- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Provider and Patient Knowledge Gaps on Biosimilars: Insights From Surveys
ABSTRACT
Beyond the legal and regulatory limitations associated with biosimilar availability in the United States, the adoption of biosimilars is contingent on the willingness of health care providers (HCPs) to prescribe them and of patients to accept them. In this dynamic market, it is of paramount importance to understand the current awareness, attitudes, and preferences of a broad spectrum of stakeholders if uptake of biosimilars is to be optimized. In this article, we highlight knowledge gaps among US HCPs and patients regarding biosimilars for immune-mediated inflammatory diseases as assessed in published survey literature over the last 5 years. Although HCP familiarity and understanding of biosimilars appears to have improved over the last 5 years, survey data suggest that some physicians and pharmacists still approach use of biosimilars with caution owing to concerns regarding nonmedical switching, interchangeability, pharmacist-led substitution, and the extent of any cost savings. Patients understand the potential cost benefits of biosimilars but share many of the HCPs’ concerns. A large majority of patients were also concerned that biosimilars would not treat their disease as well as the reference product and that switching may cause more adverse effects. Consequently, nonmedical switching is a major concern for patients, with the majority reporting that they would attempt to avoid a switch. Although patients trust their physicians’ treatment recommendations and express confidence in biosimilars, they have mixed views on automatic substitution by pharmacists. The areas of concern identified can be used to guide further education programs for HCPs and patients, and, in doing so, improve biosimilar uptake.
Am J Manag Care. 2022;28:S227-S233
For author information and disclosures, see end of text.
Introduction
Biosimilars represent a cost-effective alternative to their corresponding approved reference products when acceptable quality, safety, immunogenicity, and efficacy regulatory standards are demonstrated.1-4 If out-of-pocket costs of a biosimilar are similar to or lower than those of the reference product, patient access to care may be increased, leading to earlier treatment initiation and greater therapeutic continuity over the course of a chronic disease.5-7 Thus, use of biosimilars has the potential to improve or maintain health outcomes for more patients, and the ensuing price competition may reduce costs to payers.
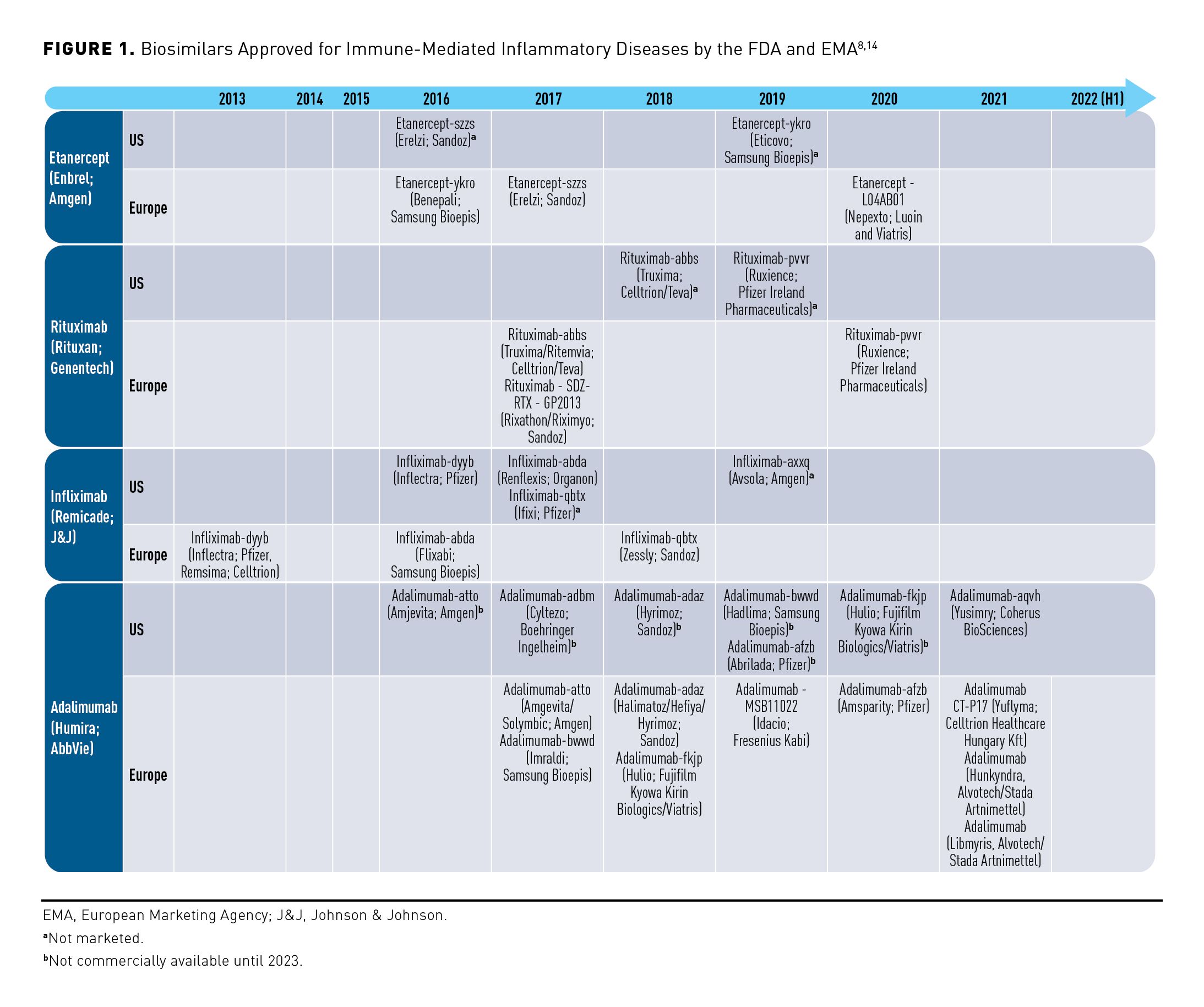
Since the US Congress created an abbreviated approval pathway for biosimilars in 2010, 37 biosimilars representing 12 molecules were approved by the FDA as of August 2022, although more than 100 biosimilars are currently in preclinical and clinical development.8-10 In all, 22 of these biosimilars are marketed in the United States, with the remainder not currently marketed for various reasons including active patent litigation or patent litigation settlements.8,11 Biosimilar adoption has been slow but growing, and, since 2019, particularly in the oncology and hematology settings.7,12 As of 2020, there has been double-digit growth in biosimilar uptake within the first 2 years of launch, but this trend is tempered by the collective market share of all biosimilars exceeding 50% for only 1 (filgrastim [Neupogen; Amgen]) of the 7 reference products with which they compete.12 As of April 2021, 3 biosimilars in the oncology setting (for reference products bevacizumab [Avastin; Genentech], trastuzumab [Herceptin; Genentech], and rituximab [Rituxan; Genentech]) were projected to attain nearly 60% share of volume for their respective molecules by the end of their second year on the market, which was a substantially higher and faster uptake than that of most other biosimilars.9 In contrast, the biosimilar landscape in Europe flourished from inception, with at least 64 biosimilars approved, marketed, and prescribed.13 Figure 1 provides a snapshot of the US and European Union (EU) biosimilar markets as they pertain to agents for immune-mediated inflammatory diseases.8,14
