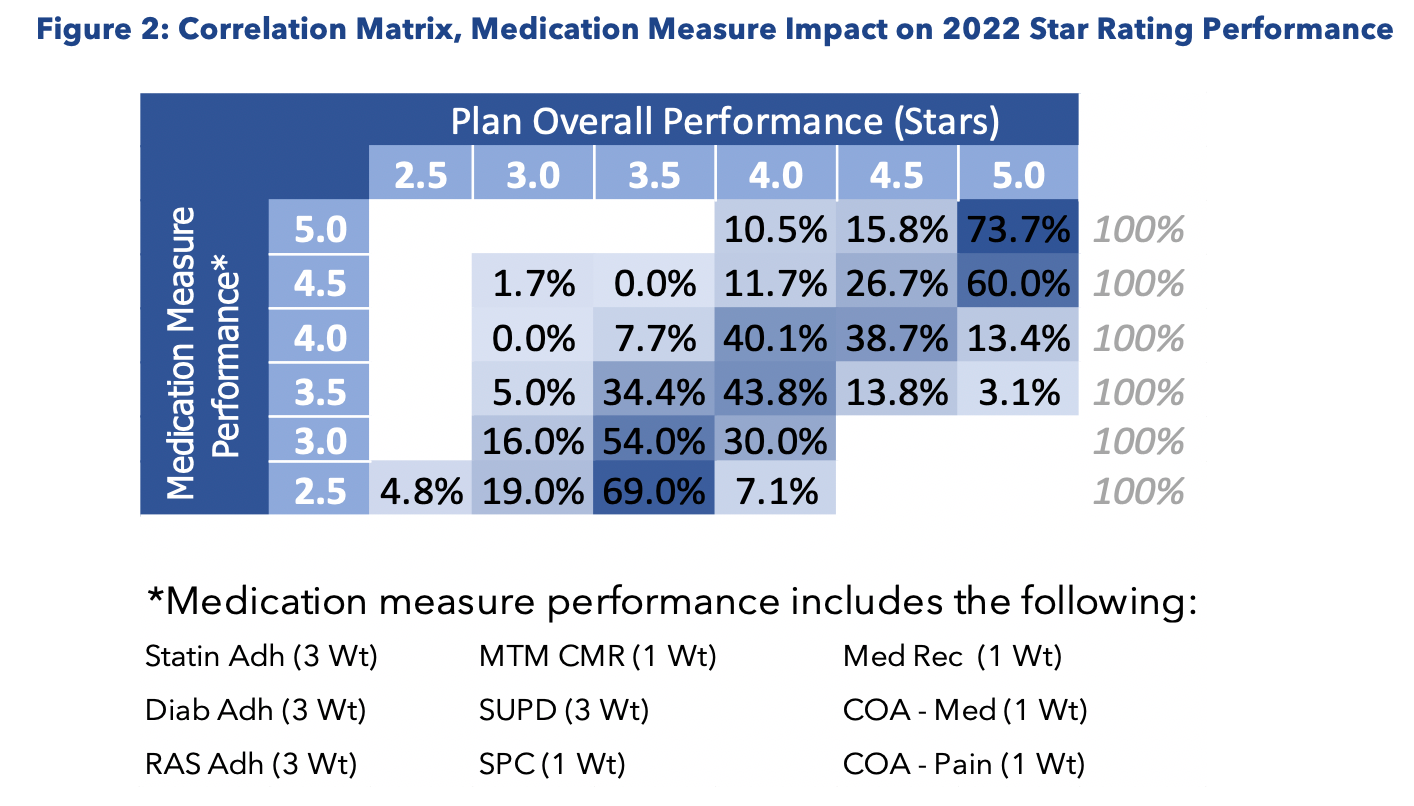
Meanwhile, poor performance on four crucial medication adherence measures actively dragged down the Star Rating scores of health plans in the 2022 Star Ratings year. For example, plans achieving 4.5 and 5 stars on medication measures were much more likely to achieve 5 stars in overall plan performance (Figure 2)—except for medication therapy management completion rate.
Plans that are struggling in these areas are now positioned for a double blow: the increasing importance of these outcome measures, coupled with the return of downside adjustments and the implementation of new guardrails, may significantly raise their odds of lower Star Ratings in future performance periods.
Figure 2. Correlation Matrix, Medication Measure Impact on 2022 Star Rating Performance
Developing Strategies for Star Ratings Success in 2023 and Beyond
Health plans are already coming to the tail end of the 2023 Star Ratings performance year, but there is still a strong incentive to start making positive changes as quickly as possible. They can start by reexamining their approach to member management and consumer satisfaction.
Despite the growing emphasis on CAHPS, it is still very common for health plans to have a disconnected approach to consumer engagement with disparate teams held accountable for different performance measures. This siloed approach results in higher health plan costs and poor consumer experiences.
Plans will need to take a comprehensive and consumer-centric approach to providing access to care by identifying every consumer touchpoint, examining each process related to that interaction, and creating a coordinated, team-based workflow that is both efficient and focused on the member’s unique preferences and needs.
Plans should ensure they offer up-to-date provider network information, multiple options for communication and engagement, and appropriate education to improve health literacy for members. With the right analytics tools, plans can also assess their population-level analysis on a continual basis to identify potential future benefit changes and individual-level action plans.
Similar strategies can be highly effective for improving performance on medication adherence and management measures, especially for members experiencing polypharmacy.
Plans may consider implementing data-driven risk stratification and CRM tools that identify high-risk, complex members in need of personalized medication adherence support.
Using telepharmacy outreach and experienced clinicians trained in motivational interviewing techniques, plans can effectively coach members toward better medication adherence and improve their likelihood of positive clinical outcomes.
MA plans should actively incorporate services to address social determinants of health, such as connecting members to community-based organizations providing meal delivery services, transportation, housing services, or other socioeconomic supports. Actively providing holistic services can improve a member’s ability to stay adherent to medications while simultaneously improving their satisfaction with getting needed care, which is an important CAHPS element.
Plans can further enhance their medication adherence strategies by offering medication synchronization, home delivery of medications, and compliance packaging that makes it easier for polypharmacy members to take their prescriptions consistently and correctly.
Key Takeaways for MA Plans
The exceptional Star Ratings of 2022 may seem like a small bright spot in an extraordinarily brutal period for MA populations nationwide. While plans should make the most of the benefits that come from their temporarily inflated ratings this year, they simply cannot afford to rest on their laurels in the years to come.
2023 and future performance periods will bring most of these rankings back down to earth, especially if plans do not make immediate preparations to contend with upcoming changes to the Star Ratings methodology. Any plan that is not actively improving member experiences and medication adherence rates risks a significant reckoning next October when the Star Ratings for 2023 are revealed.
By adopting data-driven approaches to managing CAHPS scores and focusing on supporting high-risk patients with medication adherence initiatives, MA plans can take advantage of the upcoming Star Ratings adjustments and lay the groundwork for continued success, bringing better service and better care to their members.
Author Information
Jason Z. Rose, MHSA, is CEO of AdhereHealth.
