- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
CGM Use May Reduce Likelihood of Diabetic Retinopathy in T1D
This finding on continuous glucose monitoring (CGM) remained even after the researchers adjusted for glycemic control according to HbA1C levels.
In this study, continuous glucose monitoring was associated with lower odds of vision-related complications in persons with type 1 diabetes | Image credit: Koroleva-stock.adobe.com.jpeg
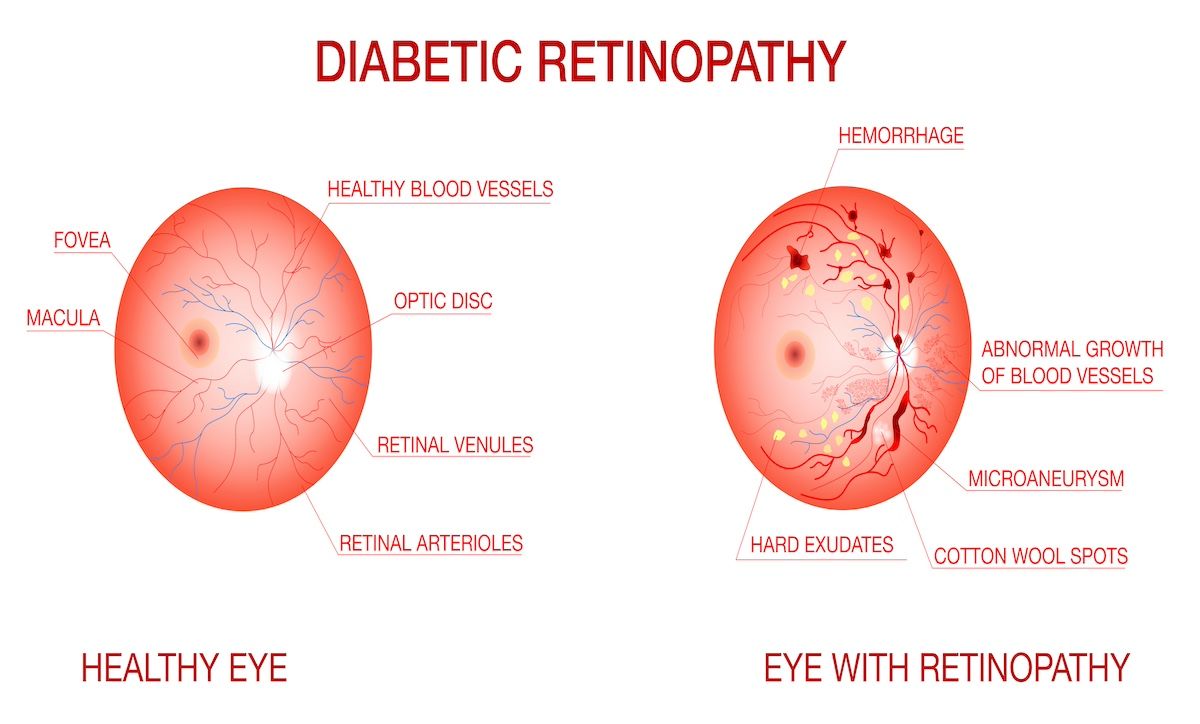
Using a continuous glucose monitoring (CGM) device could help reduce the risk of vision-related complications in patients with type 1 diabetes (T1D), say study findings.
The retrospective findings, published in JAMA Network Open, show that among adult patients, CGM was associated with lower odds of diabetic retinopathy (DR) and proliferative DR—the primary outcome measure of the study. This finding remained even after the researchers adjusted for glycemic control according to HbA1C levels.
“As the use of CGM in the management of T1D continues to increase, it may help mitigate the development of DR and vision loss related to diabetes, and thus should be encouraged in the management of diabetes,” wrote the researchers. They also noted that CGM use likely reduces fluctuation in glucose levels even as mean glucose levels remain the same, thus having a protective effect against diabetes complications such as DR.
Among the 550 patients included in the study, who attended a tertiary diabetes center and ophthalmology center between 2013 and 2021, CGM use compared with no CGM use was associated with an OR of 0.52 (95% CI, 0.32-0.84; P = .008) for DR and 0.42 (95% CI, 0.23-0.75; P = .004) for proliferative DR in multivariate analysis.
The researchers noted a diverse range of patients were included in the study; 24.5% were Black/African American, 4.9% were Hispanic, and 68.4% were White. A similar amount of patients accounted for Area Deprivation Index scores by quintile.
Nearly half (47.5%) of patients used a continuous glucose monitor and insulin pump, 62.7% used a monitor only, and 58.2% used an insulin pump only. Using just an insulin pump did not show any associations with DR, the researchers found, straying from previous research, including one study that found use of an insulin pump was associated with a reduced risk of the complication among young and pregnant patients.
Throughout the study period, 44.4% (n = 244) of patients, with a median duration of diabetes of 20 years, received a DR diagnosis. Several factors were associated with an increased risk of DR, including longer duration of diabetes (OR, 1.07; 95% CI, 1.04-1.09; P < .001), having other microvascular complications (OR, 8.87; 95% CI, 5.60-14.06; P < .001), and mean HbA1C (OR, 1.29; 95% CI, 1.11-1.50; P = .001).
“From the landmark Diabetes Control and Complications Trial in patients with T1D, it is known that longer duration of diabetes and higher HbA1C levels are associated with worse long-term diabetes outcomes, including ophthalmic complications,” described the researchers, reflecting on the similar findings in their study. “The worldwide prevalence of DR and proliferative DR is higher in patients with T1D compared with patients with T2D. Hence, our finding that CGM use is associated with a lower odds of DR and proliferative DR development in patients with T1D, a higher-risk group, is important and enhances the American Diabetes Association recommendations that CGM use be considered standard of care for glucose monitoring in individuals with T1D.”
Over time, DR progressed in 21.8% of their patients, which the researchers noted was lower than those seen in previous studies in the early days of intensive insulin therapy and before use of diabetic technologies like CGM.
Reference
Liu TY, Shpigel J, Khan F, et al. Use of diabetes technologies and retinopathy in adults with type 1 diabetes. JAMA Netw Open. 2024;7(3):e240728. doi:10.1001/jamanetworkopen.2024.0728