In the United States, improved patient access to biosimilars and encouraging forward-looking projections regarding biosimilar uptake across multiple therapeutic areas were forestalled by the COVID-19 pandemic. In 2020, US approvals for biosimilars declined, likely due to the altered business practices of many biopharmaceutical businesses and regulatory action delays (eg, international site inspections) related to the urgent regulatory reviews for pharmaceuticals related to the COVID-19 pandemic.12
Beyond the legal and regulatory limitations associated with biosimilar availability in the US, the adoption of biosimilars is contingent on the willingness of health care providers (HCPs) to prescribe biosimilars and of patients to accept them. One systematic review of surveys revealed that both US and European HCPs had a lack of overall familiarity and understanding toward biosimilars, engendering concerns about safety and efficacy that resulted in limited biosimilar prescribing.15 Another systematic review examining physicians’ perceptions of the uptake of biosimilars revealed that whereas their knowledge of and attitudes toward biosimilars were generally positive, their prescribing was limited, especially for patients already exposed to biologics.16 Furthermore, there was skepticism among physicians regarding pharmacist-led substitution of biologic medicines.16 Important limitations of these systematic reviews include the small number of studies evaluated, analyses based on data published before 2017 (when many biosimilars had not yet been approved in the United States), and the lack of involvement of subspecialists who are likely to have more experience regarding the use of biosimilars.15 The latter limitation is underscored by clinical practices at Kaiser Permanente and the US Department of Veterans Affairs, which have integrated routine use of biosimilars successfully.17,18 At Kaiser Permanente, this was achieved through collaborative policy development between all stakeholders that fosters prescriber confidence in the formulary, access to unbiased educational material, and autonomous shared-care decision-making free from financial constraints.17
In this dynamic market, it is of paramount importance to understand the current awareness, attitudes, and preferences of a broad spectrum of stakeholders toward biosimilars if uptake of these medicines is to be optimized throughout the United States. In this article, we highlight knowledge gaps among US HCPs and patients regarding biosimilars for immune-mediated inflammatory diseases as assessed in published survey literature over the past 5 years.
Issues Identified From Health Care Providers
The overall familiarity and understanding of HCPs toward biosimilars have improved over the last 5 years, although some key uncertainties remain (see eAppendix Table 1 [eAppendices available at ajmc.com]). Since an early survey conducted between November 2015 and January 2016,19 physicians and pharmacists now appear to comprehend the FDA definition of a biosimilar; the weight of evidence suggests that they appreciate biosimilars to be equally safe and efficacious alternatives to approved reference products.11,20-22 Nevertheless, survey data suggest that some physicians and pharmacists still approach use of biosimilars with caution because of concerns regarding nonmedical switching, interchangeability, pharmacist-led substitution, and extent of cost savings.
