- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Biosimilar HLX01 Demonstrates Bioequivalence With Rituxan in DLBCL
A new study has found that HLX01 (HanliKang), a rituximab biosimilar, had comparable overall survival and progression-free survival rates to the reference product (Rituxan) in patients with diffuse large B-cell lymphoma (DLBCL).
This article originally appeared on The Center for Biosimilars®.
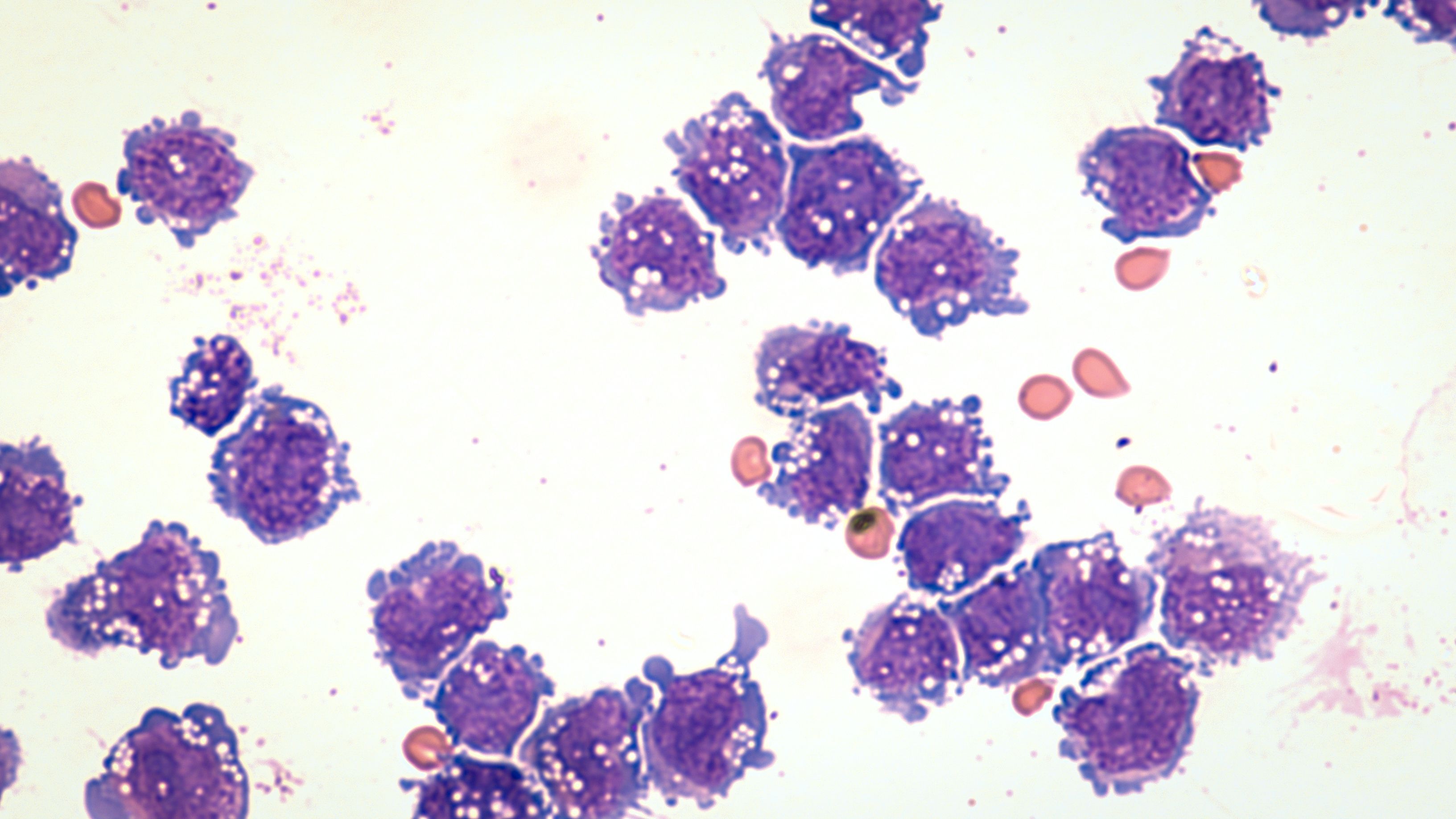
Microscopic image of DLBCL
Image credit: DavidALitman - stock.adobe.com
A phase 3, randomized, double-blind study conducted in China found bioequivalence between reference rituximab (Rituxna) and HLX01 (HanliKang), a rituximab biosimilar, for overall survival (OS) and progression-free survival (PFS) in patients with diffuse large B-cell lymphoma (DLBCL).
