- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Implementing Pharmacy-Led Telehealth Strategies to Help Medicare Advantage SNPs Improve Care for Older Adults Amid COVID-19 and Beyond
Pharmacy-led telehealth strategies will position Special Needs Plans (SNPs) for Star Ratings success during the pandemic and for years to come.
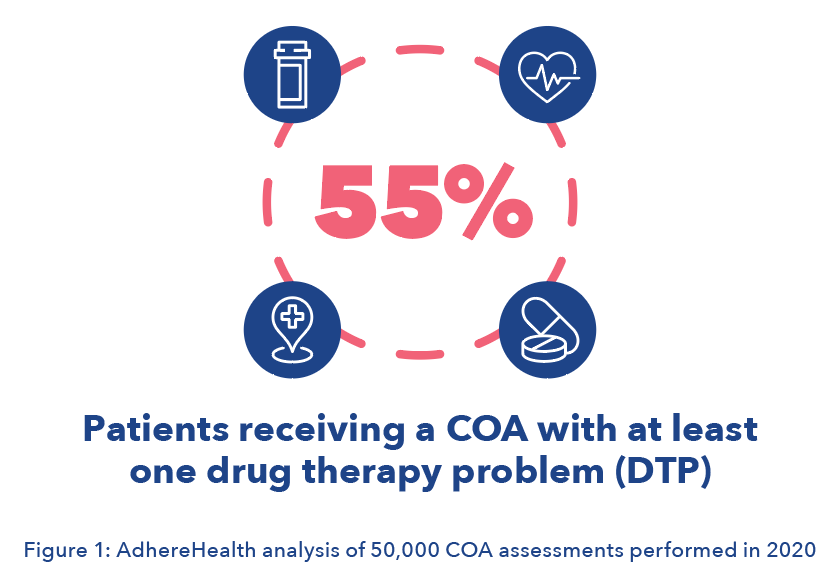
A nationwide survey found that more than half of older Americans put off medical treatment during the first month of the pandemic. Social distancing is helping curb the spread of coronavirus disease 2019 (COVID-19). However, avoidance of typical medical treatment places quality of care for seniors at higher risk, amplifying challenges for the most vulnerable parts of the population. Across the country, older adults with chronic and disabling health conditions or intellectual disabilities have been delaying essential medical care out of fear of the coronavirus. The consequence is an alarming trend—one that may be equally harmful to seniors’ health—medication nonadherence. At the end of the 2020 contract year, AdhereHealth conducted a large national telepharmacy outreach to Medicare Advantage (MA) members that qualified for Star Ratings Care of Older Adults (COA) measures. Of the membership assessed, 55% had at least 1 drug therapy problem (DTP) that would have gone unaddressed without the pharmacist outreach.
According to the CDC, the Special Needs Plan (SNP) population is disproportionately at risk of severe illness from exposure to COVID-19. Evidence shows that older people with preexisting conditions are more susceptible to needing hospitalization, intensive care, or a ventilator compared with younger patients. Last year, dual-eligibles (those eligible for both Medicare and Medicaid) that contracted the virus were hospitalized at a rate more than 5 times higher than beneficiaries with Medicare only. A growing body of evidence confirms that social determinants of health (SDOH) and medication adherence issues are key drivers of these health outcomes. Indeed, a concerning number of older adults already have unresolved DTPs because of disruptions in their medical care during the pandemic.
Now, with COVID-19 cases in the United States on the rise again, so are corresponding fears about contracting the virus during a doctor’s visit. Many seniors, especially dual-eligibles, remain hesitant to return to health services. Beyond the traditional provider setting, health plans have typically used doctors or nurse practitioners to provide targeted home assessments for higher risk consumers. However, COVID-19 concerns have led beneficiaries to decline these visits at a much higher rate in 2020 as well. Moreover, researchers now warn viral mutations may cause yet another COVID-19 wave, potentially limiting the efficacy of vaccines and prolonging the march toward immunity even further. All of this means seniors will likely remain isolated and continue to defer care for the foreseeable future. And without support for SDOH challenges, emerging problems with medication adherence could get even worse unless MA SNPs change their approach to providing needed care.
The COA Factor
CMS requires all 3 types of SNPs (C-SNP, D-SNP, and I-SNP) to perform the COA quality measures in the 2021 contract year. To avoid degradation of Star Ratings, SNPs must mitigate the impact of delay in care and reassess their strategy for delivering essential care to at-risk seniors. Intelligent clinical workflow tools can support these efforts by integrating data to provide a holistic view of the patient, including SDOH issues that may contribute to nonadherence. Modern solutions allow providers to document things like food access challenges, copayment issues, transportation access, and other barriers that may prevent access to care or medication.
