- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
CAR T-Cell Therapy Responses Differ by Race and Ethnicity, Study Finds
While response and safety may vary across racial and ethnic subgroups, progression-free survival and overall survival does not appear to differ when chimeric antigen receptor T-cell therapy is used in the treatment of patients with multiple myeloma.
This article was originally published by Targeted Oncology. This version has been lightly edited.
Differences in safety and response—but not in overall survival (OS) or progression-free survival (PFS)—were observed across different racial and ethnic subgroups when patients with relapsed/refractory multiple myeloma (RRMM) were treated with the BCMA-directed chimeric antigen receptor (CAR) T-cell therapy idecabtagene vicleucel (ide-cel; Abecma). Ide-cel is still a feasible treatment for patients with RRMM, regardless of race or ethnicity, according to findings published in Blood Advances.1
In the study, investigators examined the incidence of toxicities, adverse events (AEs), response to ide-cel, and survival. Two-hundred and seven patients with RRMM were treated with standard-of-care ide-cel, and 28% were from racial and ethnic minorities. There were 22 (11%) Hispanic/Latinx patients, 36 (17%) non-Hispanic Black patients, and 149 (72%) non-Hispanic White patients. Eight patients who identified as Asian, Pacific Islander, American Indian, or Alaskan Native were excluded due to limitations of sample size and power to evaluate group-specific effects. The median follow-up time was 9.3 months.
Differences in PFS and OS by race and ethnicity were statistically insignificant (P = .49 and P = .99, respectively), and after adjusting for clinically relevant covariates, race and ethnicity were not associated with PFS. Median PFS was 4.2 months for Hispanic/Latinx patients, 6.5 months for non-Hispanic Black patients, and 8.5 months for non-Hispanic White patients.
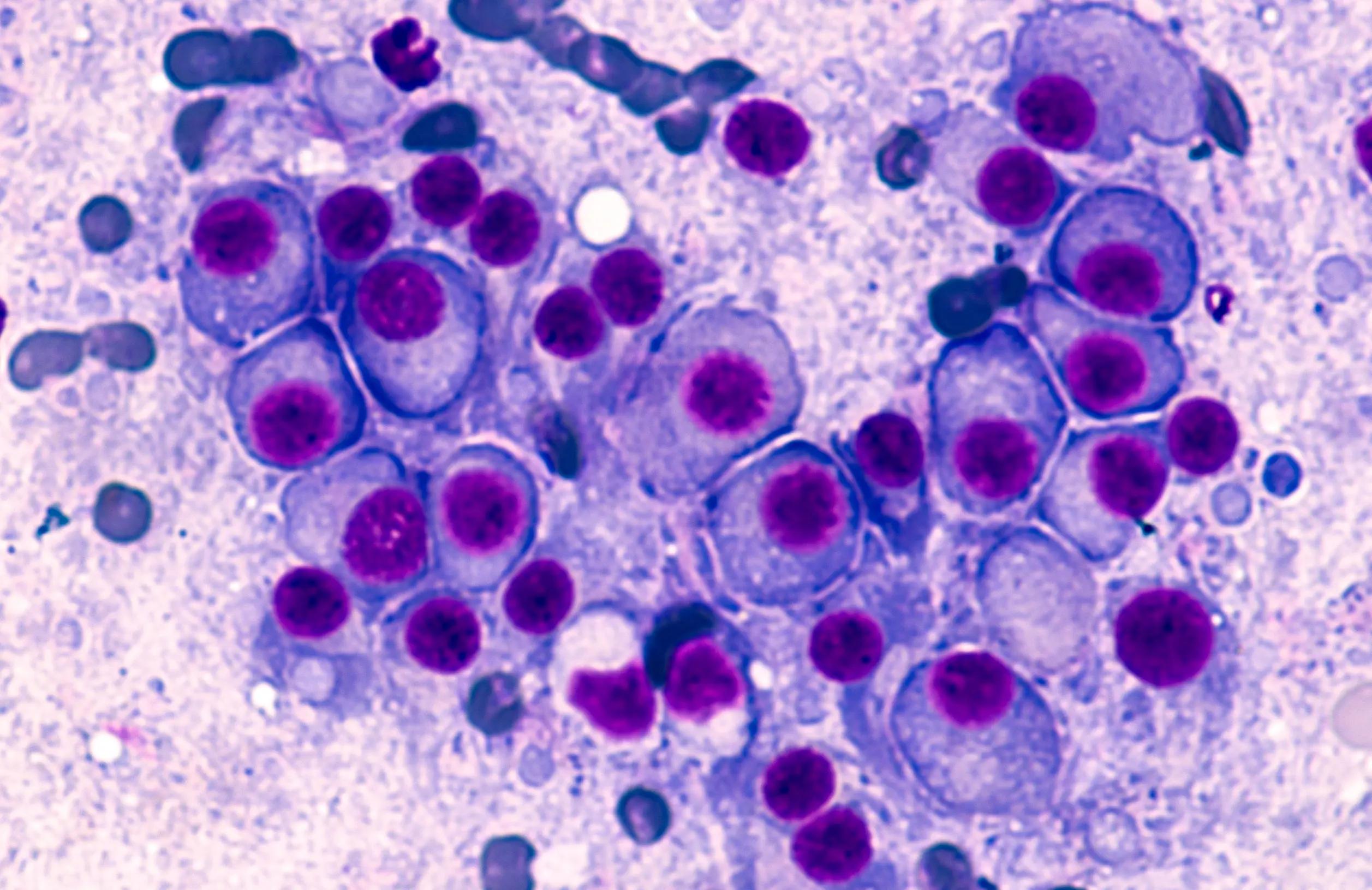
Multiple myeloma | Image credit: David Litman - stock.adobe.com
Median OS across all subgroups was not reached. However, Hispanic/Latinx patients experienced a lower best overall response rate at 59% compared with non-Hispanic Black and White patients, both at 86% (P = .01).
