- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Climate Change Impacts Allergy Health Risks: Gary Falcetano, PA-C, AE-C
Gary Falcetano, PA-C, AE-C, discussed the correlation between climate change and allergy health risks.
Temperature changes and pollution can have significant impacts on allergies, Gary Falcetano, PA-C, AE-C, US Scientific Affairs Manager for Allergy at Thermo Fisher Scientific, explained in an interview with The American Journal of Managed Care® (AJMC®). Falcetano discussed the connection between rising temperatures and prevalence of allergic rhinitis and asthma, as well as barriers to patient education and allergy management.
AJMC: How would you articulate the scientific connection between rising global temperatures and the increased prevalence and severity of allergic rhinitis and asthma?
Falcetano: There are multiple environmental factors that can impact respiratory diseases, many of which are mediated by allergies.1 Warmer global temperatures, rising CO₂ levels, and increased rainfall directly impact the intensity, duration, and geographic spread of allergen exposures—particularly pollen and mold. These changes not only prolong pollen seasons but also increase allergen potency, leading to more severe reactions in sensitized individuals.
Research shows that up to 90% of children and 60% of adults with asthma have allergic triggers that can induce or exacerbate symptoms,2 and even in patients with chronic obstructive pulmonary disease (COPD), allergic sensitization plays a role in nearly 30% of cases.3 The combination of environmental pattern changes produces a worsening situation because people encounter increased allergen amounts for longer times, which can intensify allergic rhinitis and asthma impacts.
AJMC: In your experience, what are some of the most significant barriers to effective patient education and management for individuals with asthma in the context of increasing heat waves and poor air quality?
Falcetano: It is important for patients to understand that airway inflammation can be exacerbated by both allergic and nonallergic triggers. Temperature changes and pollution, especially elevated levels of ozone and particulate matter, are 2 nonallergic triggers that can negatively impact everyone, but especially those with pre-existing chronic respiratory disease.4
Symptom control optimization must begin before environmental stressors become expected. The management of symptoms requires patients to handle their known allergic triggers while they learn to use controller medications correctly and consistently. Effective disease management requires prior guidance about extreme weather events, which should include instructions to reduce heat and pollutant contact.
AJMC: What practical, evidence-based recommendations would you provide to a patient with pollen-induced asthma to mitigate their exposure and manage their symptoms during a particularly long or severe allergy season?