Nonmedical Switching
Nonmedical switching with biologics occurs when patients change medicines from an approved reference product to its biosimilar (or vice versa) for reasons not related to clinical need.23-25 Nonmedical reasons for switching may include treatment cost or availability and typically relate to insurance formulary coverage.25
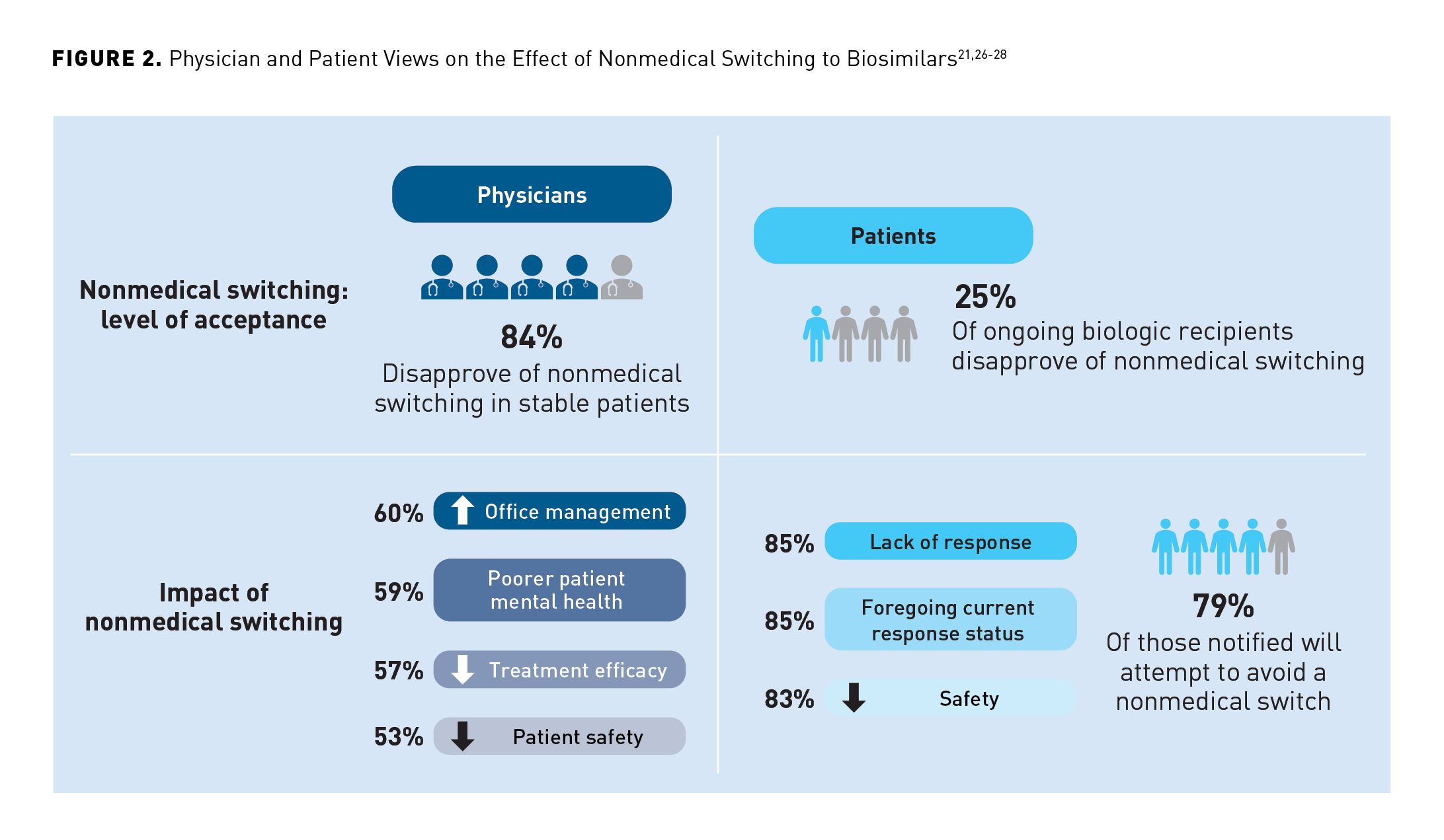
In a survey of US physicians published in 2019, over 80% expressed concerns regarding nonmedical switching to biosimilars and the impact such switching would have on patient care and physician practice (Figure 2).21,26-28 In a 2019 survey of 320 US rheumatologists who prescribed tumor necrosis factor-α inhibitors, a higher proportion of respondents stated that they were more likely to initiate biosimilar treatment for a biologic treatment–naive patient with rheumatoid arthritis than they were to switch to the biosimilar for a patient with rheumatoid arthritis doing well on the reference product (73% vs 35%).21 Likewise, in a 2020 survey of 602 specialists who regularly prescribed biologic medications to their patients, physicians were more likely to prescribe a biosimilar to patients who were newly starting therapy than to patients who were already successfully established on a reference product.11 Given that biosimilar switching is often resisted by physicians when dealing with patients already stabilized on a biologic therapy, it is not surprising that this sentiment was expressed with respect to nonmedical switching in an online survey published in 2019, with 84% of physicians expressing concern about this practice.26
Nonmedical switching to approved generic (ie, nonbiologic) medicines readily occurs without prescriber knowledge via communications between patients and their insurers.29 Once the initial switch has occurred, a process for more switching is triggered, which cascades into a complex multiple-switching default setting. To regain some control over patient circumstance, most recommendations from professional societies support switching only if it is deemed suitable by the treating physician.24,30-32 Insurer-mandated nonmedical switching is generally opposed by the American College of Rheumatology; they acknowledge that although it may be a reasonable cost-saving exercise for patients with stable disease, it cannot be justified for patients with tenuous disease control.31 The American Medical Association encourages use of sunset clauses in insurance coverage so that patients and HCPs can be prepared for the change, recommending that when a medication is removed from the formulary after the beneficiary enrollment period is over, it should be covered for the duration of the benefit year.33 Other best practices aimed at preserving concordant relationships between treating physician, pharmacist, and patient include HCPs forewarning patients that nonmedical switching may occur without prescriber knowledge and incumbency on the dispensing pharmacist to inform the prescriber if a nonmedical switch is set to occur. There are national survey data to suggest that formulary status of the biologic agents supersedes a patient’s previous experience with a product when it comes to prescriber choice.34 Thus, robust formulary development by local pharmaceutical and therapeutics committees should engender HCPs with confidence in the biosimilar deployed by unavoidable nonmedical switching.
