- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Bispecific Antibodies for the Treatment of B-Cell Lymphomas
Introduction
Advances in cancer immunotherapy have yielded chimeric antigen receptor (CAR) T-cell and bispecific antibody (BsAb) treatments, which redirect T cells to tumor cells regardless of their T-cell receptor (TCR) specificity. Unlike monoclonal antibodies (mAbs), which target the same epitope of an antigen, BsAbs target both a tumor-associated epitope and an epitope within the TCR complex. It can take up to 8 weeks to manufacture, ship, and ensure quality control of CAR T-cell therapies; however, BsAb treatments are an off-the-shelf treatment that can be initiated promptly.1
On July 27, 2023, AJMC® hosted a roundtable, entitled, “Bispecific Antibodies for the Treatment of B-Cell Lymphomas.” The event was moderated by Matthew Matasar, MD, MS, of the Rutgers Cancer Institute of New Jersey. He was joined by Joshua Brody, MD; Lorenzo Falchi, MD; Brad Kahl, MD; Zahra Mahmoudjafari, PharmD, MBA, BCOP, FHOPA; and Mazyar Shadman, MD, MPH. Focused upon the treatment of B-cell lymphomas (BCLs), the conversation highlighted current and emerging evidence surrounding the use of BsAbs, potential benefits and limitations of these compounds compared with other available treatment modalities, operational considerations for implementation in academic settings and community-based practices, and unmet needs and future directions for the use of these agents.
Background
Several BsAb formats have been developed. These include full-length immunoglobulin G–like antibodies, bispecific T-cell engagers, dual-affinity retargeting proteins, diabodies, and immune-mobilizing monoclonal TCRs against cancer.1,2 All induce formation of an immune synapse that activates T cells to kill tumor cells.1
As of August 29, 2023, the FDA has approved 9 BsAbs, including 2 for non-oncology indications (hemophilia A and macular edema) and 7 BsAbs with indications across solid and hematologic cancers. BsAbs have received FDA approval for specific indications in the treatment of B-cell precursor acute lymphoblastic leukemia (blinatumomab), non–small cell lung cancer (amivantamab), uveal melanoma (tebentafusp), and multiple myeloma (teclistamab), with the indications for each specifying context for use in these broader disease states. The FDA has also approved mosunetuzumab, epcoritamab, and glofitamab for the treatment of lymphoma in various contexts.3
Bispecific Antibodies in the Treatment of Lymphoma
Mosunetuzumab, epcoritamab, and glofitamab all target CD20 and, within the TCR complex, CD3.1,4-6
Mosunetuzumab
In December 2022, mosunetuzumab became the first FDA-approved BsAb for the treatment of lymphoma; it is indicated for the treatment of adults with relapsed or refractory (R/R) follicular lymphoma (FL) after 2 or more lines of systemic therapy.3,4,7 The medication is given intravenously with step-up dosing in cycle 1. Patients being treated with mosunetuzumab should receive premedication with a corticosteroid, diphenhydramine, and acetaminophen before all doses in cycles 1 and 2 to reduce the risk of cytokine release syndrome (CRS) and infusion-related reactions. Mosunetuzumab carries a boxed warning for CRS.4
