- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Clot Formation, Fibrinolysis Assays May Help Show Important Differences Between Hemophilia A Treatments
Researchers found that in vitro clot formulation and fibrinolysis assays were able to determine the hemostatic effects of different replacement agents, as well as identify distinct pharmacodynamic responses across the different mechanisms of action.
Leveraging in vitro clot formulation and fibrinolysis assays may help guide personalized treatment for patients with hemophilia A, suggest findings from a new study.
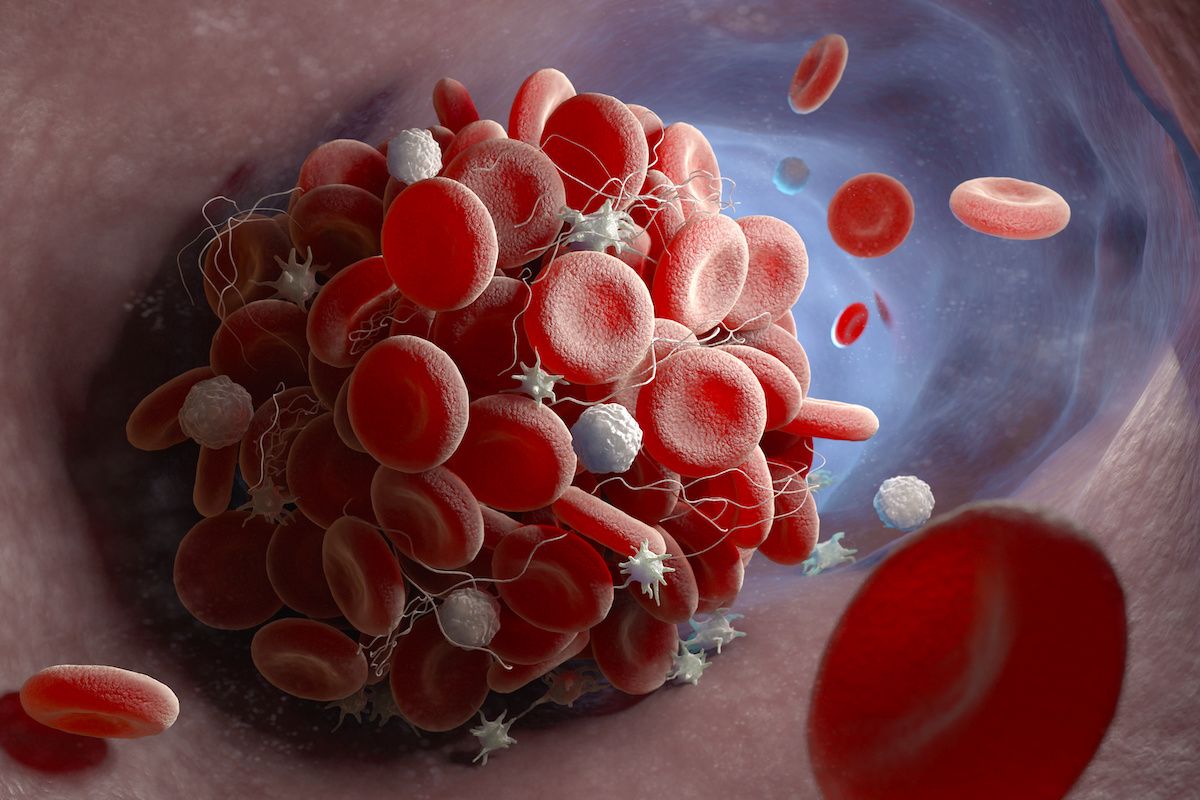
Formation of a blood clot | Image Credit: © Tatiana Shepeleva - stock.adobe.com
Detailing their findings in Research & Practice in Thrombosis & Haemostasis, the researchers of the study found that in vitro clot formulation and fibrinolysis assays were able to determine the hemostatic effects of different replacement agents, as well as identify distinct pharmacodynamic responses across the different mechanisms of action.
“The variable performance of hemostatic drugs with differing mechanisms of action in clinical hemostasis assays complicates efforts to compare agents in preclinical settings, monitor postinfusion pharmacologic responses, and optimize dosing for efficacy and safety,” explained the researchers. “Compared to normal plasma, hemophilia plasma delays clot formation and reduces stability in tissue factor-triggered assays, and products that enhance hemostasis improve these characteristics.”
All tested replacement agents corrected reduced clot formation and increased fibrinolysis observed among hemophilia-pooled plasma samples. Notably, concentration relationships and effects varied by drug, suggesting that the assays were sensitive to the different mechanisms of action.
The researchers tested replacement products, including recombinant factor VIII (rfVIII) and PEGylated rFVIII, and bypassing products, including emicizumab and activated prothrombin complex concentrate, in pooled and individual platelet-poor plasma samples. The researchers observed clot formulation and stability improvements with bypassing agents and varying trends with replacement agents.
These findings were observed among a relatively small sample of plasmas, which included plasmas from 6 males with hemophilia for the plasma pool, plasmas from 11 males for individual samples, and plasmas from 8 healthy donors.
Across the plasma pool, interassay variability was under 15% across clot formulation parameters. Similar concentrations of rFVIII and PEGylated rFVIII yielded similar effects on the plasma samples and both significantly surpassed the normal range for rate at 1 IU/mL. Meanwhile, the same concentrations of polysialylated rFVIII had a more pronounced effect and the same concentrations of porcine rFVIII had a less pronounced effect.
Notably, interassay variability was higher for fibrinolysis. Across fibrinolysis assays, rFVIII and PEGylated rFVIII showed similar effects and polysialylated rFVIII showed more pronounced activity, significantly surpassing the normal range for rate at concentrations of 0.25 IU/mL or greater.
“Conventional endpoint assays (eg, activated partial thromboplastin time) provide information on the initial events leading to early thrombin generation and fibrin fiber formation. However, additional thrombin generation and fibrin formation, maturation of the fibrin network, and generation of antifibrinolytic mechanisms that protect the clot from premature degradation occur after the clotting time,” wrote the researchers. “A strength of the in vitro clot formation and fibrinolysis assays tested here is that they can detect both the clotting onset as well as additional parameters that can differentiate normal and hemophilic clots. Consequently, these assays enabled us to study products with conventional effects on clotting, as well as nontraditional agents that do not alter onset time-based assays but enhance subsequent coagulation events that promote hemostasis.”
Among individual samples used for clot formulation and fibrinolysis assays, baseline clotting varied significantly, which the researchers expected. While all replacement products resulted in procoagulant effects, the group observed notable differences in responses to different treatments across the plasmas.
Reference
Holle L, Pantazis J, Turecek P, Wolberg A. Clot formation and fibrinolysis assays reveal functional differences among hemostatic agents in hemophilia A plasma. Res Pract Thromb Haemost. 2024;8(1):102337.
AAV5 Gene Therapy for Severe Hemophilia A Successfully Enables FVIII Production
June 20th 2024The phase 3 GENEr8-1 study demonstrated that valoctocogene roxaparvovec, an AAV5-vectored gene therapy, effectively enabled endogenous FVIII production in adults with severe hemophilia A without developing clinically meaningful FVIII inhibitors.
Read More