“These findings should be investigated in a larger cohort of racially and ethnically diverse RRMM patients treated with [standard-of-care] ide-cel with longer follow-up time,” study authors wrote.
For safety, non-Hispanic Black patients also appeared to be more likely to develop cytokine release syndrome (CRS), with 97% of non-Hispanic Black patients developing CRS compared with 77% of Hispanic/Latinx and 85% of non-Hispanic White patients (P = .04). However, there were no observed differences between subgroups regarding incidence of severe CRS grade 3 or higher, immune effector cell-associated neurotoxicity syndrome grade 3 or higher, or administration of steroids of tocilizumab (Actemra). While non-Hispanic Black patients had longer median hospital stays (13.5 days) compared with non-Hispanic White patients (9.0 days) and Hispanic/Latinx patients (8.0 days), there were no differences in intensive care unit admissions observed.
These findings were in line with another 2022 study published in Blood Advances that investigated the impact of race, ethnicity, and obesity on CAR T-cell therapy outcomes in patients with multiple myeloma and non-Hodgkin lymphoma. These findings concluded that CAR T-cell therapy could provide substantial benefit regardless of demographic characteristics, but toxicity profiles may vary across subgroups.2
“With the continued expansion of therapeutic options for RRMM patients in the SOC setting, continued evaluation of safety and efficacy across diverse patients is critical to ensure equity in the improvement of outcomes for all RRMM patients,” study authors concluded.1
References
1. Peres L, Oswald L, Dillard C, et al. Racial and ethnic differences in clinical outcomes among multiple myeloma patients treated with CAR T-cell therapy. Blood Adv. Published online October 16, 2023. doi:10.1182/bloodadvances.2023010894
2. Faruqi A, Ligon J, Borgman P, et al. The impact of race, ethnicity, and obesity on CAR T-cell therapy outcomes. Blood Adv. 2022;6(23):6040-6050. doi:10.1182/bloodadvances.2022007676
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