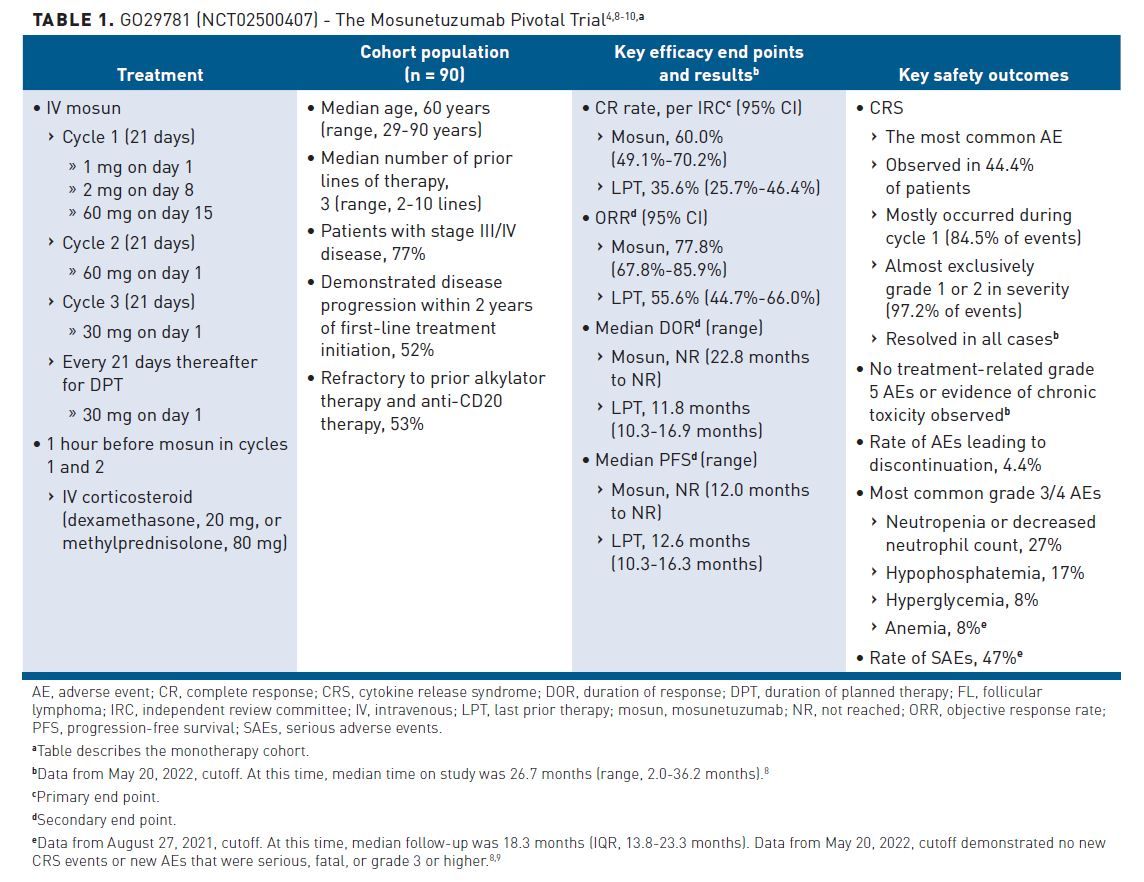
FDA approval was based on the results of the GO29781 trial (NCT02500407), which evaluated the safety and efficacy of mosunetuzumab as monotherapy and in combination with atezolizumab (Table 1).4,8-10 The open-label, multicenter, multi-cohort, phase 1/2 study enrolled patients with FL who had an ECOG performance status of 0 or 1 at baseline and who had had at least 2 prior lines of therapy including an anti-CD20 therapy and an alkylating agent. Compared with last prior therapy (LPT), monotherapy with mosunetuzumab (n = 90) was associated with improved rate of complete response (CR) as determined by an independent review committee (IRC), duration of response (DOR), progression-free survival (PFS), and objective response rate (ORR) after a median time on study of 26.7 months (range, 2.0-36.2 months). Treatment with mosunetuzumab correlated with CR rate per IRC of 60.0% (95% CI, 49.1%-70.2%), median DOR that was not reached (NR) (range, 22.8 months to NR), median PFS that was NR (range, 12.0 months to NR), and ORR of 77.8% (95% CI, 67.8%-85.9%).8-10 CRS, the most common adverse event (AE), was observed in 44.4% of patients; it mostly occurred during cycle 1 (84.5% of events), was almost exclusively grade 1 or 2 in severity (97.2% of events), and was resolved in all cases. No treatment-related grade 5 AEs or evidence of chronic toxicity was observed, and the rate of AEs leading to discontinuation was 4.4%.8
Subsequent to these results and FDA approval, the National Comprehensive Cancer Network (NCCN) updated its guidance for FL in 2023 to include a recommendation for use of mosunetuzumab in third-line and subsequent therapy. Other suggested options for third-line and subsequent treatment include second-line therapies that were not previously administered, PI3K inhibitor copanlisib, EZH2 inhibitor tazemetostat, and the CAR T-cell therapies axicabtagene ciloleucel (axi-cel) and tisagenlecleucel (tisa-cel).11 All recommendations for third-line and subsequent therapy are category 2A.
Epcoritamab
In May 2023, the FDA approved epcoritamab for the treatment of R/R diffuse large BCL, not otherwise specified (DLBCL-NOS), including DLBCL arising from indolent lymphoma, and high-grade BCL after 2 or more lines of systemic therapy.12 Epcoritamab carries a boxed warning for CRS and for immune effector cell–associated neurotoxicity syndrome (ICANS). Epcoritamab is administered as a subcutaneous injection with a step-up dosing schedule in cycle 1. Due to the paired risk of CRS and ICANS, patients should be hospitalized for 24 hours after the day 15 step-up to a 48-mg dose during cycle 1.5
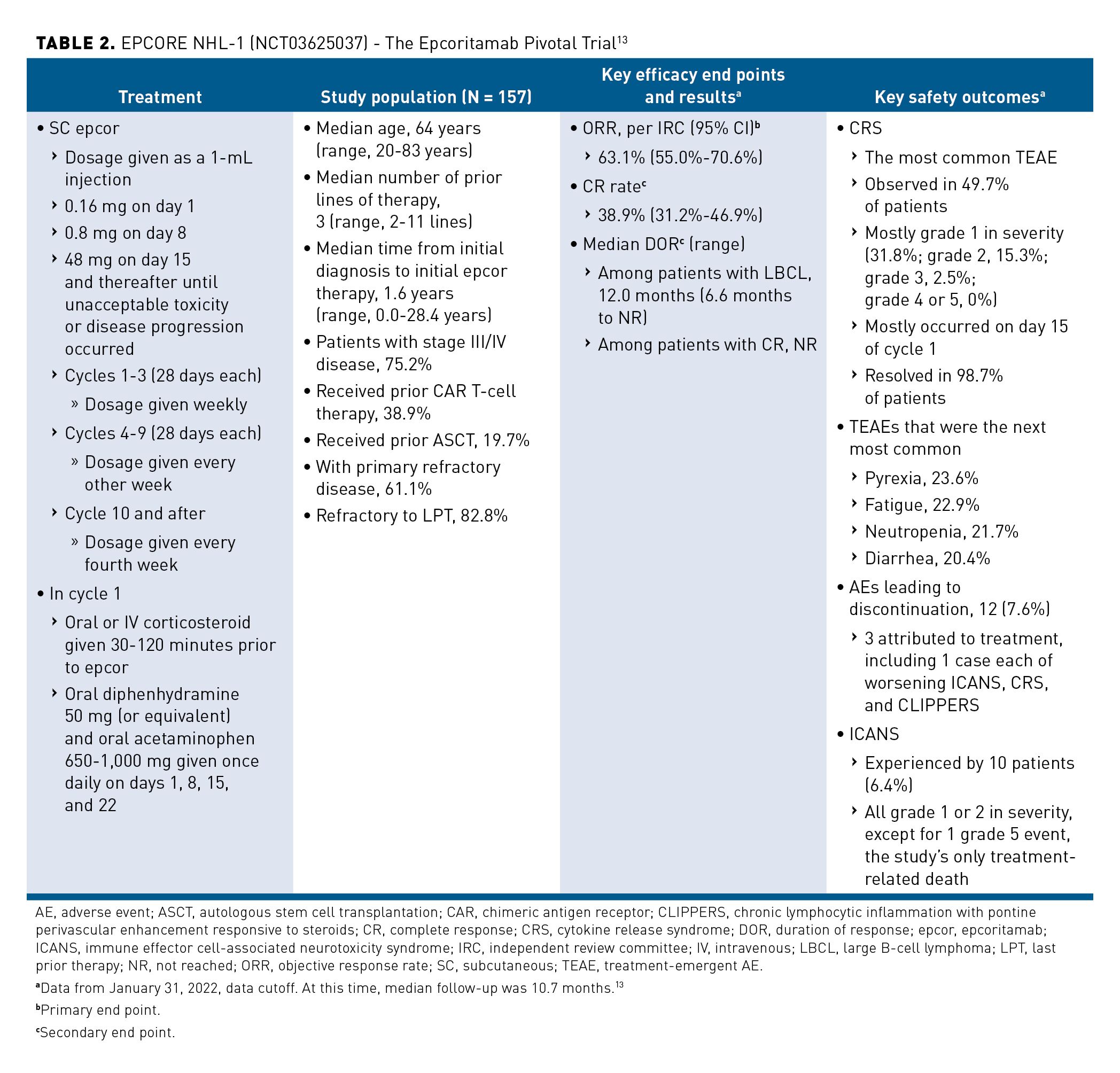