Falcetano: It is important for patients to understand the full range of their potential allergic triggers, as 80-90% of individuals with allergies are sensitized to more than one allergen.5 While pollen may be a major driver of symptoms during a particularly severe season, it’s often just one part of the problem. Allergy is a cumulative threshold disease, meaning that simultaneous exposure to multiple allergens (like dust mites, pets, or mold) can worsen symptoms and make asthma more difficult to manage.
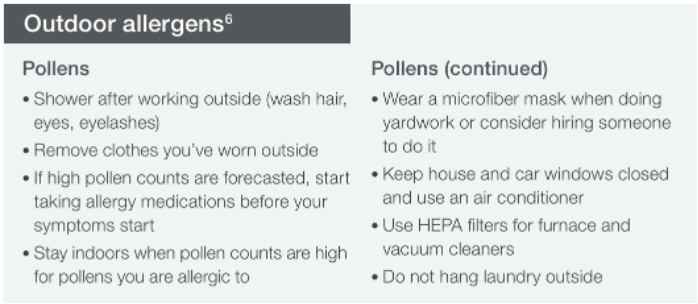
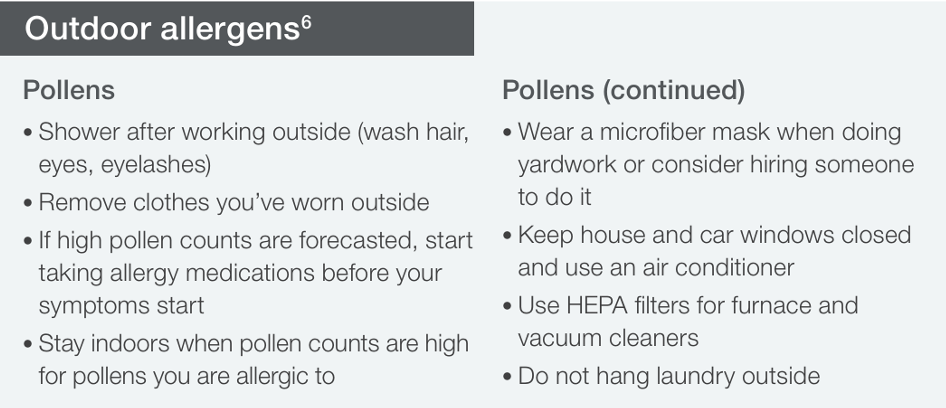
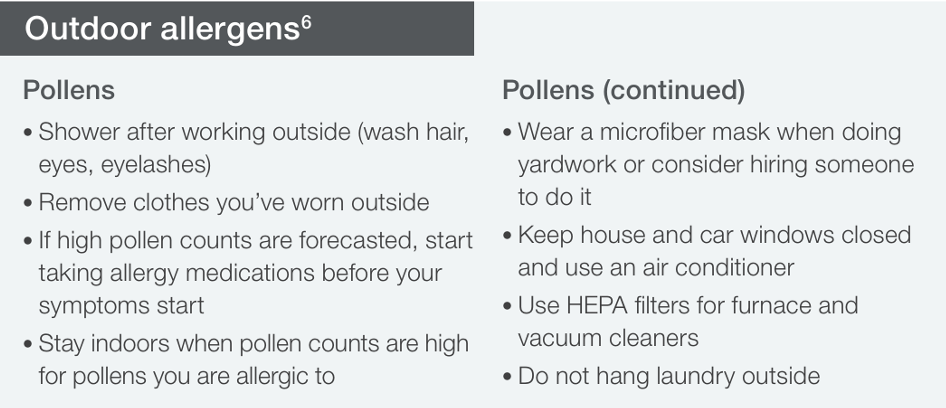
The testing of specific IgE against grasses, trees, weeds, and indoor allergens should focus on the most prevalent allergens in the patient's geographical region. Multiple national and international guidelines support this approach to help clinicians understand the individual sensitizations that may be causing upper or lower respiratory symptoms in patients. Clinical laboratories provide region-specific environmental allergen profiles that enable clinicians to obtain complete allergy trigger assessments efficiently. The Mayo Clinic provides guidelines for patients with allergies to handle pollen exposure.6
However, reducing exposure to other identified allergens can also help minimize cumulative symptom burden—potentially improving medication effectiveness and reducing the risk of exacerbations.7
AJMC: What specific populations do you consider to be at highest risk for heat-related illnesses, and what screening questions or protocols could be implemented in a clinical setting to identify them?
Falcetano: Patients at both ends of the age spectrum, as well as those with co-morbidities, are at the highest risk for heat-related illnesses. Specific populations who are economically disadvantaged and may lack access to air-conditioned living areas are especially vulnerable. Questions regarding living environments should be a standard part of any allergy assessment to identify any potential allergen exposures but also to better understand the general environmental limitations patients may be facing.
AJMC: Medications such as beta-blockers, diuretics, and certain psychiatric medications can interfere with thermoregulation. How do you think a patient should manage their medication regimen during a heatwave, and how could they be counseled on the associated risks?
Falcetano: Certain classes of medications can interfere with thermoregulation and/or fluid balance8—notably anticholinergics, including first-generation antihistamines like diphenhydramine, which carry anticholinergic properties. From an allergy management perspective and treatment standpoint, second-generation antihistamines are generally safer and equally effective.
Patients should be on the lowest effective doses and be counseled regarding the importance of avoiding overheating and staying hydrated. Patients should remain aware of symptoms of heat-related illness, such as dizziness, confusion, or excessive fatigue.