Findings were published recently in BioMed Central Cancer.
Rituximab is a monoclonal antibody used to treat DLBCL, as well as other aggressive cancers. HLX01 was developed in line with China's National Medical Products Administration (NMPA) and the World Health Organization. On February 22, 2019, the NMPA approved HLX01 as the first biosimilar in China.
China’s standard care in the first-line setting for patients with DLBCL is the combination of rituximab with cyclophosphamide, doxorubicin, vincristine (Oncovin), and prednisone (R-CHOP). The researchers randomized patients to receive either R-CHOP intravenously or HLX01 combined with cyclophosphamide, doxorubicin, vincristine, and prednisone (H-CHOP) as doses of 375 mg/m2 once every 3 weeks for up to 6 weeks.
Data from 27 hospitals across China were used to enroll 316 patients in the study, with the researchers using April 28, 2022, as the cut-off date (R-CHOP, n = 159; H-CHOP, n = 157). The 6 planned treatment cycles were completed by 91.8% of the R-CHOP cohort and 87.3% of the H-CHOP group. The median age of patients was 56.1 years, with the median duration of follow-up as 65.1 months. OS and PFS values were recorded at the 1-, 3-, and 5-year marks.
The International Prognostic Index (IPI) had 96.5% of patients in IPI 1 and 2, 47.2% had clinical stage III/IV disease, and 17.7% had bone marrow involvement. The study found no significant differences in efficacy or OS between the treatment groups. The 5-year OS rates were 75.4% and 81%, for R-CHOP and H-CHOP, respectively; for patients completing all 6 cycles, the 5-year OS rates were 77.6% and 83.3%. A similar number of patients died in both groups (R-CHOP, n = 41; H-CHOP, n = 31).
There were no statistically significant differences in PFS between the R-CHOP and H-CHOP treatment groups 5 years after completing all 6 cycles (75.6% vs 79.6%, respectively).
For patients with low-risk DLBCL (IPI score 1 or 2), the R-CHOP and H-CHOP groups, respectively, had similar 5-year OS rates (IPI 1, 80.2% vs 86.8%; IPI 2, 68% vs 76.2%) and PFS rates (IPI 1, 75.3% vs 84.1%; IPI 2, 68.2% vs 72%).
Patients with an IPI score of 1 had better outcomes than those with a score of 2 (OS, 83.1% vs 72.3%; PFS, 79.3% vs 70.2%). No significant differences were observed in OS or PFS between clinical stages I/II and III/IV (OS, 79.4% vs 76%; PFS, 79% vs 70.4%).
Limitations of the study included the likeliness of nonresponse bias with telephone follow-up and the absence of visual cues that compromise the data representation.
Study results were comparable with previous long-term follow-up studies administering rituximab with chemotherapy in patients with DLBCL.
The authors concluded, “HLX01 is an appropriate substitute for rituximab that can provide comparable efficacy in patients with low- or low-intermediate IPI risk DLBCL.”
Reference
Qin Y, Song Y, Wang D, et al. Long-term outcomes with HLX01 (HanliKang), a rituximab biosimilar, in previously untreated patients with diffuse large B-cell lymphoma: 5-year follow-up results of the phase 3 HLX01-NHL03 study. BMC Cancer. 2024;24(1):124. doi:10.1186/s12885-024-11876-9
