- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
CNS Metastases in EGFR-Mutant NSCLC: Emerging Therapeutic Strategies and Ongoing Challenges
Central nervous system (CNS) metastases in EGFR-mutant non–small cell lung cancer (NSCLC) remain a major challenge, with emerging therapies and evolving trial designs aiming to improve outcomes and address unmet needs.
Central nervous system (CNS) metastases remain a major clinical challenge in the management of non–small cell lung cancer (NSCLC), particularly in tumors harboring oncogenic drivers such as EGFR mutations and ALK rearrangements.
At the 2025 World Conference on Lung Cancer (WCLC) in Barcelona, Spain, Helena Yu, MD, attending physician at Memorial Hospital and research director at Thoracic Oncology Service at Memorial Sloan Kettering (MSK) Cancer Center, presented a comprehensive overview of the biology, current treatment options, and ongoing challenges associated with CNS involvement in EGFR-mutant NSCLC. Yu highlighted recent clinical insights, novel therapeutic approaches, and evolving strategies for radiation use, while also identifying key areas for future research.
Incidence and Prognostic Impact of CNS Metastases
CNS metastases are disproportionately enriched in lung cancer compared with other solid tumors, and their frequency varies significantly among oncogene-driven subsets, Yu explained. Patients with EGFR-mutant and ALK-positive NSCLC have some of the highest rates of brain metastases, with more than half ultimately developing CNS involvement over the course of their disease.
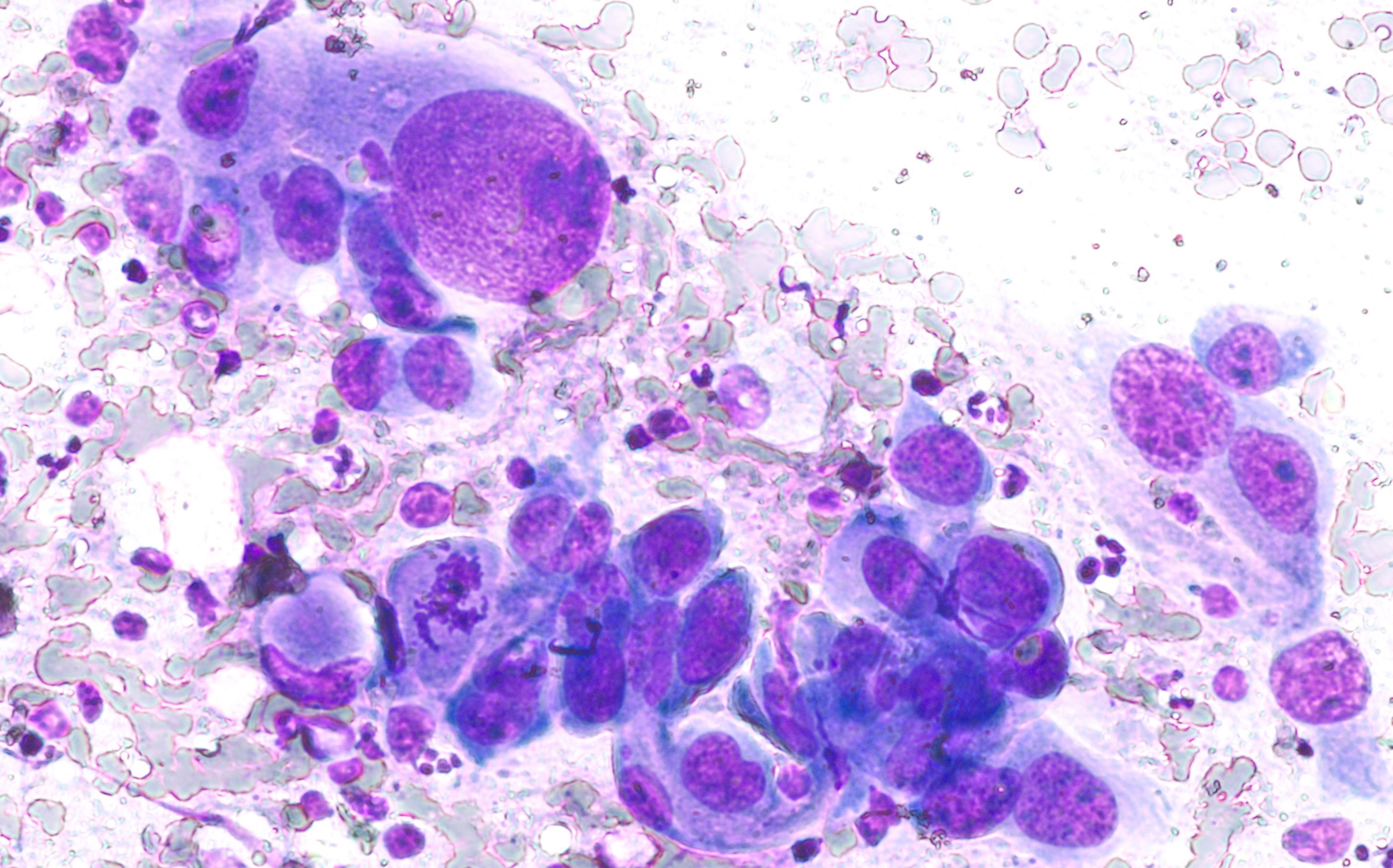
Cytology of a pulmonary nodule showing a type of non–small cell lung cancer. Image Credit: © David A Litman - stock.adobe.com
“We did this study where we looked at patients treated with first-line osimertinib [Tagrisso; AstraZeneca] to try to get a contemporary cohort to know what the baseline incidence of brain metastases and leptomeningeal disease [LMD] is, and what is the acquired CNS metastasis rate on first-line osimertinib. You can see about a third, or 36%, of patients present at the time of metastatic disease with CNS involvement,” Yu said during the WCLC session. “At 5 years, that number goes up to 54%. De novo LMD is actually quite rare, but at the 5-year mark, about 12% of patients will have leptomeningeal involvement.”