Interchangeability
The term “interchangeability” refers to the practice of changing 1 medicine for another to achieve the same clinical effect in each patient.35 An interchangeable biologic is a biosimilar that produces the same clinical outcome as the reference product in any given patient. For a biosimilar to obtain regulatory designation as an interchangeable biosimilar, additional evidence may include switching studies to demonstrate that efficacy and safety is maintained when a patient switches between the reference biologic and the biosimilar.36,37
Although the FDA has approved 37 biosimilars, it has granted an interchangeable designation (which requires a second FDA review of additional interchangeable studies) to very few.38,39 Notably, many biosimilar manufacturers have chosen not to seek an interchangeable designation; possibly, they have been deterred by the additional cost of these interchangeable studies. To date, only 3 biosimilars have been given interchangeable status. The first, Semglee (insulin glargine-yfgn; Viatris), was awarded in July 2021 as an interchangeable for insulin glargine (Lantus, sanofi-aventis U.S.). Insulin was only included as a biologic eligible for biosimilar status in March 2021. When insulins were moved under the biologic regulations, the FDA guidance stated that switching studies may not be necessary to achieve interchangeable designation. Subsequently, Cyltezo (adalimumab-adbm; Boehringer Ingelheim) was also granted interchangeable status with Humira (adalimumab; AbbVie) in October 2021.40 Most recently, Cimerli (ranibizumab-eqrn; Coherus BioSciences) was granted interchangeable status with Lucentis (ranibizumab; Genentech) in August 2022.8 The interchangeable designation permits substitution of the reference product with its biosimilar at the pharmacy without physician consent in accordance with state law.12 The analogous situation occurs with the dispensing of small-molecule medicines when generics are freely interchanged with the reference products after quality issues (eg, bioequivalence testing) have been satisfied. It is up to each state to make and enact policies on automatic biosimilar substitution at the pharmacy level.41 At present, there is a lack of interstate harmonization of regulatory standards for automatic substitution.41 On April 22, 2021, Oklahoma became the final state to enact a law regarding substitution of interchangeables at the pharmacy level once FDA-approved. Notably, the majority of state laws include a requirement to notify the HCP when such a substitution is made.41,42
Survey data published from 2017 to 2021 indicate a lack of clarity on interchangeability among HCPs (eAppendix Table 1). In a 2019 survey, most responding rheumatologists (84%) stated that they were aware that an approved biosimilar was not automatically deemed interchangeable by the FDA.21 However, only 20% of pharmacists knew that FDA approval as “interchangeable” meant that the biosimilar could be substituted without contacting the prescriber.22 Furthermore, only 11% of surveyed pharmacists knew that, at that time, none of the existing biosimilars had been designated as interchangeable.22
Clearly, the lack of interchangeable biosimilars in the United States represented a major barrier to the uptake of these agents. This problem is being addressed directly with clinical studies designed to evaluate whether outcomes in a switching arm are similar to those in the reference arm with respect to pharmacokinetics, efficacy, immunogenicity, and safety.43
An example of demonstrated biosimilar interchangeability is the VOLTAIRE clinical trial program, encompassing head-to-head comparisons of adalimumab-adbm and its reference product adalimumab, which received an interchangeable designation in October 2021. In the VOLTAIRE-PK study (NCT02045979) of healthy subjects, 3-way bioequivalence of adalimumab-adbm to US- and EU-approved adalimumab was demonstrated, and the safety and immunogenicity results of the 3 study drugs were highly comparable.44 In the rheumatoid arthritis setting of VOLTAIRE-RA (NCT02137226) and VOLTAIRE-RAext (NCT02640612), adalimumab-adbm demonstrated similar efficacy, safety, and immunogenicity to adalimumab, and switching from adalimumab to adalimumab-adbm had no impact on efficacy, safety, and immunogenicity.45,46 Adalimumab-adbm demonstrated equivalent efficacy and immunogenicity and comparable safety to adalimumab in patients with chronic plaque psoriasis participating in the randomized phase 3 VOLTAIRE-PSO study (NCT02850965).47 The interchangeability of adalimumab-adbm and adalimumab in patients with moderate to severe chronic plaque psoriasis was then demonstrated in the phase 3 VOLTAIRE-X trial (NCT03210259).48 VOLTAIRE-X data showed that switching several times between adalimumab-adbm and adalimumab reference product resulted in equivalent pharmacokinetics, efficacy, immunogenicity, and comparable safety in people with moderate to severe chronic plaque psoriasis. At week 32, the study met the primary end point, supporting the application of adalimumab-adbm as an interchangeable biosimilar for the adalimumab reference product. Moreover, an earlier systematic review of data from several switching studies showed no changes in efficacy, safety, trough serum drug concentration, or immunogenicity between other adalimumab biosimilars and the adalimumab reference product.1
Once the interchangeability of a biosimilar has been demonstrated, the FDA advises that Biologics License Application holders include a labeling statement on interchangeability placed immediately beneath the initial US approval portion of the prescribing information section of the product label. The published evidence base showing biosimilar interchangeability together with the associated FDA product labeling statement will ease formulary decision-making.
Pharmacist-led Substitution
Pharmacist-led substitution refers to dispensing of 1 medicine instead of another generic (nonbiologic) medicine or interchangeable biosimilar without consulting the prescriber.49 For small-molecule medicines, pharmacist-led substitution is generally allowed for drugs that have demonstrated pharmacokinetic bioequivalence to the branded reference medicine and that are listed as equivalent; exceptions can be made if the prescriber indicates “dispense as written” (or “DAW”) on the prescription. Even then, substituting an ongoing treatment is not advised without a concordant shared-care arrangement when the drug has a low therapeutic index or when the patient has multiple or severe morbidities. State laws permit pharmacists to substitute an interchangeable biosimilar for the reference product without prior knowledge of the HCP everywhere except for Alabama, Indiana, South Carolina, and Washington State, although some states include restrictions on when this is permissible that relate to treatment cost. However, at present, pharmacists cannot substitute a biosimilar for a reference product in most cases, because interchangeability has not been established, with only 3 biosimilars approved as interchangeable at this time. Indeed, in a 2020 survey of 602 physicians, 75% were largely opposed to automatic substitution of biologics by pharmacists.11 Physicians expressing this hesitancy may be concerned about both losing involvement with patients’ treatment and dealing with the higher level of complexity associated with biosimilars.
Making a substitution of a biosimilar product at the pharmacy level comes with challenges, and clear local and national biosimilar substitution laws, as well as management strategies, are needed.50 As they did during the advent of generic medicines, pharmacists will play a key role in raising awareness of biosimilars and interchangeable biosimilars among prescribers and patients and minimizing skepticism about biosimilar quality, safety, and efficacy.
