- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Changes in Trimethylamine N-Oxide Associated With Disease Severity, Prognosis in PAH
The prognosis and disease severity of pulmonary arterial hypertension (PAH) was found to be associated with changes in trimethylamine N-oxide.
The changes in the gut microbiota-dependent metabolite called trimethylamine N-oxide (TMAO) were found to be correlated to the prognosis of pulmonary arterial hypertension (PAH) as well as alteration of the severity of the disease, according to a study published in Therapeutic Advances in Respiratory Disease.
Several diseases can be affected by gut microbiota, which includes TMAO. Previous studies have found a negative correlation between levels of TMAO and the prognosis of pulmonary hypertension as well as coronary heart diseases. However, the association between the change in TMAO and PAH has not been explored as well. This study aimed to determine what association exists between the 2.
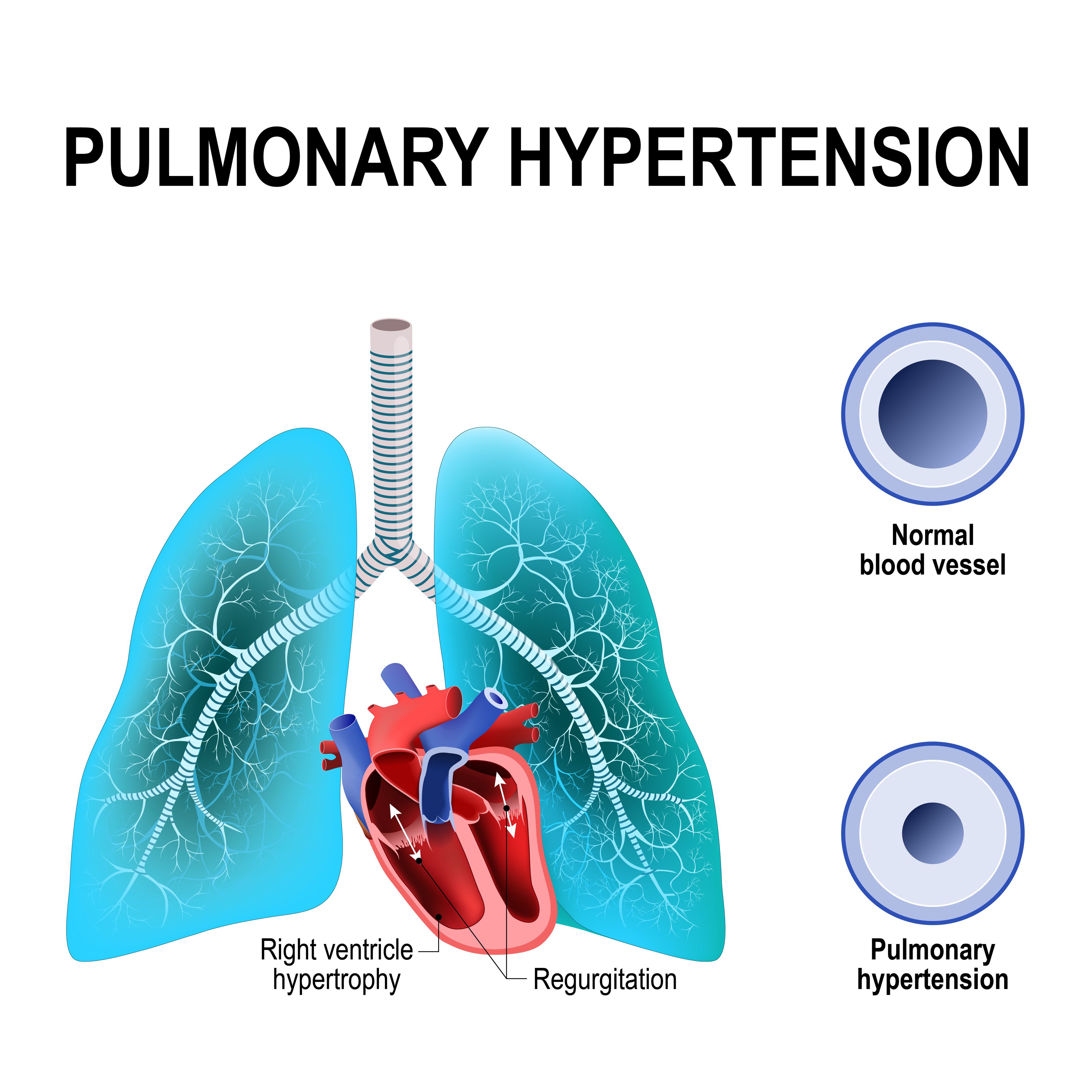
Pulmonary hypertension | Image credit: designua - stock.adobe.com
Eligible patients included those who were diagnosed with PAH associated with congenital heart disease or idiopathic PAH between May 2019 and June 2020. Patients were included if they had 2 or more measurements of TMAO and were able to be followed up regularly. An electronic medical record system was used to collect data on demographics, comorbidities, the 6-minute walking distance, and parameters from echocardiography, right heart catheterization, and laboratory tests.