According to Yu, these findings emphasize that CNS progression remains a significant unmet need even in the era of highly CNS-penetrant tyrosine kinase inhibitors (TKIs). Prognostically, Yu noted that outcomes differ depending on whether CNS metastases are present at baseline or develop during treatment. Contrary to initial assumptions, Yu explained that patients with acquired CNS metastases or LMD on osimertinib experience worse survival compared with those who present de novo with CNS disease. Mutation subtype also influences prognosis, as patients with atypical or uncommon EGFR mutations fare worse when CNS involvement is present.
Genomic and Molecular Insights
Efforts to identify genomic determinants of CNS metastasis have yielded limited but intriguing results. Comparisons between patients with and without brain metastases identified a higher frequency of CDK11 amplifications and a lower frequency of MYCN amplifications among those with CNS involvement, according to Yu. In paired CNS and systemic tumor samples subjected to next-generation sequencing, no single-gene alterations were significantly different between compartments. However, numerical trends suggested increased PI3K pathway alterations and LSM2 amplification in brain metastases or leptomeningeal lesions, Yu explained.
Further, Yu noted that mutational signature analyses have not revealed clear associations with CNS spread, underscoring the likelihood that epigenetic and expression-level changes, rather than isolated genomic events, drive CNS tropism. This area remains a critical focus for future research, according to Yu.
Amivantamab Plus Lazertinib: A CNS-Focused Trial
Despite rapid advances in targeted therapy, systemic treatment options for patients with active, progressive CNS disease remain constrained by trial design. Most ongoing clinical studies exclude patients with untreated or progressive brain metastases and leptomeningeal involvement, limiting access to novel therapies, Yu noted. Given that over 50% of patients with EGFR-mutant NSCLC ultimately face CNS progression, these exclusions disproportionately impact this population and leave significant gaps in evidence.
To address this gap in evidence, Yu and colleagues conducted an investigator-initiated trial at MSK evaluating the combination of amivantamab (Rybrevant; Janssen Biotech) and lazertinib (Leclaza; Janssen) in patients with active CNS disease. Yu explained that 2 cohorts were enrolled: one with progressive brain metastases (n = 20) and another with active LMD (n = 21).
In the brain metastases cohort, patients had to meet Response Assessment in Neuro-Oncology Brain Metastases (RANO-BM) measurable disease criteria. Systemic response rates reached 30%, while intracranial responses were observed in 40%, demonstrating meaningful CNS activity comparable to systemic efficacy.