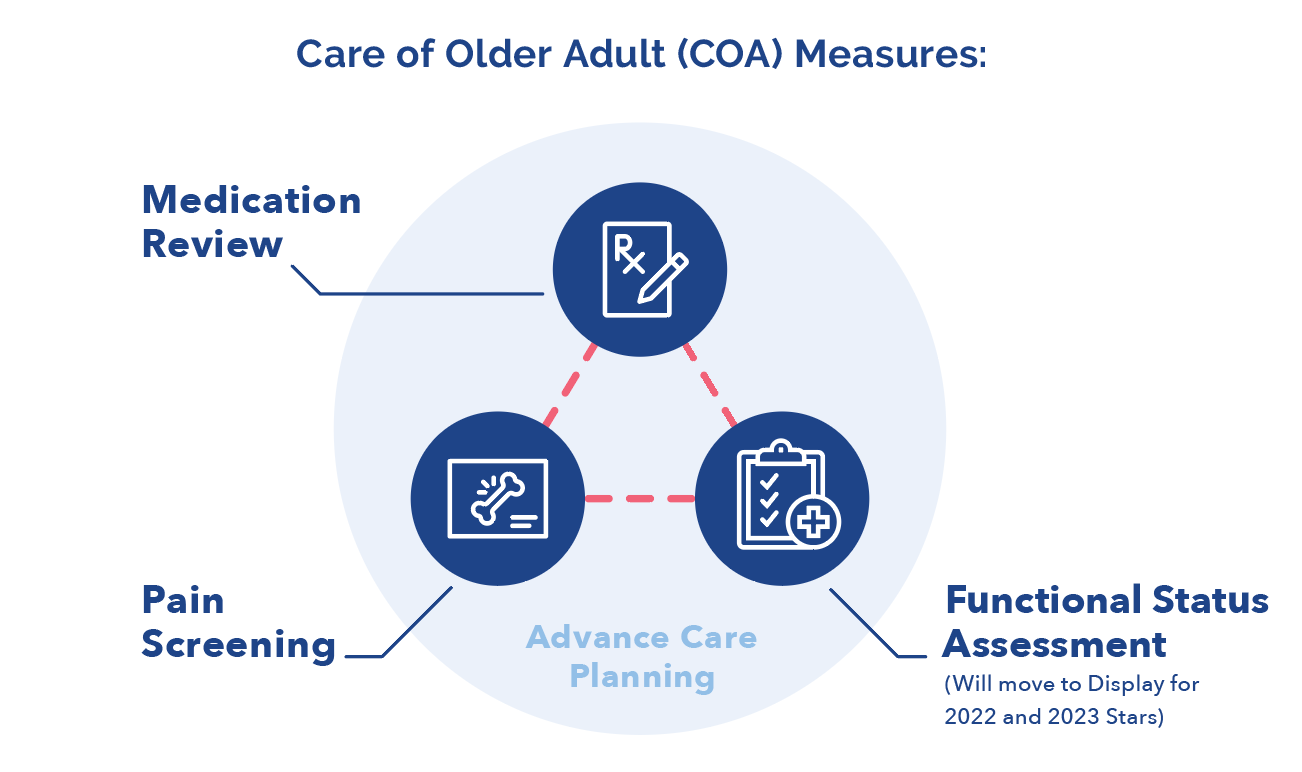
The criteria for COA requires all SNPs to document an annual Medication Review and Pain Assessment for each consumer 66 years and older. These two measures factor into the MA plan’s overall Star Ratings score. Updated COA measures will also include a Functional Status Assessment, which was retired but is coming back in contract year 2023 with a revised question set. CMS has announced Functional Status Assessment will be a display measure in contract year 2022.
Disruptions in health care caused by the pandemic have made it more of a challenge for SNPs to perform necessary COAs. As a result, AdhereHealth found a troubling number of seniors were at risk of adverse drug reactions, allergic reactions, and other safety issues related to their medications.
Beyond quality of care concerns, the importance of COA quality measures cannot be underestimated. For one, consumers who did not receive COA assessments are more likely to submit a negative response in Consumer Assessment of Healthcare Providers & Systems (CAHPS) consumer experience surveys. CMS recently made material changes for the weighting measures related to CAHPS. The Agency for Healthcare Research and Quality (AHRQ) orchestrates CAHPS surveys and supplemental items designed to capture patient experience with health care services at multiple levels of the delivery system. CMS recently determined that CAHPS measures will be quadruple-weighted beginning in contract year 2021, equaling 32% of the overall MA Star Ratings score. Plans that fall below CMS’s 4-star threshold will lose out on reimbursements from the nearly $7 billion Quality Bonus Payment pool—to the tune of approximately $500 per member per year.
CAHPS surveys ask beneficiaries (or caregivers) about their experience with their health plans and its provider network. Consumers are specifically asked:
- Has your health plan helped you get needed care?
