- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Biosimilar Follitropin Alfa Offers Fertility Savings in France
A French study found that follitropin alfa, a biosimilar fertility drug, is more cost-effective compared with its originator, leading to potential savings for both patients and the health care system.
A French study found that follitropin alfa, a biosimilar fertility drug, is more cost-effective compared with itsoriginator, leading to potential savings for both patients and the healthcare system. | Image Credit: cristianstorto - stock.adobe.com
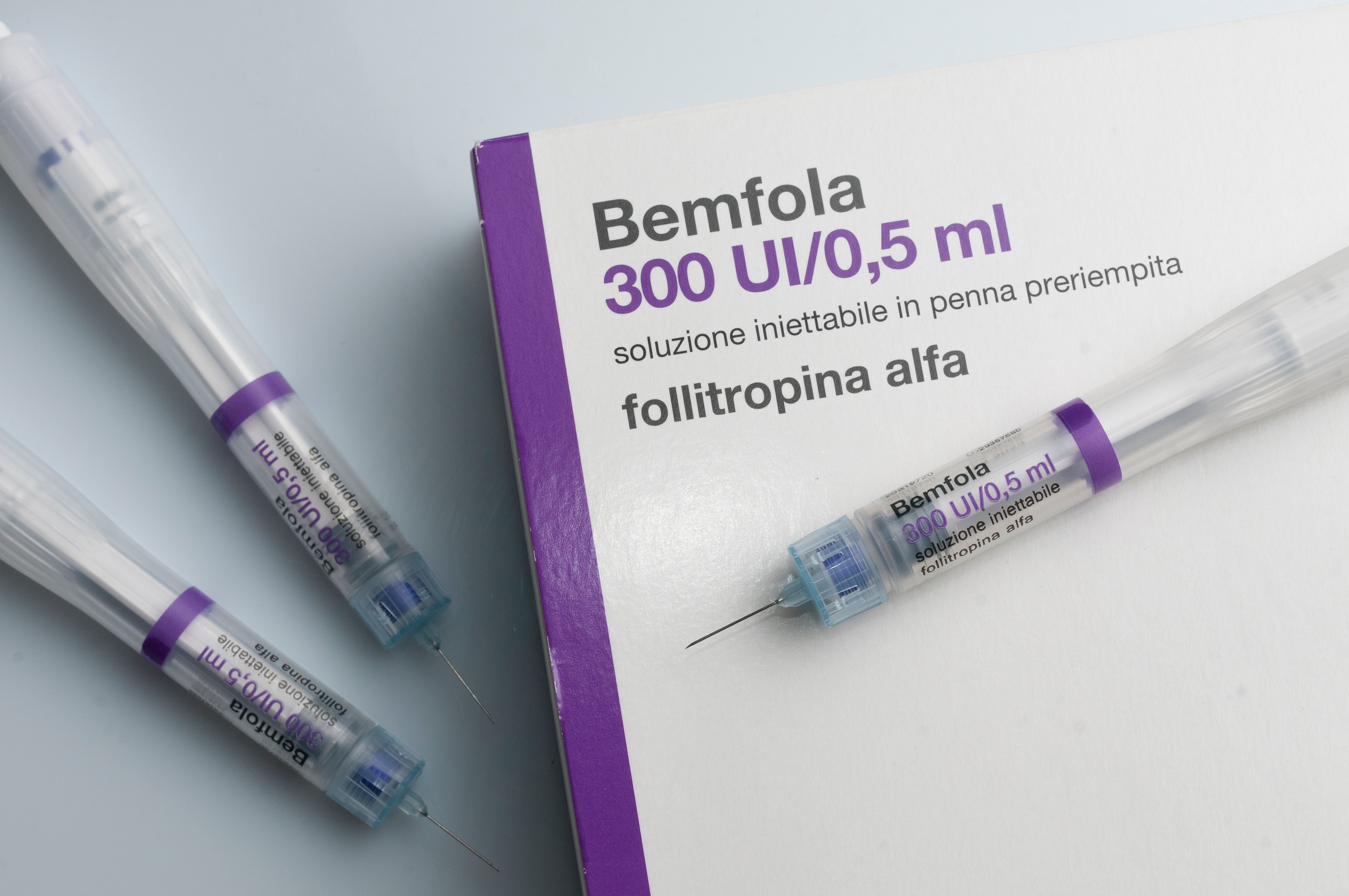
The follitropin alfa biosimilar (Bemfola) was more cost-effective compared with the originator in ovarian stimulation based on the cost per cumulative live-birth rates (CLBRs) from a French health care payer perspective, according to a new analysis published in the European Journal of Obstetrics & Gynecology and Reproductive Biology.1
Infertility, typically associated with social stigma and high treatment costs, affects an estimated 1 in 6 people globally. Assisted reproductive technologies (ARTs) is a popular option for women who are struggling to become pregnant. The CDC defines ARTs as procedures that surgically remove the eggs from a woman’s ovaries and combine them with sperm in the laboratory before returning the fertilized embryo to the woman’s body or donating it to another woman.2
Although ART procedures have demonstrated effectiveness, the act of follicle-stimulating hormones creates significant cost burdens for patients.1 The French health care system has suggested biosimilars as a solution to initiate savings benefits. France introduced the follitropin alfa biosimilar in 2015 as the first recombinant human follicle stimulating hormone (r-hFSH).