“When we looked at the LMD cohort, systemic responses were again around 33%. But the RANO-BM response rate was 0%,” Yu said. “Still, time on treatment for patients with LMD was quite long, with a median of 8.3 months. Progression-free survival [PFS] in the brain metastases cohort was 5.9 months, while in the LMD cohort it was 8.3 months. Median overall survival [OS] was 17.9 months in the brain metastases group and 14.4 months in the LMD group. These outcomes are much more promising than historical controls.”
According to Yu, these results suggest that amivantamab plus lazertinib provides clinically meaningful benefit in CNS disease and also underscore the limitations of current response criteria, which may fail to capture relevant neurologic or biologic improvements.
Novel Therapeutic Concepts: Iron Chelation in LMD
Emerging preclinical work points to novel vulnerabilities in leptomeningeal metastases, according to Yu. Research led by Adrienne Boire, MD, PhD, a neuro-oncologist at MSK, has shown that tumor cells within the leptomeningeal space rely heavily on iron availability. In murine models, intrathecal administration of the iron chelator deferoxamine reduced cerebrospinal fluid (CSF) iron levels and improved survival. A clinical study is now underway combining intrathecal deferoxamine with systemic osimertinib, offering a potential new avenue for tackling LMD, Yu noted.
Role of Radiation in the TKI Era
The role of radiation therapy (RT) in the context of CNS-penetrant TKIs remains an area of active debate. Retrospective studies suggest that upfront RT may improve intracranial PFS, but no OS benefit has been demonstrated compared with salvage RT upon progression. Moreover, the risk of radiation necrosis is significant, particularly for larger lesions (> 1.5 cm), where rates can approach 60% over 2 years.
“Guidelines, though not prospective data, suggest that upfront TKIs can generally be recommended for small, sub-centimeter, asymptomatic brain metastases. An exception may be patients with CNS-only disease or CNS-only recurrence, where upfront radiation may be reasonable. Still, no prospective studies have been done,” Yu said. “We can extrapolate from systemic disease, where local consolidative therapy at the time of minimal residual disease [MRD] improves both PFS and OS, but we need prospective studies to test whether that applies in CNS disease, perhaps at later time points such as MRD, where we might minimize toxicity.”
For patients with baseline brain metastases at 1 cm or greater, Yu noted that retrospective data from MSK is available looking at patients with EGFR-mutant NSCLC and brain involvement treated with either TKI alone or TKI plus upfront radiation.
“For patients with larger brain metastases at 1 cm or greater, there was a clear improvement in time to CNS progression with upfront radiation. Using machine-learning volumetric analysis in these patients, we found that residual CNS disease—meaning incomplete responses—was associated with higher rates of progression compared to those with intracranial complete response,” Yu said. “This really identifies a high-risk population: Patients who start out with large brain metastases that persist after 3 months on a TKI.”
To address this, an ongoing investigator-initiated trial at MSK is randomizing such patients to continued osimertinib alone vs osimertinib plus consolidative RT, with intracranial PFS at 9 months as the primary end point, Yu explained. This trial aims to clarify whether local therapy confers added benefit in high-risk patients while sparing others unnecessary toxicity.
Proton Craniospinal Irradiation for LMD
Another promising development lies in the use of proton craniospinal irradiation (CSI) for LMD, according to Yu. Traditional photon involved-field RT has historically provided palliative benefit without improving survival. However, a randomized phase 2 trial (NCT04343573) led by Jonathan Yang, MD, PhD, a radiation oncologist at NYU Langone, demonstrated that proton CSI significantly improved both PFS and OS in patients with LMD from solid tumors, predominantly lung and breast cancers.1-3
These findings may establish proton CSI as a new standard of care for LMD, offering the first prospective evidence of a survival benefit in this notoriously difficult-to-treat setting, Yu explained.
Challenges in Diagnosis and Response Assessment
Diagnosis and response monitoring in LMD remain highly problematic, according to Yu. Radiographic assessments are limited in sensitivity and plagued by poor inter-observer concordance, even among CNS-dedicated neuroradiologists. CSF cytology, while widely used, is also imperfect, Yu explained, as even with 3 lumbar punctures, sensitivity remains at approximately 90%, and single assessments can be falsely negative in up to 45% of patients with clinical disease.
