- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Compliance Packaging Is Key for Improving High-risk Patient Medication Adherence
Medication adherence is crucial for managing chronic diseases, especially in complex, high-risk patients. Compliance packaging is a key tool for managing these populations.
As former US Surgeon General C. Everett Koop observed, “Drugs don’t work in patients that don’t take them.” It is estimated that half of patients with a chronic disease struggle significantly with medication adherence.
Because approximately 2 in 3 (67%) Medicare Advantage (MA) members have 2 or more chronic conditions, the number of nonadherent patients with high-risk, complex health needs is in the millions.
Medication nonadherence has both clinical and financial impacts. Across all patient populations, the overall cost burden of medication nonadherence has been estimated at half a trillion dollars in the United States annually. For MA plans, deploying innovative strategies to trim this waste by improving medication adherence is essential for delivering cost-effective, exceptional care to a growing member population.
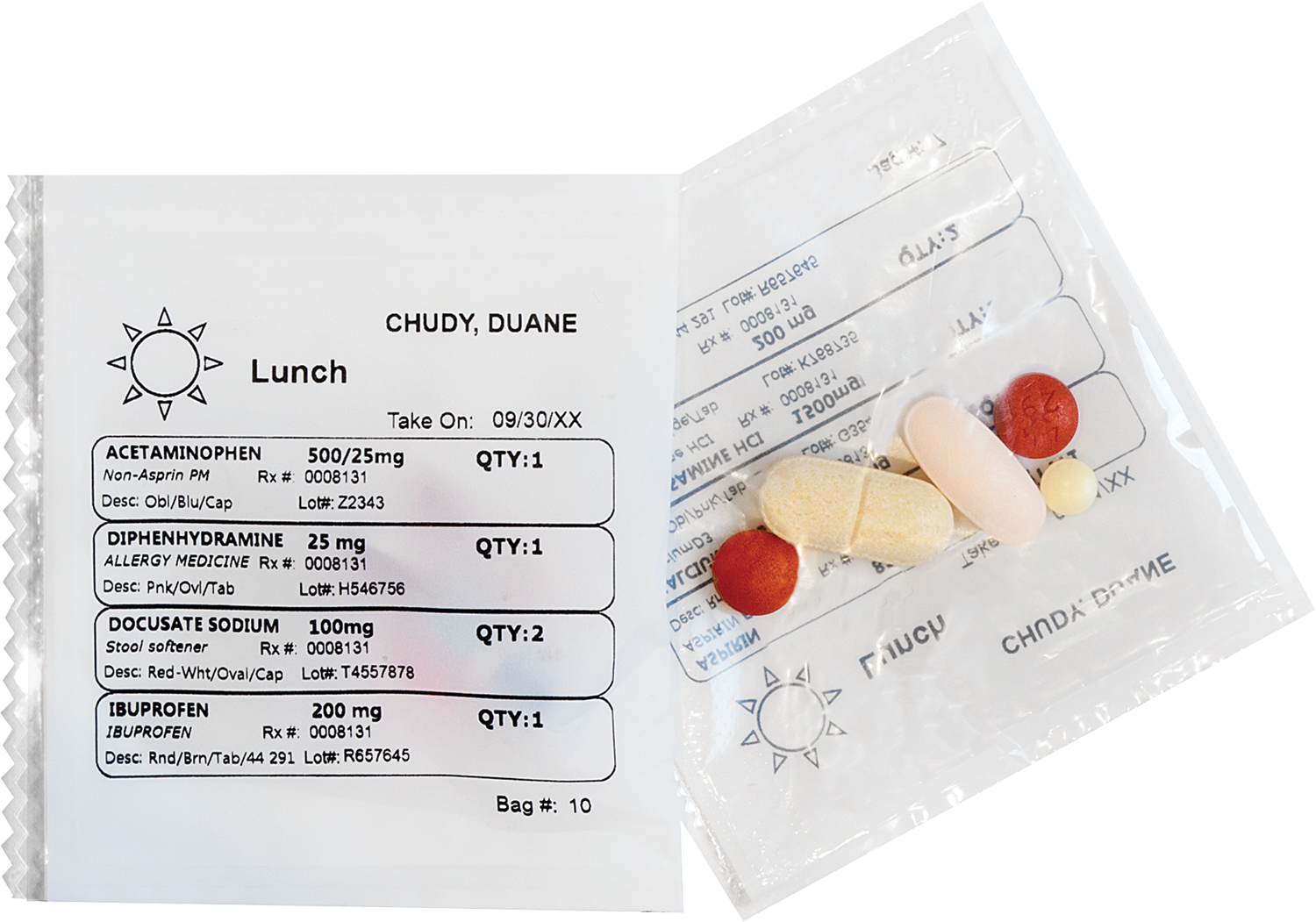
Compliance packaging is a low-cost, high impact way to help patients adhere to their recommended medications. Compliance packaging, such as blister packs and dosage strips, actively supports adherence with simplified organization, synchronized medication refills, enhanced access to medications, and streamlined management of complicated routines.