FDA approval was based upon results of the EPCORE NHL-1 trial (NCT03625037), which evaluated the safety and efficacy of epcoritamab as a monotherapy (Table 2).12,13 The open-label, multicenter, single-arm, phase 1/2 study enrolled adults with R/R CD20+ large BCL (LBCL), ECOG performance status of 0 to 2 at baseline, 2 or more prior lines of therapy including an anti-CD20 therapy, and prior failure with or ineligibility for autologous stem cell transplantation (ASCT) (N = 157). Overall, 88.5% (n = 139) of study participants had DLBCL. At median follow-up of 10.7 months, treatment with epcoritamab was associated with ORR per IRC of 63.1% (95% CI, 55.0%-70.6%), and the CR rate was 38.9% (95% CI, 31.2%-46.9%). Among patients with de novo DLBCL (n = 97), epcoritamab treatment was associated with an ORR of 60.8% (95% CI, 50.4%-70.6%) and a CRR of 46.0% (95% CI, 29.3%-61.5%). Among patients with transformed DLBCL (n = 40), epcoritamab treatment was associated with an ORR of 67.5% (95% CI, 50.9%-81.4%) and a CRR of 45.0% (95% CI, 29.3%-61.5%). The median DOR among all patients was 12.0 months (95% CI, 6.6 months to NR) and was NR among complete responders. CRS, the most common treatment-emergent AE (TEAE), was observed in 49.7% of patients and was mostly grade 1 in severity; it mostly occurred on day 15 of cycle 1, and it resolved in 98.7% of patients. ICANS was experienced by 10 patients (6.4%) and accounted for the study’s only treatment-related death.13
Glofitamab
In June 2023, the FDA approved glofitamab use after 2 or more lines of systemic therapy for treatment of R/R DLBCL-NOS or LBCL arising from FL.14 Glofitamab carries a boxed warning for CRS, is administered intravenously, and is given with step-up dosing in cycle 1. To diminish circulating and lymphoid tissue B cells, patients should be pretreated with one 1000-mg dose of obinutuzumab on day 1 of cycle 1, one week before starting glofitamab. Patients should also be pretreated with dexamethasone, acetaminophen, and an antihistamine to reduce risk of CRS and infusion-related reactions. Because of the risk of CRS, patients should be hospitalized for 24 hours after completing the step-up dose on day 8 of cycle 1.6
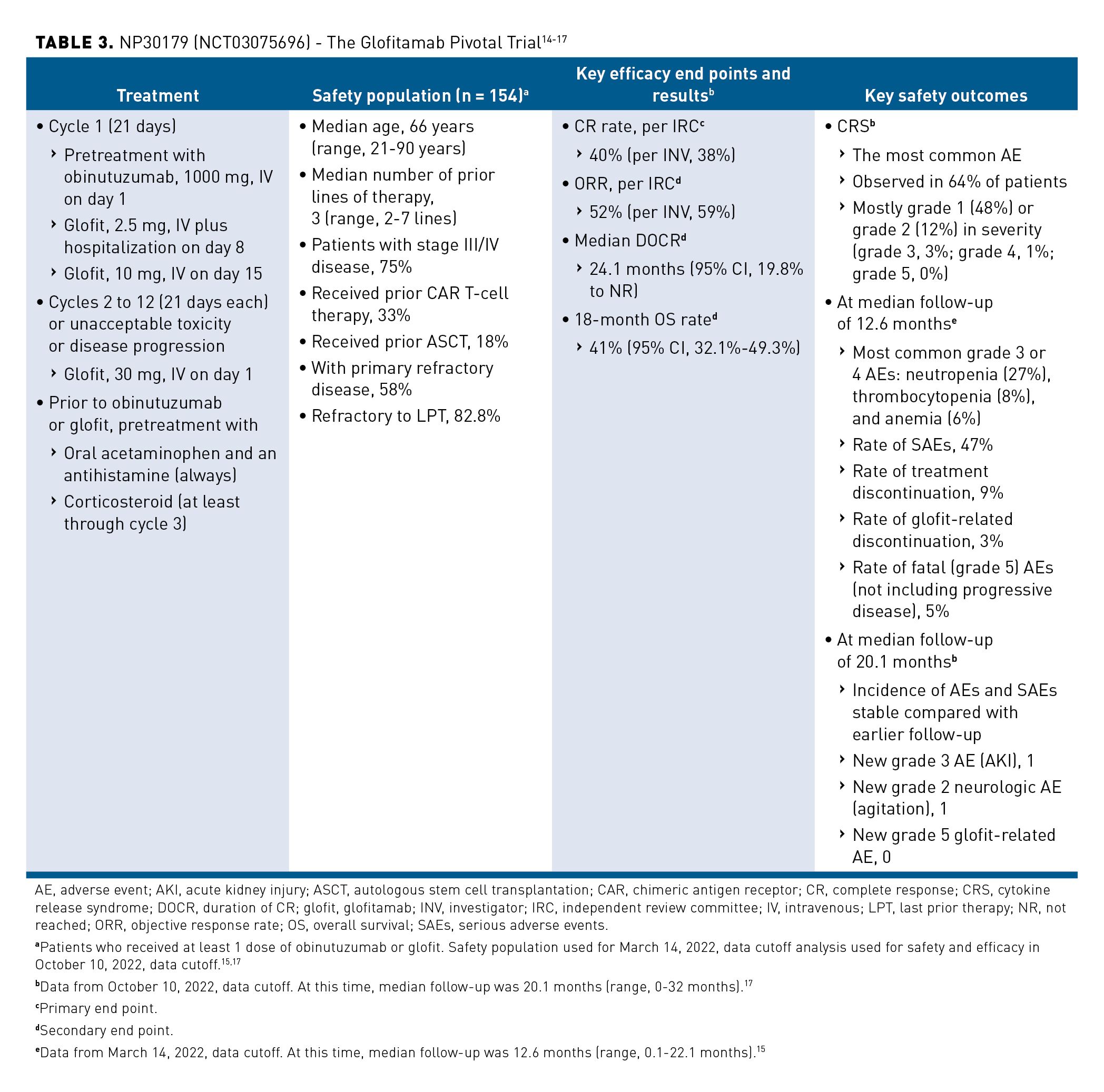
FDA approval was based on results of the NP30179 trial (NCT03075696), which evaluated the safety and efficacy of glofitamab as a monotherapy (Table 3).14-17 The open-label, multicenter, single-arm, phase 1/2 study enrolled adults with relapsed or refractory DLBCL, ECOG performance status of 0 or 1 at baseline, and 2 or more prior lines of therapy including an anti-CD20 therapy and at least 1 anthracycline-containing treatment (N = 155). At median follow-up of 20.1 months (range, 0-32 months), treatment with glofitamab was associated with CR rate per IRC of 40% (38% per investigator [INV]) and ORR per IRC of 52% (59% per INV). Median duration of CR was 24.1 months (95% CI, 19.8 months to NR) and the 18-month OS rate was 41% (95% CI, 32.1%-49.3%). CRS, the most common AE, was observed in 64% of patients and was mostly grade 1 (48%) or grade 2 (12%) in severity (grade 3, 3%; grade 4, 1%; grade 5, 0%). Incidence of AEs and SAEs remained stable compared with an earlier analysis that had a median follow-up of 12.6 months.17