Fasting blood samples were collected to examine TMAO in all patients. Baseline TMAO came from hospitalization and the second came from after an average of 6 months. All patients were followed up every 6 months until the outcome occurred or the study ended in November 2022. The median number of follow-ups was 4. Adverse clinical events, including a decline in the 6-minute walking distance, death, rehospitalization, and deterioration of pulmonary hypertension (PH), were defined as the primary outcome.
There were 117 patients included in this study, of which 45 had idiopathic PAH, and 72 had PAH associated with congenital heart disease. The patients had a median (IQR) of 25 (19-33) months of follow-up during which 39 patients had adverse clinical events and 29 cases of rehospitalization due to either heart failure or deterioration of PH. Patients were classified into 2 groups based on their measurement of changes in TMAO, less than 1.082 μmol/L and at least 1.082 μmol/L, with 1.082 μmol/L found to be the optimal cutoff.
Patients who had changes in TMAO greater than or equal to 1.082 μmol/L had a higher prevalence of chronic kidney disease (15.8% vs 1.0%) compared with the other group. Patients in the group with a change of more than 1.082 μmol/L also had a lower level of albumin, higher uric acid, and a higher level of TMAO (3.35 vs 1.23) compared with the other group.
An increased risk of adverse clinical events were found in patients who had higher levels of TMAO at baseline and the second time point and had higher changes in TMAO. A multivariable Cox analysis found a similar result, with patients with a change of greater than or equal to 1.082 μmol/L having 4 times the increased risk of adverse events compared with the other group (HR, 3.955; 95% CI, 1.486-10.527). The association was increased after adjusting for laboratory parameters at the second time point (HR, 4.050; 95% CI, 1.468-11.174).
Risk of death was also higher in the patients with higher changes in TMAO and PAH (HR, 3.980; 95% CI, 1.088-13.910). Higher changes in TMAO were still correlated with adverse clinical events in patients with PAH after excluding patients with chronic kidney disease (HR, 2.792; 95% CI, 1.291-6.040).
There were a few limitations to this study. The sample size was small and came from a single center, which could have limited the generalizability of the study. Data on the patients’ diet were not available to analyze. A microbiota assessment was also not included, even though TMAO was formed in the gut microbiota.
The researchers concluded that patients who were diagnosed with PAH had their prognostic outcomes associated with the changes in TMAO, regardless of what their baseline TMAO was. Disease severity was also affected by the changes in TMAO.
Reference
Yang Y, Li X, Wang P, et al. The significance of dynamic monitoring plasma TMAO level in pulmonary arterial hypertension – a cohort study. Ther Adv Respir Dis. 2024;18:1-13. doi:10.1177/17534666231224692
Echocardiographic Assessment Shows Promise as Risk Predictor in PAH
August 29th 2025Close to 40% of patients with right heart failure and pulmonary arterial hypertension (PAH) who remain critically ill and require admittance to the intensive care unit die within 1 year of that hospitalization.
Read More
Tricuspid Regurgitation Reliable Prognostic Indicator of PAH Severity
August 13th 2025Despite knowledge of the benefits of right heart hemodynamic measures for evaluating patient prognosis in the setting of pulmonary arterial hypertension (PAH), gaps remain in a defined role for tricuspid regurgitation as it relates to echocardiographic phenotype.
Read More
Lung Transplant Referrals Lag for High-Risk Patients With PAH
July 18th 2025Despite recommendations on early referral for lung transplantation in cases of pulmonary arterial hypertension (PAH), there is a lack of in-depth understanding of this current landscape; in this analysis, clinical parameter data were used to compare outcomes between patients who were and were not referred for lung transplantation.
Read More