“The study aimed to perform a cost-effectiveness analysis of follitropin alfa biosimilar vs the originator in women undergoing IVF [in vitro fertilization]/ICSI [intracytoplasmic sperm injection]treatment based on real-world evidence from a French health care perspective in terms of cost per CLB,” wrote the research authors.
The study design was a decision-tree cost-effectiveness model, focused on the total costs and CLBR for each ovarian stimulation for a follitropin alfa biosimilar and its originator. The model utilized clinical data from the REOLA study, a retrospective, real-world study that used anonymous management systems across France.3 Additionally, the study model applied a consistent time horizon from one year after oocyte retrieval to embryo transfer, either fresh or frozen, including the time until live birth as a result from the transfers.1
Total costs per CLB were €18,147 ($20,200) with the follitropin alfa biosimilar and €18,834 ($20,965) with the originator. This saved €687 ($764) per CLB after ovarian stimulation with the biosimilar. The stimulation phase represented the greatest difference between the originator and the biosimilar for the average woman. The follitropin alfa biosimilar also was 9.1% cheaper compared with the originator, representing reduced drug costs.
Biosimilar cost savings were between €796 ($886) and €1155 ($1285) per CLB when estimated to include drug wastage. This outcome only further increased the overall total cost savings. If the REOLA study treated every woman with follitropin alfa biosimilar (N = 6606),the resultant savings could be €4,538,322 ($5,051,833), equivalent to 250 CLBs. When this method is applied to the entirety of France, biosimilars could save the health system €13,994,190 ($15,577,632) or lead to 771 more births compared with higher-cost originators.
The originators are sold as multidose, multiuse pens whereas the biosimilars are chosen by the physician based on the appropriate follitropin alfa biosimilar pen size for the patient’s daily r-hFSH need to reduce waste. Switching to follitropin alfa biosimilar has the potential to save the French health care system money due to decreased drug costs and less wastage.
Study limitations included the use of assumptions to fill knowledge gaps, which risks bias, an essential measurement to the research model. Despite this, the model displayed more cost-effective options with the biosimilars for ovarian stimulation in France compared with the originator based on costs per CLB.
“This is the first health economic study utilizing real world data and CLBR, enabling a more representative analysis of the cost-effectiveness of infertility treatments utilized in French clinical practice,” concluded the study authors.
References
- Lehmann M, Arbo E, Pouly JL, et al. Determining the cost-effectiveness of follitropin alfa biosimilar compared to follitropin alfa originator in women undergoing fertility treatment in France. Eur J ObstetGynecolReprod Biol X. 2024;22:100311. doi:10.1016/j.eurox.2024.100311
- What is assisted reproductive technology? CDC. October 8, 2019. Accessed September 30, 2024. https://www.cdc.gov/art/whatis.html
- Barrière P, Samir Hamamah, Arbo E, et al. A real-world study of ART in France (REOLA) comparing a biosimilar rFSH against the originator according to rFSH starting dose. J GynecolObstetHum Reprod 2023;52(1):102510-102510. doi:10.1016/j.jogoh.2022.102510
The Breakdown: Breast Cancer Research Awareness Day
August 19th 2025Breast cancer is the second most common cancer among women and the second leading cause of cancer-related deaths among women in the US. In light of Breast Cancer Research Awareness Day, The American Journal of Managed Care® breaks down the most recent advancements in breast cancer prevention, screening, and therapies.
Listen