Compliance packaging
The Challenges of Medication Adherence for Chronically Ill MA Members
Medication adherence is strongly correlated with having a daily routine and strong support system to ensure members take their medications as instructed. When members are left on their own to manage 8 or 10 different medications every day, they often fall out of compliance.
One large research study found that 62% of polypharmacy members sometimes forgot to take their drugs as prescribed, while 37% ran out of their medicine before they could secure a refill, and 23% admitted that they were not careful enough with how they took their medications.
These issues are directly tied to higher costs and worse outcomes. For example, a recent study found a 2-fold increase in the likelihood of hospitalization for patients with diabetes who were nonadherent to oral antidiabetic medications. Another study indicates that patients with high cholesterol and high blood pressure commonly delay or forgo treatment, a decision that likely contributes to an increase in both cardiovascular event risk and health care costs.
For many of these individuals, the social determinants of health (SDOH) contribute significantly to these problems. Low health literacy levels, lack of access to transportation, insufficient funds to pay for medications, and other socioeconomic limitations contribute enormously to nonadherence.
MA plans are responsible for a large number of beneficiaries facing the dual threat of deeply rooted SDOH factors and multiple chronic conditions. According to 2018 data, patients with 1 chronic condition were 55% more likely to choose MA compared to patients with no such conditions. Those with 3 or 4 conditions were 75% to 80% more likely to go with MA, and those with 5 or more conditions were 70% more likely to select MA.
With so many vulnerable members, MA plans have a strong incentive to invest in medication adherence tools that can reduce costs and improve outcomes at scale, especially as the nation moves more deeply into the arena of value-based care.
The Role of Compliance Packaging in Medication Adherence
There is clearly an immense need for patients to better manage their chronic conditions with prescribed medications. Compliance packaging, also known as multimedication packaging, can close the gaps.
Blister packs and dosage strips with pills organized by date or time of day can easily streamline the management of medication routines.
Blister packs

Pharmacists can also synchronize medications so that members receive an appropriate supply of their drugs on a single “anchor date” instead of being forced to coordinate refills several times a month, sometimes with more than one pharmacy. Meanwhile, proactive outreach from pharmacists and care managers can ensure that members understand their regimens and have access to clinical and community resources that can help keep them on track with their overall health.
Compliance packs can even be hand delivered to members with a courier service, ensuring that individuals with daily living limitations or lack of access to transportation will always receive their medications on time.
The Multifaceted Benefits of Offering Compliance Packaging
Incorporating compliance packaging options for members with 8 or more prescriptions can bring swift positive results to members, caregivers, and MA plans alike.
In addition to relieving daily burdens on members and their family members, compliance packaging has been shown to raise adherence rates and potentially improve subsequent clinical outcomes.
In one analysis, for example, transitioning to compliance packaging resulted in a mean adherence rate of 71% compared with just 63% among control subjects using traditional methods. Researchers cited the use of blister packs as a key factor for success.
MA plans also stand to gain from happier, healthier, more adherent patients. Medication adherence rates can be a crucial lever for securing a high MA Star Rating, since half of the weighting for a health plan’s rating is anchored to medication-related quality measures. What’s more, Consumer Assessment of Healthcare Providers and Systems measures in MA Star Ratings now represent 32% of the overall weighting in 2021.
Pairing simplified, synchronized compliance packaging with a strong focus on overcoming the SDOH barriers to medication adherence may result in better outcomes, improved patient satisfaction, lower costs, and a boost to the health plan’s public reputation.
Compliance packaging is a cost-effective way to support better medication adherence for high-risk patients. By adopting more intuitive and more proactive medication management strategies, MA plans can avoid financial waste and improve their Star Ratings while actively helping members attain their long-term health goals.
Author Information
Jason Z. Rose, MHSA, is CEO of AdhereHealth.