Price Effects and Cost Savings
Biologics account for 37% ($120 billion) of all US drug costs but only 2% of all prescriptions written; since 2014, they also account for 93% of the overall growth in total spending.51 Biosimilars are intended to provide affordable treatment options for patients and cost savings for payers, theoretically lowering the systemic financial burden as lower-cost versions of the reference product; in turn, the cost of the reference product is driven down by competitive pressure. Realistically, for each therapeutic intervention, more than 1 biosimilar for each reference product is needed to lower costs. With so few biosimilars currently marketed in the United States, there is a lack of motivation for prescribers to switch to a biosimilar when the cost savings are not justified.
Data from a national online survey conducted from 2019 to 2020 and involving 507 US dermatologists, gastroenterologists, hematologists, oncologists, nephrologists, and rheumatologists indicated that most prescribers will choose the approved reference product over the biosimilar when both agents are on the formulary.34 A difference in formulary status between the 2 agents as well as financial incentives are needed to affect willingness to prescribe the biosimilar.33 These findings have major ramifications, given that US health plans covered biosimilars as preferred in only 14% of decisions in 2019.52 In addition, at present, savings realized by the payer have not been shown to directly benefit the patient, and the results of several studies suggest that this lack of financial incentive is impeding biosimilar uptake.52-55 Indeed, in the absence of strong financial incentives, there is a tendency for prescribers to obtain a prior authorization to receive the nonformulary approved reference product for patients currently treated with it, despite the additional administrative burden.34
In a 2020 survey, two-thirds of physicians stated that they would be more likely to prescribe biosimilars if they knew that they would reduce patient out-of-pocket costs.11 However, whereas physicians believe that biosimilar out-of-pocket costs are lower than those associated with the approved reference product, they remain concerned that drug discount programs may mitigate differences in patient costs.11 In a survey of rheumatologists published in 2020, there was a reluctance in switching from reference products to biosimilars, partly because of insufficient cost savings.56 Most biosimilars on the market today are priced at only a 15% to 40% discount of the reference product list price, and two-thirds of surveyed rheumatologists indicated that those pharmacoeconomics were not favorable enough to motivate them to switch.56
Not surprisingly, physicians seek greater transparency about prices for approved reference biologics and biosimilars.11 If physicians could see seamless direct cost savings for the patient, they would be encouraged toward greater prescribing.11,34 Rather, the extent to which physicians are burdened with a range of administrative tasks when attempting to prescribe biosimilars (eg, requirements for prior authorization, appreciation of drug discount programs) renders the potential cost savings unrewarding. In an online survey of patients in 2020, 56% reported that they went without therapy for administrative reasons during the period of transition from the approved reference product to the biosimilar.11 Physicians are likely aware of these temporary treatment interruptions only anecdotally from some of their patients, and, thus, may avoid future switching if cost savings are marginal.
Issues Identified From Patients
Patients understand the potential cost benefits but share many of the concerns HCPs have regarding biosimilars (eAppendix Table 2).11,27,57 A caveat to this pertains to efficacy and safety; this raises uncertainties for patients.27,57 A large majority of patients (85%) in a survey published in 2019 were concerned that biosimilars would not treat their disease as well as a reference treatment would, 85% did not want to switch to a biosimilar if their current biologic was working, and 83% were concerned that switching may cause more adverse effects (Figure 2).21,26-28 Consequently, nonmedical switching is a major concern for patients. In a survey published in 2019, 79% of patients indicated that they attempt to avoid the switch; in another survey published in 2021, 43% of patients reported accepting the switch.27,57
Although patients trust their physicians’ treatment recommendations and express confidence in biosimilars, they have mixed views on automatic substitution by pharmacists.11 Among patients surveyed in 2020, 71% expressed full confidence in a biosimilar prescribed by a physician, but 23% stated that they would accept the switch but feel worried.11
Clearly, there is a role for HCPs in addressing patients’ concerns by providing greater information on biosimilars. Nearly all patients in a 2020 survey had confidence in the FDA approval process assuring biosimilar quality, safety, and efficacy, which is a critical communication point in discussions between HCPs and their patients.11 Nonmedical switching is a vexing issue for patients, likely because of disempowerment, especially when identifying the correct treatment has been a long and difficult process. This can be addressed by encouraging shared-care decision-making with HCPs, which educates and empowers patients, making them active participants in their care.
Conclusions
The increasing use of biosimilars will have a positive effect on the availability of biologics and health care costs. As more biosimilars are approved and marketed, the transition of eligible patients from approved reference products will pose challenges that can be overcome by informed HCPs and patients. The issues raised in surveys on biosimilars focused on nonmedical switching, interchangeability, pharmacist-led substitution, and delivery of cost savings. Presently, biosimilars have not reduced inconvenience for physicians prescribing biologics, and there is prescriber and patient unease regarding nonmedical switching and pharmacist-led substitution. These areas of concern can be used to guide further education programs for HCPs and patients, and, in doing so, improve biosimilar uptake. In the meantime, it is important to champion best practices that assist with biosimilar integration into the formulary building process.
Acknowledgments
The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors (ICMJE). The authors received no direct compensation related to the development of the manuscript. Writing, editorial support, and formatting assistance was provided by Andy Shepherd, PhD, CMPP; and Malcom Darkes of Elevate Scientific Solutions, which was contracted and funded by Boehringer Ingelheim Pharmaceuticals, Inc. (BIPI). BIPI was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Data sharing
Data sharing is not applicable to this article, as no new data were created or analyzed in this report.
Author Affiliations: Weill Cornell Medicine and Hospital for Special Surgery (AG), New York, NY; National Psoriasis Foundation (former/retired; CE), Austin, TX; Division of Immunology & Rheumatology, Department of Medicine, Stanford University (VS), Palo Alto, CA.