Guideline Recommendations
In its Clinical Practice Guidelines for B-Cell Lymphomas, version 1.2023, the NCCN updated its guidance for FL to include mosunetuzumab. In its version 5.2023 guidance released on July 7, 2023, the NCCN also updated recommendations for DLBCL and histologic transformation of indolent lymphomas to DLBCL to reflect the approval of epcoritamab and glofitamab. For third-line and subsequent therapy for DLBCL, the NCCN recommends the use of epcoritamab and glofitamab, including use in patients with disease progression after CAR T-cell therapy or transplant. Other suggested treatment regimens include anti-CD19 CAR T-cell therapies axi-cel, tisa-cel, and lisocabtagene maraleucel (liso-cel) if not previously given, and therapies that are not T cell–mediated, including loncastuximab tesirine and selinexor. All recommendations for third-line and subsequent therapy are category 2A. For treatment of histologic transformation of indolent lymphomas to DLBCL after multiple lines of therapies, the NCCN recommends epcoritamab and glofitamab as preferred systemic therapy regimens when there is no intention to proceed to transplant. Under these circumstances, the NCCN recommends use of epcoritamab for the histologic transformation of FL or marginal zone lymphoma (MZL) (any subtype) and treatment with glofitamab for the histologic transformation of FL or nodal MZL. The NCCN also suggests anti-CD19 CAR T-cell therapy including liso-cel for the histologic transformation of FL or MZL (all subtypes), and axi-cel and tisa-cel for the histologic transformation of FL or nodal MZL.11
Operational Considerations
BsAbs are directly available off-the-shelf products. By contrast, CAR T-cell therapies, which are personalized, take 6 to 8 weeks from “vein to vein” and require bridging therapies to treat patients until the CAR T-cell product is available.1,11 However, during the roundtable, Dr Matasar argued that deployment of BsAbs involves such operational considerations as the presence or absence of risk evaluation and mitigation strategy (REMS) programs, hospitalization requirements, the management of prophylaxis to avoid toxicities, and overall coordination of care. These factors, Dr Matasar noted, can impact both implementation and cost; they must be addressed within the health care community for widespread implementation and uptake of this class of agents.
Stakeholder Insights
Dr Matasar began the roundtable by asking about the availability of BsAbs. All panelists responded that at their institutions, mosunetuzumab, epcoritamab, and glofitamab are either on the formulary or would be soon. Moreover, at most panelists’ health care centers, physicians are, or are expected to be, able to choose between epcoritamab and glofitamab for LBCL.
Clinical Availability of Bispecifics
