- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Bispecific Antibodies Represent DLBCL Treatment Breakthrough
Analysis of single-agent, combination, and novel bispecific antibodies revealed a positive landscape of treatment for patients with diffuse large B-cell lymphoma (DLBCL).
Bispecific antibodies (BsAbs) have encouraging response rates along with a manageable safety profile in patients with relapsed/refractory diffuse large B-cell lymphoma (R/R DLBCL), according to a review of single-agent and combination trials and novel BsAb constructs published in OncoImmunology.
R/R DLBCL represents a major medical challenge, especially for patients facing poor outcomes after front-line chemoimmunotherapy. Despite advancements in treatment options, especially involving chimeric antigen receptor (CAR) T cells, roadblocks remain to effective CAR T-cell therapy delivery, the investigators discussed. These include complex insurance approval processes, high costs, long product turnaround, and limited access outside of large tertiary care centers.
The investigators aimed to provide an overview of BsAb trials for patients with R/R DLBCL, including single-agent data, results from combination trials, and an analysis of the future of treatment for these patients.
Beginning with an assessment of toxicity, the most significant adverse effects (AEs) associated with BsAb therapy in clinical trials were due to T-cell overactivation. Cytokine release syndrome was the most common, and it was observed in 15% to 80% of patients. Onset generally occurred during the initial treatment cycle, the researchers discussed.
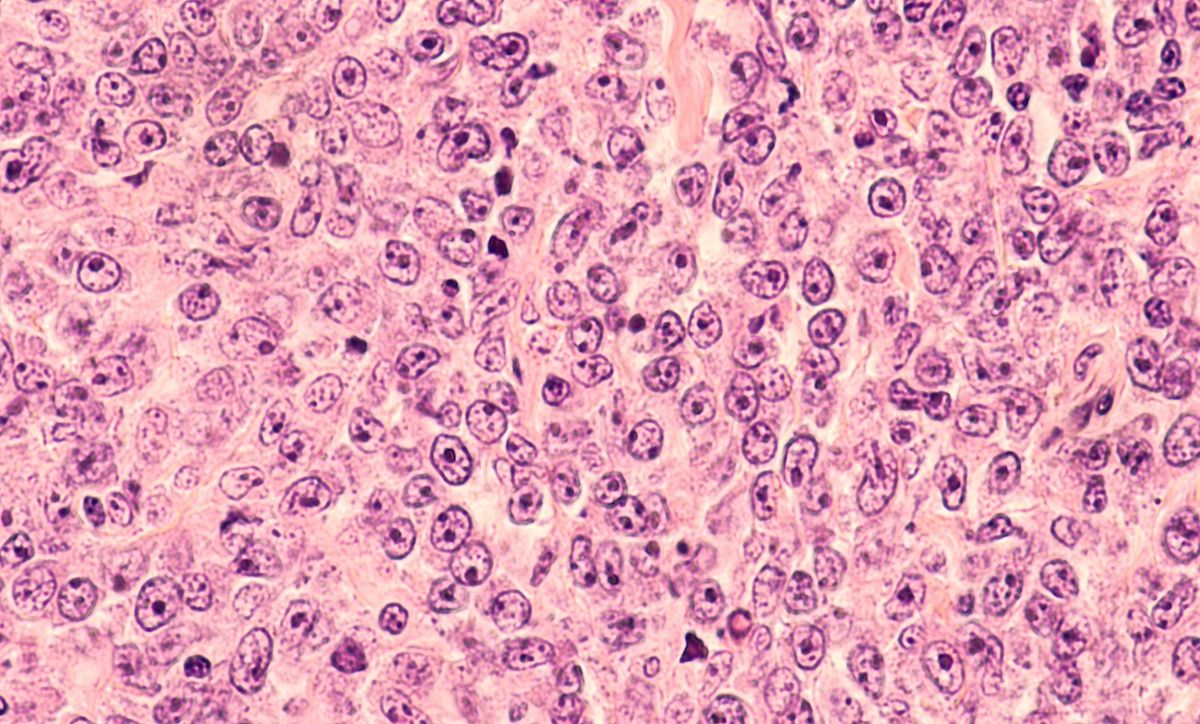
Photomicrograph of a diffuse large B-cell lymphoma | Image Credit: © DavidALitman - stock.adobe.com
Additionally, cytopenias were frequently seen following treatment with BsAbs, primarily grade 1/2 neutropenia (15%-33%) and anemia (19%-38%). The investigators noted the multifactorial pathogenesis of their development and that AEs overall were manageable and rarely led to treatment interruptions or discontinuations.
Single-agent trials investigating a series of T-cell antibodies also were examined by the investigators. Blinatumomab, a CD19 x CD3 fusion protein, had encouraging clinical results but was saddled with continuous, multiweek intravenous administration. Mosunetuzumab, an anti-CD3 x CD20 BsAb, led to an overall response rate (ORR) of 35% and a complete response (CR) rate of 19%.
Epcoritamab, a subcutaneously administered CD20 x CD3 BsAb, was studied in a phase 1/2 trial and administered using a stepped-up dosing schedule. Among the 8 patients with DLBCL treated, the ORR was 88% and the CR rate was 38%, the investigators found.
Combination trials were also of interest to the investigators, as preclinical work indicated that the coadministration of BsAbs with traditional T-cell cytotoxic agents could retain efficacy and improve survival. For example, epcoritamab was combined with dexamethasone, high-dose cytarabine, and oxaliplatin/carboplatin and led to an ORR of 100% and CR rate of 80%.
Furthermore, mosunetuzumab was combined with polatuzumab in patients with R/R DLBCL; 98 patients received mosunetuzumab, with polatuzumab administered in cycles. Of these patients, 59% had a response, and 46% had a CR, the investigators found.
Notably, T-cell activation and proliferation become amplified by additional interactions with costimulatory receptors. These observations led the investigators to analyze trials involving a variety of novel BsAb combinations that simultaneously target B-cell antigens and T-cell costimulatory receptors.
One such novel BsAb combination is RO7227166, which targets CD19 on B cells and 4-1BB on T cells and had preliminary findings among 56 patients of a 67% ORR and 39% CR rate, the investigators found.
Another antibody, RO7443904, binds CD19 and CD28 and is being combined with glofitamab in a dose-escalation trial. Preclinical models indicated that RO7443904 improved the antitumor effects of glofitamab without increasing cytokine release, according to the investigators.
Lastly, multispecific antibodies were explored, due in part to their potential to overcome resistance to and improve the activity associated with BsAbs. AZD0486, a novel anti–CD19 x CD3 BsAb that can reduce CRS by binding to T cells with low affinity, had promising initial results, the investigators wrote.
Overall, the investigators commented on the encouraging response rates and encouraging safety profile of BsAbs in the current landscape of treatment.
“Clearly, longer follow-up is needed to ascertain durability of responses and curative potential, if any, of these drugs,” the investigators concluded.
Reference
Cassanello G, Luna de Abia A & Falchi L. Trial watch: bispecific antibodies for the treatment of relapsed or refractory large B-cell lymphoma. Oncoimmunology. 2024;13(1):2321648. doi:10.1080/2162402X.2024.2321648