Author ORCID iD: Vibeke Strand, MD (https://orcid.org/0000-0003-4978-4072).
Funding Source: This supplement was supported by Boehringer Ingelheim Pharmaceuticals, Inc.
Author Disclosures: Dr Gibofsky reports serving as a consultant/advisor to AbbVie, Biosplice Therapeutics, Lilly, Novartis, and Pfizer; he reports being on the speakers’ bureau for AbbVie, Amgen, and Pfizer; and he reports owning stock in AbbVie, Amgen, Bristol Myers Squibb, and Pfizer. Dr Evans reports serving as a volunteer board member for the National Psoriasis Foundation and serving as a consultant or paid advisory board member for Celgene. He has received honoraria from Celgene and Cigna, and he reports being on the speakers’ bureau for AbbVie and Celgene. Dr Strand reports serving as a consultant/advisor for AbbVie, Amgen, Arena Pharmaceuticals, Aria Pharmaceuticals, AstraZeneca, Bayer, Bristol Myers Squibb, Bioventus, Boehringer Ingelheim, Celltrion, ChemoCentryx, EMD Serono, Endo, Equillium, Galapagos, Genentech/Roche, Gilead Sciences, GSK, Horizon, Ichnos Sciences, Inmedix, Janssen, Kiniksa Pharmaceuticals, Kypha, Lilly, Merck, MiMedx, Novartis, Pfizer, Regeneron, Rheos Medicines, R-Pharm US, Samsung, Sandoz, Sanofi, Scipher Medicine, Servier Pharmaceuticals, SetPoint Medical, Sorrento Therapeutics, Sun Pharma, and UCB.
Authorship Information: Analysis and interpretation of data (AG, CE, VS); drafting of the manuscript (AG, CE, VS); critical revision of the manuscript for important intellectual content (AG, CE, VS).
Address correspondence to: Allan Gibofsky, MD, JD. Email: GibofskyA@hss.edu
References
1. Huizinga TWJ, Torii Y, Muniz R. Adalimumab biosimilars in the treatment of rheumatoid arthritis: a systematic review of the evidence for biosimilarity. Rheumatol Ther. 2021;8(1):41-61. doi:10.1007/s40744-020-00259-8
2. Cohen HP, Blauvelt A, Rifkin RM, Danese S, Gokhale SB, Woollett G. Switching reference medicines to biosimilars: a systematic literature review of clinical outcomes. Drugs. 2018;78(4):463-478. doi:10.1007/s40265-018-0881-y
3. Tanaka E, Kawahito Y, Kohno M, et al. Systematic review and meta-analysis of biosimilar for the treatment of rheumatoid arthritis informing the 2020 update of the Japan College of Rheumatology clinical practice guidelines for the management of rheumatoid arthritis. Mod Rheumatol. 2021:1-13. doi:10.1080/14397595.2021.189959
4. Scientific considerations in demonstrating biosimilarity to a reference product. Guidance for industry. FDA. April 2015. Accessed June 26, 2021. https://www.fda.gov/media/82647/download
5. The impact of biosimilar competition in Europe. IQVIA. October 2019. Accessed August 5, 2022.
https://ec.europa.eu/docsroom/documents/38461/attachments/1/translations/en/renditions/pdf
6. Olech E. Biosimilars: Rationale and current regulatory landscape. Semin Arthritis Rheum. 2016;45(suppl 5):S1-10. doi:10.1016/j.semarthrit.2016.01.001
7. Biosimilars 101: practice concerns, market acceptance, and the biosimilars pipeline. Center for Biosimilars. August 2, 2022. Accessed September 15, 2022. https://www.centerforbiosimilars.com/resources?display=recent
8. Biosimilar approval status in the US: FDA filing dates and actions. BR&R Biosimilars Review and Report. 2022. Accessed August 5, 2022. https://biosimilarsrr.com/us-biosimilar-filings/
9. Biosimilars in the United States 2020–2024, Competition, savings, and sustainability. Institute report. IQVIA. September 29, 2020. Accessed August 5, 2022. https://www.iqvia.com/insights/the-iqvia-institute/reports/biosimilars-in-the-united-states-2020-2024
10. Rader RA. Biosimilars pipeline shows remarkable, sustained growth. Biosimilar Development. March 7, 2019. Accessed August 5, 2022. https://www.biosimilardevelopment.com/doc/biosimilars-pipeline-shows-remarkable-sustained-growth-0001
11. Wilde S, Schapiro L, Fletcher M, Pearson C. Understanding stakeholder perception of biosimilars. NORC. April 2021. Accessed August 5, 2022. https://www.norc.org/PDFs/Biosimilars/20210405_AV%20-%20NORC%20Biosimilars%20Final%20Report.pdf
12. 2020 Biosimilar trends report. Amgen Biosimilars. September 2020. Accessed August 5, 2022.