The prescribing information (PI) for epcoritamab and glofitamab both state that patients should be hospitalized for administration of certain doses.5,6 This, noted Dr Shadman, creates logistical complexity. Staff members of his institution plan to follow the label in this regard initially, but he expects that hospital admission requirements will be relaxed as his team gains experience with these drugs.
Dr Mahmoudjafari noted that the word should has provoked conversation. It gives institutions flexibility regarding whom to admit and whom to manage in outpatient clinics provided that there are workflows in place to admit patients requiring additional support.5,6
Like Dr Shadman, Dr Kahl will begin by following the PI and probably will reduce the admission requirements over time. Members of his hospital staff are creating an outpatient cellular therapy unit and, after the unit has been operational for some time, may select patients for outpatient administration in the same way that Dr Mahmoudjafari does. Like Dr Shadman and Dr Kahl, Dr Falchi anticipated, “In the coming months, hospitalization for initial doses of BsAbs will be commonplace, and individual practitioners will tailor use of these drugs to implement them safely.” The physician confidence that such tailoring instills is important, according to Dr Falchi, especially for practitioners who have little experience with CAR T-cell or BsAb therapy in their centers.
Agent/Selection Preferences
Dr Kahl anticipated that given the results of the GO29781 trial, mosunetuzumab would soon become the preferred third-line therapy at his center. Whereas practitioners at Dr Kahl’s hospital had more familiarity with glofitamab and were likely to prefer this agent initially, those at Dr Falchi’s institution have had more experience with epcoritamab. Nevertheless, practitioners at his health care center participated in EPCORE NHL-1 and NP30179 trials. Further, nurses and inpatient physicians at his institution are familiar with both agents, which he expects will become the center’s exclusive third-line options for DLBCL.
Dr Brody noted that formulary position—rational or not—may impact the physician's decision regarding treatment. At his institution, for instance, epcoritamab is on his hospital’s outpatient formulary, and glofitamab is on the inpatient formulary.
CRS Management Strategies
Dr Matasar later asked panelists how they manage the high rates of low-grade CRS associated with BsAb treatment. Patient understanding of CRS symptoms and departure from the hospital with instructions for acetaminophen use foster CRS management, according to Drs Falchi and Kahl. Dr Kahl’s patients are encouraged to contact the on-call provider if they develop a fever, and Dr Falchi’s patients receive 2 nursing calls the next day to check symptoms.
Although the 2 experts acknowledged debate among providers regarding to what degree patients treated with BsAbs should monitor their own vital signs, Drs Falchi and Kahl underscored their comfort with such monitoring if a patient has a good thermometer, a good blood pressure machine, and a designated caregiver and demonstrates reliable measuring and reporting.
