- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Children With SCD Have Limited Gastrointestinal Evaluations
Although children with sickle cell disease (SCD) frequently present with abdominal pain, limited gastrointestinal evaluations are performed for them.
Gastrointestinal (GI) evaluations may have been performed less frequently than necessary in children with sickle cell disease (SCD), as they often present with abdominal pain. According to a study published in Pediatric Blood & Cancer, evaluations specific to GI issues are needed to improve diagnosis and management of these issues.
SCD costs hospitals approximately $2.4 billion in the United States, with children with SCD reporting acute pain starting in their first years of life. There is limited data on how prevalent abdominal pain is in emergency department (ED) visits for acute pain in children with SCD. This study aimed to identify the prevalence and outcomes of abdominal pain in children going to the ED for SCD acute pain treatment.
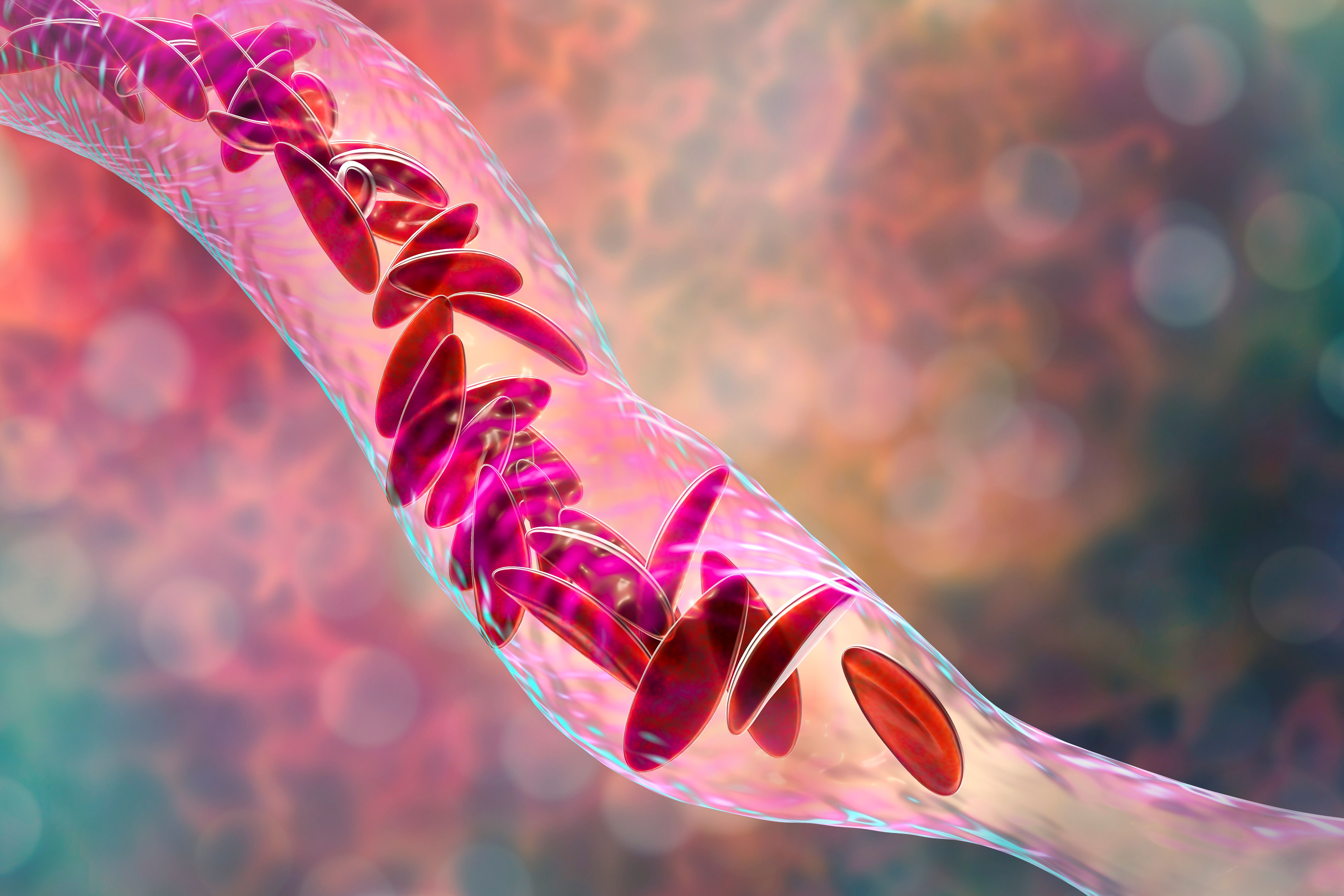
Sickle cell anemia, 3D illustration. Clumps of sickle cell block the blood vessel | Image credit: Dr_Microbe - stock.adobe.com
Children under 21 years old with SCD who went to the ED with abdominal pain or were hospitalized for abdominal pain at the Children’s Hospital of Alabama from July 2, 2020, to September 22, 2022, were considered for the study. Participants were included if they had a diagnosis of SCD and had an ED visit for pain regardless of admission. Patients not presenting with pain at the chart review were excluded. Patients were categorized as either aged younger than 5 years or 5 years and older, as health care burden increases in older children. Children were also categorized by severity of SCD.
There were 378 patients with 1279 encounters who were included in this study, 52% of whom were male. A total of 73% of the pain encounters were from 68% of the patients with sickle cell anemia (SCA). The mean (SD) age of the participants at their first repot of pain was 8.8 (5.9) years and 70% of the patients were aged 5 years and older. The median number of acute care visits was 2.
A total of 23% of acute pain encounters involved abdominal pain as a source of pain, with multiple areas of pain (31%), extremity pain (24%), and chest/back pain (22%) being the other commonly identified areas of pain. Patients who had diffuse abdominal pain were admitted to the hospital more often than those without diffuse abdominal pain (76% vs 46%); patients were 3.7 times more likely to be admitted when they had diffuse abdominal pain compared with those without.
A total of 58% of the 291 encounters with abdominal pain did not receive an abdominal radiograph or ultrasonograms. Of the 123 encounters that had imaging, 65% had an abnormality on at least 1 of the imaging modalities. The researchers found that 59% of abdominal x-rays and 67% of abdominal ultrasonograms performed were abnormal. Findings of gallstones/sludge were in 57% of abnormal ultrasonograms, 27% had a splenomegaly, 23.3% had hepatomegaly, and 6.7% had pancreatitis.
There were some limitations to this study. Underreporting of the prevalence of abdominal pain or other symptoms of GI issues is possible due to the retrospective nature of the study. Decision-making in which patients to image could not be differentiated in the study. Underlying GI pathology was possible in patients could not be reported on if imaging wasn’t done. Timeliness of analgesia and other interventions were not included in the possible risk factors for admission rates. This study also took place at a single center and may not be generalizable to other locations.
The researchers concluded that children with SCD often had abdominal pain. Studying the clinical presentation, symptoms, and signs of GI pathologies in children with SCD could help improve diagnoses and treatment.
Reference
Dike CR, Fittro S, Oster RA, et al. Gastrointestinal symptoms, diagnostic evaluations, and abdominal pathology in children with sickle cell disease. Pediatr Blood Cancer. Published online October 3, 2023. doi:10.1002/pbc.30699
First Subcutaneous Prophylaxis for Hemophilia A and B With Inhibitors Approved by FDA
December 23rd 2024The approval of concizumab-mtci (Alhemo) injection marks a significant milestone in managing hemophilia A and B with inhibitors by preventing or reducing bleeding episodes in adults and children 12 years and older.
Read More