https://www.amgenbiosimilars.com/-/media/Themes/Amgen/amgenbiosimilars-com/Amgenbiosimilars-com/pdf/USA-CBU-80723-2020-Amgen-Biosimilar-Trends-Report.pdf
13. Feldman M, Reilly MS. A white paper: US biosimilars market on pace with Europe. Generics Biosimilars Initiative J. 2020;9(4):150-154. doi:10.5639/gabij.2020.0904.025
14. Biosimilars approved in Europe. Generics and Biosimilars Initiative. July 2022. Accessed August 5, 2022. https://www.gabionline.net/biosimilars/general/biosimilars-approved-in-europe
15. Leonard E, Wascovich M, Oskouei S, Gurz P, Carpenter D. Factors affecting health care provider knowledge and acceptance of biosimilar medicines: a systematic review. J Manag Care Spec Pharm. 2019;25(1):102-112. doi:10.18553/jmcp.2019.25.1.102
16. Sarnola K, Merikoski M, Jyrkka J, Hameen-Anttila K. Physicians’ perceptions of the uptake of biosimilars: a systematic review. BMJ Open. 2020;10(5):e034183. doi:10.1136/bmjopen-2019-034183
17. Biosimilars at Kaiser Permanente. Institute for Health Policy. December 2020. Accessed August 5, 2022. https://www.kpihp.org/wp-content/uploads/2020/12/Biosimilars_at_KP_121420_FINAL.pdf
18. Generic and biosimilar disease modifying therapies. US Department of Veterans Affairs. Multiple Sclerosis Centers of Excellence. August 2021. Accessed August 5, 2022. https://www.va.gov/MS/Veterans/medications/Generic_and_Biosimilar_Disease_Modifying_Therapies.asp
19. Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33(12):2160-2172. doi:10.1007/s12325-016-0431-5
20. Greene L, Singh RM, Carden MJ, Pardo CO, Lichtenstein GR. Strategies for overcoming barriers to adopting biosimilars and achieving goals of the Biologics Price Competition and Innovation Act: a survey of managed care and specialty pharmacy professionals. J Manag Care Spec Pharm. 2019;25(8):904-912.
21. Gibofsky A, McCabe D. US rheumatologists’ beliefs and knowledge about biosimilars: a survey. Rheumatology (Oxford). 2021;60(2):896-901. doi:10.1093/rheumatology/keaa502
22. Stevenson JG, McCabe D, McGrath M, McBride A. A survey to assess pharmacists’ knowledge and understanding of biosimilars and interchangeability. J Manag Care Spec Pharm. 2021;27(suppl 10b):S97. Abstract U7. https://www.jmcp.org/doi/epdf/10.18553/jmcp.2021.27.issue-10-b#:~:text=U7,age%20restrictiveness
23. Feagan BG, Marabani M, Wu JJ, Faccin F, Spronk C, Castaneda-Hernandez G. The challenges of switching therapies in an evolving multiple biosimilars landscape: a narrative review of current evidence. Adv Ther. 2020;37(11):4491-4518. doi:10.1007/s12325-020-01472-1
24. McKinnon RA, Cook M, Liauw W, et al. Biosimilarity and interchangeability: principles and evidence: a systematic review. BioDrugs. 2018;32(1):27-52. doi:10.1007/s40259-017-0256-z
25. Weeda ER, Nguyen E, Martin S, et al. The impact of nonmedical switching among ambulatory patients: an updated systematic literature review. J Mark Access Health Policy. 2019;7(1):1678563. doi:10.1080/20016689.2019.1678563
26. Teeple A, Ellis LA, Huff L, et al. Physician attitudes about nonmedical switching to biosimilars: results from an online physician survey in the United States. Curr Med Res Opin. 2019;35(4):611-617. doi:10.1080/03007995.2019.1571296
27. Teeple A, Ginsburg S, Howard L, et al. Patient attitudes about non-medical switching to biosimilars: results from an online patient survey in the United States. Curr Med Res Opin. 2019;35(4):603-609.
doi:10.1080/03007995.2018.1560221
28. Coleman C, Salam T, Duhig A, et al. Impact of non-medical switching of prescription medications on health outcomes: an e-survey of high-volume medicare and medicaid physician providers. J Mark Access Health Policy. 2020;8(1):1829883. doi:10.1080/20016689.2020.1829883
29. Salam T, Duhig A, Patel AA, et al. Communication of medication nonmedical switching policies and procedures by insurance companies: results of an e-survey. Clin Ther. 2020;42(6):1077-1086. doi:10.1016/j.clinthera.2020.04.007
30. Position paper on generic therapeutic & biosimilar substitution. American Academy of Dermatology. Amended August 3, 2013. Accessed August 5, 2022. https://www.aad.org/Forms/Policies/Uploads/PS/PS-Generic%20Therapeutic%20and%20%20Biosimilar%20Substitution.pdf
31. Position statement: biosimilars. American College of Rheumatology. 2016. Accessed August 5, 2022. https://www.rheumatology.org/portals/0/files/biosimilars-position-statement.pdf
32. Drug formularies and therapeutic interchange H-125.991. American Medical Association. Modified 2020. Accessed August 5, 2022. https://policysearch.ama-assn.org/policyfinder/detail/Drug%20Formularies%20and%20Therapeutic%20Interchange%20H-125.991?uri=%2FAMADoc%2FHOD.xml-0-227.xml
33. Prior authorization and utilization management reform principles. American Medical Association. 2017. Accessed August 5, 2022. https://www.ama-assn.org/sites/default/files/media-browser/principles-with-signatory-page-for-slsc.pdf
34. Kolbe AR, Kearsley A, Merchant L, et al. Physician understanding and willingness to prescribe biosimilars: findings from a US national survey. BioDrugs. 2021;35(3):363-372. doi:10.1007/s40259-021-00479-6
35. Ebbers HC, Schellekens H. Are we ready to close the discussion on the interchangeability of biosimilars? Drug Discov Today. 2019;24(10):1963-1967. doi:10.1016/j.drudis.2019.06.016
36. Ebbers HC, Muenzberg M, Schellekens H. The safety of switching between therapeutic proteins. Expert Opin Biol Ther. 2012;12(11):1473-1485. doi:10.1517/14712598.2012.711308