Dr Falchi treats grade 1 CRS aggressively to interrupt the self-sustaining biological process underlying CRS and gain experience with CRS escalation. Such institution-based experience, he noted, may minimize cases of grade 3 CRS. To this end, Dr Falchi’s patients treated with BsAbs go home with three 8-mg doses of dexamethasone and instructions to call a nurse for guidance on whether to self-administer with unremitting fever or fever that recurs after acetaminophen. In his experience, being able to re-dose a BsAb can give physicians confidence in using steroids in this manner. Dr Mahmoudjafari agreed. She has used steroid prophylaxis with BsAbs to decrease the incidence of CRS; such prophylaxis often is avoided with CAR T-cell therapy, she noted. Dr Kahl had not yet prescribed on-hand corticosteroids, but he endorsed the practice.
Many patients treated with mosunetuzumab in clinical trials had low-grade CRS, which manifests as a fever; however, it was a common AE related to use of COVID-19 vaccines, Dr Brody observed. Patients on mosunetuzumab who are frail or who have high comorbidity are his principal concern, and they may need to be admitted. Similarly, epcoritamab and glofitamab have both demonstrated CRS rates at about 3% grade 3, and about 97% of Dr Brody’s patients believe that hospital admission is unnecessary. He noted that outpatient platforms for these agents and trials in exclusively outpatient settings may yield data to better support treatment outside of the hospital.
Dr Brody added, “Simple algorithms for CRS may increase efficient delivery of BsAbs and facilitate management of more severe disease.” At his institution, treatment for grade 1 CRS is fluids and acetaminophen or nonsteroidal anti-inflammatory drugs; treatment for grade 2 CRS includes tocilizumab for most patients; and, for the rare cases of grade 3 CRS, treatment may include use of steroids and transfer of patients to the intensive-care unit for blood pressure monitoring and pressure support. Because many AEs occur overnight, human-to-human interaction between the primary physician and the overnight provider is important.
Dr Mahmoudjafari echoed this sentiment and added that academic centers need to partner with community providers and develop simple CRS management algorithms. The FDA does not require REMS programs for BsAbs in lymphoma as it does for CAR T-cell products, she observed, which may foster access. Dr Mahmoudjafari noted, “The work required for REMS programs has been a barrier to administration of CAR T-cell therapy in community settings.” This work can include completion of a training program by an authorized representative from a health care institution, training of relevant hospital staff, maintenance of training records, and assurance that at least 2 doses of tocilizumab are readily available for each patient; further, patients should be provided with an information card and instructed to remain within 2 hours of the institution for at least 4 weeks after CAR T-cell infusion.18,19
Partnering to Avoid Unnecessary Emergency Department Admission
Panelists were unanimous in their opinion that unnecessary trips to the emergency department (ED) for low-grade CRS should be avoided and that partnerships with other stakeholders are needed in this effort. To this end, Dr Kahl encourages patients and on-call providers against going to the ED automatically when a fever arises. He noted that most CRS can be managed in the outpatient setting and that trips to the ED can result in unnecessary testing, procedures, and admissions.
Collaborating with nursing and ED colleagues to shape care pathways is particularly useful, Dr Falchi added, especially because the oncologist becomes a consultant rather than a primary care physician after the patient is admitted. With some success, he has used an observation unit in the ED in which patients can stay for 1 or 2 nights. He noted that although prophylactic hospitalization may decrease as providers and health care systems gain experience with BsAbs, high-grade CRS events do require admission; he recommended admission for administration of indicated doses. Dr Matasar underscored the need for oncologists in academic settings to reach out to providers in the ED to ensure that they are educated about the diagnosis and management of CRS.
Digital Resources
Dr Matasar observed that the digital resources for at-home management that were developed during the height of the COVID-19 pandemic provide opportunities for the safe administration of BsAbs in the outpatient setting. Dr. Mahmoudjafari added that integrating at-home data taken with a well-functioning thermometer and a blood pressure cuff into the electronic health record (EHR) may allow remote monitoring for on-call teams. However, Dr Shadman noted that because CRS rates associated with BsAbs are low later in treatment, BsAb therapy may not require close monitoring after administration of early doses. He argued that less monitoring may facilitate therapy use in community settings and may avoid actions based on clinically irrelevant patient data.
Cost Implications of Inpatient BsAb Administration
Noting that treatments in an inpatient setting are rarely reimbursed by insurers, Dr Matasar highlighted that admitting patients for administration of BsAb LBCL treatments has cost implications for health systems. However, as BsAbs are largely administered in an outpatient setting, they are likely to save health systems money over the course of treatment, Dr Brody observed. Risk-stratifying patients, adding step-up doses, shifting BsAb therapy entirely to outpatient settings, and exploring observation periods rather than full admission may increase BsAb use in community centers and also lighten the burden on hospitals, he noted.
Dr Mahmoudjafari is also exploring alternative administration methods, and she foresees that inpatient dosing will become less frequent as more data on toxicity and step-up dosing become available. Controlled outpatient facilities like those used to administer CAR T-cell therapies may offer another option, according to Dr Shadman.