However, emerging tools such as circulating tumor cell enumeration and CSF-derived circulating tumor DNA (ctDNA) offer more reliable, quantifiable measures. ctDNA, in particular, provides diagnostic and prognostic information, enables detection of resistance mutations (eg, EGFR C797S), and can track clearance of driver alterations as a marker of treatment efficacy. Incorporating these modalities into clinical trials may enhance diagnostic accuracy and better capture treatment benefit.
Rethinking End Points in CNS Disease Trials
Another pressing issue is the inadequacy of current response criteria, Yu noted. In the amivantamab plus lazertinib trial, the RANO-BM response rate was 0%, yet patients experienced neurologic improvement, clinical benefit, and durable treatment durations.
“As more patients with LMD are included in clinical trials, we need better diagnostic and efficacy measures. Historically, OS has been the primary end point, but patients are now living longer and being diagnosed earlier, so OS may no longer be appropriate,” Yu said.
Yu emphasized that time on treatment and clinical benefit may be more appropriate benchmarks for future studies, particularly in LMD where conventional measures often fail.
Future Directions
Yu outlined several key priorities for advancing the management of CNS metastases in EGFR-mutant NSCLC. According to Yu, research in this area should move beyond single-gene analyses to explore epigenetic and expression-based drivers of CNS spread.
“At minimum, every trial should include CNS-focused cohorts and CNS imaging, so we can understand rates of asymptomatic progression,” Yu said.
Additionally, prospective studies are needed to define the role of consolidative RT, particularly in high-risk patients with residual disease after TKI therapy. Further, Yu noted that proton CSI warrants further investigation, as it may soon become standard of care for LMD. Better response assessment strategies, including composite end points that integrate clinical, molecular, and radiographic data, will also be essential.
Finally, Yu explained that collaborative frameworks and working groups are needed to establish consensus standards for diagnosis, monitoring, and trial end points in LMD. These efforts aim to refine risk stratification, optimize integration of systemic and local therapies, and improve outcomes for patients facing CNS progression.
Conclusion
CNS metastases in EGFR-mutant NSCLC remain a formidable barrier to long-term disease control, even in the era of CNS-penetrant targeted therapies. As Yu emphasized, the heterogeneity of CNS involvement, the prognostic impact of acquired progression, and the limitations of current diagnostic and response tools underscore the urgent need for more nuanced approaches. Advances such as the amivantamab plus lazertinib combination, proton CSI, and novel strategies such as intrathecal iron chelation offer encouraging signals, but trial designs must evolve to include patients with active CNS disease and capture clinically meaningful outcomes beyond radiographic response.
REFERENCES
- Yu H. CNS metastases in EGFR-mutant lung cancers: biology, treatment opportunities, and current challenges. World Conference on Lung Cancer; Barcelona, Spain; September 6-9, 2025.
- Proton craniospinal radiation therapy vs. partial photon radiation therapy for leptomeningeal metastasis from solid tumors. Clinicaltrials.gov. Updated May 14, 2025. Accessed September 8, 2025. https://clinicaltrials.gov/study/NCT04343573
- Yang JT, Wijetunga NA, Pentsova E, et al. Randomized phase II trial of proton craniospinal irradiation versus photon involved-field radiotherapy for patients with solid tumor leptomeningeal metastasis. J Clin Oncol. 2022;40(33):3858-3867. doi:10.1200/JCO.22.01148
The Importance of Examining and Preventing Atrial Fibrillation
August 29th 2023At this year’s American Society for Preventive Cardiology Congress on CVD Prevention, Emelia J. Benjamin, MD, ScM, delivered the Honorary Fellow Award Lecture, “The Imperative to Focus on the Prevention of Atrial Fibrillation,” as the recipient of this year’s Honorary Fellow of the American Society for Preventive Cardiology award.
Listen
Promoting Equity in Public Health: Policy, Investment, and Community Engagement Solutions
June 28th 2022On this episode of Managed Care Cast, we speak with Georges C. Benjamin, MD, executive director of the American Public Health Association, on the core takeaways of his keynote session at AHIP 2022 on public health policy and other solutions to promote equitable health and well-being.
Listen