AJMC: How can collaboration with other health care professionals, such as pharmacists, social workers, or public health officials, address heat-related health risks for patients and the wider community?
Falcetano: There are multiple strategies that clinicians can employ to address heat-related health risks from a population health perspective.
- Strengthen interdisciplinary communication: Establish regular communication channels among clinicians, pharmacists, social workers, and public health officials. This can be achieved through meetings, shared electronic health records, and collaborative platforms to discuss patient care plans and community health strategies.
- Promote cross-training: Joint educational sessions help all care team members recognize and respond to signs of heat-related illness, especially in vulnerable patients.
- Engage in proactive outreach: Coordinated efforts like distributing multilingual materials, hosting community events, and leveraging local media can raise awareness of heat-related risks and preventative actions.
- Screen and support high-risk groups: Collaborate to identify and monitor individuals most susceptible to heat—such as older adults, people with chronic illness, or those lacking stable housing—and provide targeted interventions.
- Coordinate resource access: Pharmacists can advise on heat-sensitive medications, social workers can connect patients to services, and public health teams can facilitate access to cooling centers, hydration points, and emergency care.
- Inform policy and planning: Clinicians and public health professionals can contribute real-world insights to guide local policies, from expanding green space to improving emergency preparedness.
By taking a coordinated, population health approach, healthcare teams can significantly reduce the health burden of extreme heat, especially among the most vulnerable.
AJMC: Is there anything I did not ask that you would like to add?
Falcetano: Primary care clinicians are the first and often the only healthcare professionals managing most patients presenting with allergy-like respiratory symptoms. As allergic disease increases, it is especially important to move from an empiric, medication-only treatment mindset to one based upon objective laboratory data, to not only correctly phenotype patients as allergic or non-allergic, but to provide more personalized precision medicine-based approaches to correctly identify and address exposure to known allergens, focusing on the root causes of allergic respiratory disease.
References
1. Making the connection: climate changes allergies and asthma. American Public Health Association and ecoAmerica. Accessed September 18, 2025. https://www.apha.org/getcontentasset/9eb942e2-8b95-4b17-8994-65ad03c9670b/7ca0dc9d-611d-46e2-9fd3-26a4c03ddcbb/asthma_allergies.pdf?language=en
2. Allergic asthma causes, symptoms, and testing. Allergy Insider. Accessed September 18, 2025. https://www.thermofisher.com/allergy/us/en/allergy-types-symptoms/allergic-asthma.html
3. Wiginton K. Household hazards for people with COPD. WebMD. January 4, 2021. Accessed September 18, 2025. https://www.webmd.com/lung/copd/features/household-hazards-for-people-with-copd
4. Editorial staff. Too hot? How to not trigger your asthma. The American Lung Association. May 2, 2024. Accessed September 18, 2025. https://www.lung.org/blog/asthma-heat-triggers
5. Multiple allergies and the symptom threshold. Allergy Insider. February 2025. Accessed September 18, 2025. https://www.thermofisher.com/allergy/us/en/living-with-allergies/symptom-management/symptom-threshold.html
6. Mayo Clinic Staff. Seasonal allergies: nip them in the bud. Mayo clinic https://www.mayoclinic.org/diseases-conditions/hay-fever/in-depth/seasonal-allergies/art-20048343
7. Respiratory allergy toolkit. ThermoFisher Scientific. Accessed September 18, 2025. https://www.thermofisher.com/phadia/us/en/resources/library.html?resourceID=L2NvbnRlbnQvZGFtL3BoYWRpYS9saWJyYXJ5L2VuL0FQUFJPVkFMXzIwMjVfVVNfQWxsZXJneV9SZXNwaXJhdG9yeV9Ub29sa2l0LnBkZg%3D%3D
8. Heat and medications—guidance for clinicians. CDC Heat Health. June 18, 2024. Accessed September 18, 2025. https://www.cdc.gov/heat-health/hcp/clinical-guidance/heat-and-medications-guidance-for-clinicians.html