Academic and Community Partnerships
BsAb treatment can be initiated at an academic institution or a community cancer center. In Dr Shadman’s experience, “Availability of BsAbs provides an opportunity for community practitioners to use T-cell–engaging therapies that CAR T-cell therapies have not offered.” Several community providers and centers are writing their own guidelines and building an infrastructure for BsAbs. One health care network invited Dr Shadman and colleagues from his institution to discuss BsAbs, review study data, and share experiences from clinical trials. He noted that such community-based organizations are acting as centers of excellence for BsAb therapy.
Dr Shadman underscored the need for uniform and universal guidelines for colleagues working overnight and in the ED even at his institution, which has extensive experience with BsAbs.
Selection Considerations for CAR T-Cell Therapy and BsAbs in DLBCL
Dr Brody anticipated that, for the foreseeable future and across multiple disease states, a lack of sequencing trials will hinder guidance on optimal sequencing of CAR T-cell and BsAbs therapies. He noted that CAR T-cell therapy has greater precedent of potential durable remission and cure in DLBCL compared with BsAbs. However, he cited results of a recent retrospective analysis of 100% Medicare fee-for-service claims database information for 551 patients with DLBCLthat showed significantly shorter event-free survival following CAR T-cell therapy for patients 75 years and older than for patients aged 65 to 69 years and those aged 70 to 74 years.20 He then argued that this logic does not apply to all patients and that giving CAR T-cell therapy before BsAbs may be detrimental in some cases. He speculated that, in coming years, use of BsAbs will be approved for first-line therapy in combination with chemotherapy.
Dr Falchi reiterated the greater precedents of durable remission and cure for CAR T-cell therapies and added that CAR T-cell therapy is the only second-line option for patients with DLBCL. He noted that in a CAR T-cell–enabled center, he would recommend CAR T-cell therapy over use of BsAbs. However, he noted that the body of clinical trial data for use of BsAbs is growing; in the third line, physician preference and ease of access to CAR T-cell therapies will be the major determinants in treatment choice. Current limitations to the clinical utility of CAR T-cell therapy include ease of access, including the need for patients to travel long distances or relocate to receive CAR T-cell therapy, and complex insurance approval processes, he noted. Dr Falchi highlighted that BsAbs are cost-effective and can be used for up to 6 months, which may make their use more attractive. He advocated for the use of biopsies in making this decision and recommended against BsAb use for CD20– patients.
Selection Considerations for CAR T-Cell Therapy and BsAbs in FL
Dr Matasar noted that in FL, use of neither CAR T-cell therapies nor mosunetuzumab has demonstrated curative potential. He asked panelists when one treatment might be preferred over the other.
Dr Kahl highlighted the absence of relevant data but noted that in the third line, he might prefer a CAR T-cell therapy over mosunetuzumab for a younger patient with hopes for a more durable remission. Dr Brody endorsed this approach and added that he administers CAR T-cell therapy ahead of mosunetuzumab in patients who are CD20– and in patients whose disease he believes to have transformed but for whom he cannot perform a biopsy.
Dr Shadman highlighted that each of the CAR T-cell therapies approved for FL is distinct. He does not use axi-cel because of its high toxicity, but, if a younger patient seeks a 1-time therapy and a long remission, he might offer tisa-cel or liso-cel. He noted that despite the lack of long-term safety data for mosunetuzumab, this treatment is increasingly interesting to his patients.
Closing Remarks
In closing, Dr Mahmoudjafari noted that conversations among institutions and colleagues surrounding BsAbs will continue. She anticipated seeing these agents used in earlier lines of care and having more answers regarding sequencing and toxicity, especially long-term toxicity. She stated, “Bispecifics occupy a rapidly evolving space. They’re here to stay, and we must figure them out.”
Dr Falchi named BsAbs the third immunotherapy milestone for lymphoma after mAbs and CAR T-cell therapies and found them to be among the most promising single-agent treatments for DLBCL. Like Dr Mahmoudjafari, he anticipated the use of BsAbs earlier in treatment and looked forward to data from studies of their long-term efficacy and use in combination with other—especially nonchemotherapeutic—agents, including immunomodulatory agents, costimulatory molecules, mAbs, and CAR T-cell products. Dr Falchi expected new BsAbs to receive approval when used in combination therapies, rational combinations to emerge, and BsAb combination treatments to gradually replace chemotherapy.
Dr Shadman also anticipated that use of BsAbs will emerge earlier in treatment as monotherapy and in combination with different novel drugs and chemotherapy and that sequencing will be important. He highlighted the need to develop research strategies to keep pace with the number of BsAbs and possible therapeutic combinations. In Dr Shadman’s estimation, the question will be not whether to use a CAR T-cell or a bispecific agent but how to sequence or even combine these classes of agents. He stated, “The era of bispecifics is just beginning.”
Like other panelists, Dr Kahl looked ahead to new studies and opportunities for BsAbs. He predicted their movement into earlier lines of FL therapy and their increased efficacy with improved T-cell health. Noting that standard immunochemotherapy cures a large proportion of patients in large-cell lymphoma, he looked forward to participating in forthcoming trials examining immunochemotherapy given in combination with a BsAb. He concluded, “The sky’s the limit. There will be a lot of interesting bispecific investigation in the next few years.”