- How well do you understand your medication information?
- How many times did you have an in-person, phone, or video visit with your personal doctor about your health?
Delayed doctor visits because of concerns surrounding COVID-19 create a conundrum for SNP when it comes to CAHPS, especially given their timing. These surveys are collected in the spring between March and May. Experts predict that normal life will not resume for most Americans until as late as next fall.
But the value of COA assessments extends even further. Combined, the 3 COA measures represent the components necessary to create an advanced care plan, which every SNP must have as part of the Model of Care (MOC) Review and Cure Processes. The MOC provides the foundation to ensure that the unique needs of each enrollee are identified and addressed by the SNP, promoting quality, care management, and care coordination processes. The NCQA scores each of the clinical and nonclinical elements of the MOC as part of its approval process. SNPs must score above 70% in order to receive final approval status for up to 3 years. In other words, SNPs must ensure COA services take place for a majority of members in order to continue operating as an MA plan.
Scaling an Intelligent Clinical Workflow Platform
To avoid a concerning ripple effect, forward-thinking SNPs are using pharmacy-led telehealth to conduct consumer outreach.The combination of predictive analytics and detailed clinical workflow software has proven essential to preserving access to needed care for beneficiaries of SNPs who have been reluctant or unable to go to the doctor amid quarantines.
These plans utilize data (eg, medical claims, pharmacy claims, hospital discharge, Healthcare Effectiveness Data and Information Set, and consumer surveys) to identify at-risk consumers. Licensed pharmacists conduct proactive outreach to vulnerable consumers via telehealth phone calls. Artificial intelligence within the clinical workflow platform will send automatic reminders prompting follow-ups to help patients stay on track with their health, from their very base needs to remembering to take daily medications.
As Winston Churchill said, “never let a good crisis go to waste.” Due to the pandemic, the telehealth industry became a prominent feature of the health care system that will surely be a permanent fixture for efficiency and consumer convenience. The demand for care through these virtual settings should persist due to several factors. However, many of these elderly and at-risk consumers do not have access to a smart phone or computer. Therefore traditional virtual visits are not a viable solution.
In this scenario, pharmacy-led telehealth outreach plays a critical role enabling SNPs to deliver necessary COA assessments. What’s more, the pharmacists are also uniquely qualified to identify DTPs and other gaps in case. For example, if a consumer is on diabetes medicine the pharmacist can help them facilitate getting a glycated hemoglobin check, clinician-documented blood pressure, or eye exam. In addition, pharmacists are specially trained to work with at-risk consumers to uncover and address SDOH issues by connecting consumers with community resources, such as meal services and transportation.
Even in the best of circumstances (ie, without a global pandemic), SNPs often hit hurdles when trying to follow through on COA quality measures. Research indicates that older adults receive only about half their recommended care, with varying quality and limited attention to social issues impacting their health (ie, SDOH). COVID-19 is making matters even worse. The following powerful real-world examples come from a sampling of over 50,000 COA assessments conducted by AdhereHealth last fall amid the second surge of the pandemic.
A patient for whom English is a second language told pharmacists she had not seen a doctor due to COVID-19 and transportation issues even though she was experiencing excruciating pain in her arm that was radiating into her spine. She did not have a caregiver and had become depressed. Her landlord used to check in on her, but now the landlord himself had health problems and could no longer come. This made her fearful about her housing situation.
Another patient told pharmacists she was being cared for by her niece, who was COVID-19 positive. Other patients revealed problems with insurance coverage, injuries from falls, and missed physical therapy appointments.
Perhaps most concerning were the significant number of instances in which patients and their clinicians identified issues with medications, many of which were moderate to severe. Specifically, the analysis found more than 55% of patients receiving a COA had at least 1 DTP that would otherwise have gone unaddressed if not for the specially trained pharmacist who connected with these consumers via phone.