37. Ebbers HC, Crow SA, Vulto AG, Schellekens H. Interchangeability, immunogenicity and biosimilars. Nat Biotechnol. 2012;30(12):1186-1190. doi:10.1038/nbt.2438
38. Considerations in demonstrating interchangeability with a reference product. Guidance for industry. FDA. May 2019. Accessed August 5, 2022. https://www.fda.gov/media/124907/download
39. Epstein M. Food and Drug Administration guidances on biosimilars: an update for the gastroenterologist. Therap Adv Gastroenterol. 2018;11:1756284818799600. doi:10.1177/1756284818799600
40. FDA approves Cyltezo, the first interchangeable biosimilar to Humira. FDA. October 18, 2021. Accessed August 5, 2022. https://www.fda.gov/news-events/press-announcements/fda-approves-cyltezo-first-interchangeable-biosimilar-humira
41. Cauchi R. State laws and legislation related to biologic medications and substitution of biosimilars, July 2015—covering 2013-2015 legislative sessions. National Conference of State Legislature. May 3, 2019. August 5, 2022. https://www.ncsl.org/research/health/state-laws-and-legislation-related-to-biologic-medications-and-substitution-of-biosimilars.aspx
42. State laws for biosimilar interchangeability. CardinalHealth. Updated July 2021. Accessed August 5, 2022. https://www.cardinalhealth.com/en/product-solutions/pharmaceutical-products/biosimilars/state-regulations-for-biosimilar.html
43. Alvarez DF, Wolbink G, Cronenberger C, Orazem J, Kay J. Interchangeability of biosimilars: what level of clinical evidence is needed to support the interchangeability designation in the United States? BioDrugs. 2020;34(6):723-732. doi:10.1007/s40259-020-00446-7
44. Wynne C, Altendorfer M, Sonderegger I, et al. Bioequivalence, safety and immunogenicity of BI 695501, an adalimumab biosimilar candidate, compared with the reference biologic in a randomized, double-blind, active comparator phase I clinical study (VOLTAIRE-PK) in healthy subjects. Expert Opin Investig Drugs. 2016;25(12):1361-1370. doi:10.1080/13543784.2016.1255724
45. Cohen SB, Alonso-Ruiz A, Klimiuk PA, et al. Similar efficacy, safety and immunogenicity of adalimumab biosimilar BI 695501 and Humira reference product in patients with moderately to severely active rheumatoid arthritis: results from the phase III randomised VOLTAIRE-RA equivalence study. Ann Rheum Dis. 2018;77(6):914-921. doi:10.1136/annrheumdis-2017-212245
46. Cohen SB, Czeloth N, Lee E, Klimiuk PA, Peter N, Jayadeva G. Long-term safety, efficacy, and immunogenicity of adalimumab biosimilar BI 695501 and adalimumab reference product in patients with moderately-to-severely active rheumatoid arthritis: results from a phase 3b extension study (VOLTAIRE-RAext). Expert Opin Biol Ther. 2019;19(10):1097-1105. doi:10.1080/14712598.2019.1645114
47. Menter A, Arenberger P, Balser S, et al. Similar efficacy, safety, and immunogenicity of the biosimilar BI 695501 and adalimumab reference product in patients with moderate-to-severe chronic plaque psoriasis: results from the randomized Phase III VOLTAIRE-PSO study. Expert Opin Biol Ther. 2021;21(1):87-96. doi:10.1080/14712598.2021.1851362
48. Menter A, Cohen S, Kay J, et al. Switching between adalimumab reference product and BI 695501 in patients with chronic plaque psoriasis (VOLTAIRE-X): a randomized controlled trial. Am J Clin Dermatol. 2022;23(5):719-728. doi: 10.1007/s40257-022-00708-w
49. Declerck P, Endrenyi L, Chow SC. Chapter 10: Interchangeability, switchability and substitution of biosimilar products. In: Endrenyi LDPJ, Declerck P, Chow SC. Biosimilar Drug Product Development. CRC Press/Taylor & Francis; 2017; 283-296.
50. Milmo S. Biosimilars: making the switch comes with challenges. BioPharm International. 2016;29(6):10-14. Accessed June 6, 2022. https://www.biopharminternational.com/view/biosimilars-making-switch-comes-challenges
51. Lexchin J. Affordable biologics for all. JAMA Netw Open. 2020;3(4):e204753. doi:10.1001/jamanetworkopen.2020.4753
52. Chambers JD, Lai RC, Margaretos NM, Panzer AD, Cohen JT, Neumann PJ. Coverage for biosimilars vs reference products among US commercial health plans. JAMA. 2020;323(19):1972-1973. doi:10.1001/jama.2020.2229
53. Baker JF, Leonard CE, Lo Re V 3rd, Weisman MH, George MD, Kay J. Biosimilar uptake in academic and veterans health administration settings: influence of institutional incentives. Arthritis Rheumatol. 2020;72(7):1067-1071. doi:10.1002/art.41277
54. Karaca-Mandic P, Chang J, Go R, Schondelmeyer S, Weisdorf D, Jeffery MM. Biosimilar filgrastim uptake and costs among commercially insured, Medicare Advantage. Health Aff (Millwood). 2019;38(11):1887-1892. doi:10.1377/hlthaff.2019.00253
55. Yazdany J, Dudley RA, Lin GA, Chen R, Tseng CW. Out-of-pocket costs for infliximab and its biosimilar for rheumatoid arthritis under Medicare Part D. JAMA. 2018;320(9):931-933. doi:10.1001/jama.2018.7316
56. Loria K. Survey: rheumatologists still reluctant to switch patients to biosimilars. Managed Healthcare Executive®. July 2, 2020. Accessed August 5, 2022. https://www.managedhealthcareexecutive.com/view/survey-rheumatologist-still-reluctant-to-switch-patients-to-biosimilars
57. Gibofsky A, Jacobson G, Franklin A, et al. Attitudes about biosimilars among US patients with rheumatoid arthritis, psoriasis, psoriatic arthritis, or inflammatory bowel disease: an online survey. J Manag Care Spec Pharm. 2021;27(suppl 10b):S107. Abstract Z10. https://www.jmcp.org/doi/epdf/10.18553/jmcp.2021.27.issue-10-b#:~:text=Z10,Ingelheim%20Pharmaceuticals%20Inc