References
- van de Donk NWCJ, Zweegman S. T-cell-engaging bispecific antibodies in cancer. Lancet. 2023;402(10396):142-158. doi:10.1016/S0140-6736(23)00521-4
- Tian Z, Liu M, Zhang Y, Wang X. Bispecific T cell engagers: an emerging therapy for management of hematologic malignancies. J Hematol Oncol. 2021;14(1):75. doi:10.1186/s13045-021-01084-4
- Bispecific antibodies: an area of research and clinical applications. FDA. August 2, 2023. Accessed August 20, 2023. https://cacmap.fda.gov/drugs/news-events-human-drugs/bispecific-antibodies-area-research-and-clinical-applications
- Lunsumio. Prescribing information. Genentech; 2022. Accessed September 1, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/761263s000lbl.pdf
- Epkinly. Prescribing information. Genmab US; 2023. Accessed September 1, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/761324s000lbl.pdf
- Columvi. Prescribing information. Genentech; 2023. Accessed September 1, 2023. https://www.gene.com/download/pdf/columvi_prescribing.pdf
- FDA grants accelerated approval to mosunetuzumab-axgb for relapsed or refractory follicular lymphoma. FDA. December 23, 2022. Accessed August 21, 2023. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-mosunetuzumab-axgb-relapsed-or-refractory-follicular-lymphoma
- Bartlett NL, Sehn LH, Matasar MJ, et al. Mosunetuzumab monotherapy demonstrates durable efficacy with a manageable safety profile in patients with relapsed/refractory follicular lymphoma who received ≥2 prior therapies: updated results from a pivotal phase II study. Blood. 2022;140 (suppl 1): 1467-1470. doi:10.1182/blood-2022-157691
- Budde LE, Sehn LH, Matasar M, et al. Safety and efficacy of mosunetuzumab, a bispecific antibody, in patients with relapsed or refractory follicular lymphoma: a single-arm, multicentre, phase 2 study. Lancet Oncol. 2022;23(8):1055-1065. doi:10.1016/S1470-2045(22)00335-7
- A safety, efficacy and pharmacokinetic study of BTCT4465A (mosunetuzumab) as a single agent and combined with atezolizumab in non-Hodgkin’s lymphoma (NHL) and chronic lymphocytic leukemia (CLL). ClinicalTrials.gov. Updated August 14, 2023. Accessed August 20, 2023. https://classic.clinicaltrials.gov/ct2/show/NCT02500407
- NCCN. Clinical Guidelines in Oncology. B-cell lymphomas, version 5.2023. Accessed August 21, 2023. https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf
- FDA grants accelerated approval to epcoritamab-bysp for relapsed or refractory diffuse large B-cell lymphoma and high-grade B-cell lymphoma. FDA. May 19, 2023. Accessed August 21, 2023. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-grants-accelerated-approval-epcoritamab-bysp-relapsed-or-refractory-diffuse-large-b-cell
- Thieblemont C, Phillips T, Ghesquieres H, et al. Epcoritamab, a novel, subcutaneous CD3×CD20 bispecific T-cell–engaging antibody, in relapsed or refractory large B-cell lymphoma: dose expansion in a phase I/II trial. J Clin Oncol. 2023;41(12):2238-2247. doi:10.1200/JCO.22.01725
- FDA grants accelerated approval to glofitamab-gxbm for selected relapsed or refractory large B-cell lymphomas. FDA. June 16, 2023. Accessed August 21, 2023. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-grants-accelerated-approval-glofitamab-gxbm-selected-relapsed-or-refractory-large-b-cell
- Dickinson MJ, Carlo-Stella C, Morschhauser F, et al. Glofitamab for relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2022;387(24):2220-2231. doi:10.1056/NEJMoa2206913
- Protocol for: Dickinson MJ, Carlo-Stella C, Morschhauser F, et al. Glofitamab for relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2022;387:2220-2231. doi:10.1056/NEJMoa2206913 Accessed September 1, 2023. https://www.nejm.org/doi/suppl/10.1056/NEJMoa2206913/suppl_file/nejmoa2206913_protocol.pdf
- Falchi L, Carlo-Stella C, Morschhauser F, et al. Glofitamab monotherapy in pts with relapsed/refractory (R/R) large B-cell lymphoma (LBCL): extended follow-up and landmark analyses from a pivotal phase II study. J Clin Oncol. 2023;41(16_suppl):7550. 10.1200/JCO.2023.41.16_suppl.7550
- Yescarta. Prescribing information. Kite Pharma; 2022. Accessed September 1, 2023. https://www.gilead.com/-/media/files/pdfs/medicines/oncology/yescarta/yescarta-pi.pdf
- Risk evaluation and mitigation strategy (REMS). What is the Yescarta and Tecartus REMS program? Kite Pharma. April 2022. Accessed September 1, 2023. https://www.yescartatecartusrems.com/
- Chihara D, Liao L, Tkacz J, et al. Real-world evidence of CAR T-cell therapy in older patients with relapsed/refractory diffuse large B-cell lymphoma. Blood. 2023;blood.2023020197. doi:10.1182/blood.2023020197