Here are the DTP statistics associated with this cohort of patients:
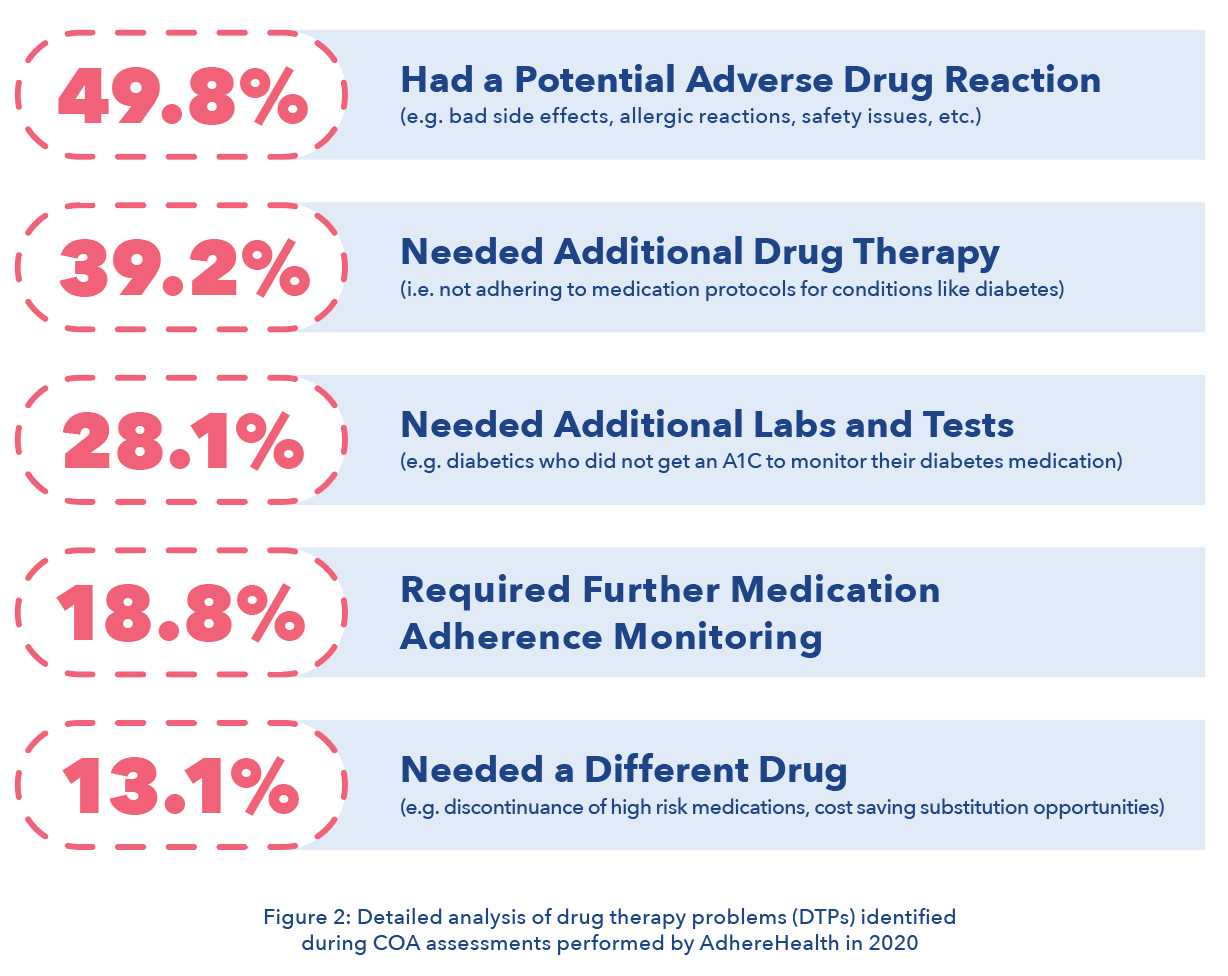
These findings are cause for alarm, not only because medication issues put these already vulnerable consumers at a higher risk for an adverse medical events, but also because medication adherence is critical to improving overall health outcomes—and in turn, integral to an organization’s MA Star Rating. More than half (52%) of the weighting for the aggregate rating is anchored to medication-related quality measures. Taken together, COA, CAHPS, and medication-related quality measures will drive 61.1% of Star Ratings for the 2021 contract year (and even more in years to come). Given the magnitude of these quality measure weightings combined with the pandemic-exacerbated barriers endemic to these vulnerable populations, SNPs must reassess their strategies now to ensure success.
Conclusions
2020 may have come to a close, but it will be some time until we truly return to “normal.” In January, the pandemic entered its 10th month in the United States. Nationally, coronavirus-related delays now account for thousands of delayed appointments and canceled doctor’s visits. Consumers still aren’t comfortable with their health plan’s in-home assessment options. Critical gaps in care will remain a challenge to address in the Medicare Special Needs sphere. SNPs need to adapt to this world and rethink their approach to ensuring quality access to care.
Despite the myriad of challenges posed by the pandemic, the crisis has also created opportunities to care for this population in new and more effective ways. Pharmacy-led telehealth can provide a marked advantage for conducting COA assessments. Additionally, these impacts go beyond COA to also affect medication-adherence measures as well as CAHPS consumer experience and SDOH-related issues. The key is reaching the right consumers at the right time, using an intelligent clinical workflow software platform to engage consumers over time in a holistic way that leverages every touchpoint with consumers, and making SDOH issues a priority in every conversation. These strategies will position SNPs for Star Ratings success during the pandemic and for years to come.
Author Information
Jason Z. Rose, MHSA, is CEO of AdhereHealth.
