- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Beyond Skin Deep: Biologic Breakthroughs and a Shift Toward Precision Care in Plaque Psoriasis
Introduction
Psoriasis, a chronic immune-mediated disorder affecting the skin, is a global health concern affecting an estimated 125 million people worldwide.1 In the United States, approximately 7.6 million adults (age, ≥ 20 years), constituting approximately 3.0% (95% CI, 2.6%-3.4%) of adults, are affected by this condition.2 Among the various clinical presentations of psoriasis, plaque psoriasis is the most prevalent, accounting for around 80% to 90% of all psoriasis cases.1
Plaque psoriasis is characterized by the formation of distinct erythematous scaly patches with clear boundaries.1 The disease results from dysregulation of the innate and adaptive immune systems and involves both the skin epithelium and connective tissue; thus, plaque psoriasis is considered an autoimmune-type inflammatory disease.3
Plaque psoriasis greatly affects the overall quality of life (QOL) of patients, particularly when lesions occur on the palms, soles, face, or other areas that are visible or susceptible to physical contact during daily activities.1 Moreover, psoriasis occurs as a comorbidity in approximately 32% of patients with metabolic syndrome (MetS) globally.4 Despite this frequent association, comprehensive guidelines for selecting appropriate treatments for individuals with both plaque psoriasis and MetS remain limited.5
In recent years, the treatment landscape for plaque psoriasis has transformed with the emergence of biologic agents, which has created new avenues for disease management. Numerous biologic therapies have been approved by the FDA and European Medical Agency (EMA) for treating moderate to severe psoriasis. These biologic agents include TNF-α inhibitors, IL-12/-17 inhibitors, IL-17 inhibitors, and IL-23 inhibitors, with each targeting specific components of the immune response cascade implicated in the pathogenesis of plaque psoriasis.6
Selecting appropriate strategies is important when treating patients with plaque psoriasis. Clinicians must account for the complex interplay between the disease and its associated comorbidities. In particular, when selecting treatments for patients with MetS, clinicians must consider the potential impact on disease severity and treatment response.7 The response to and tolerability of a given medication can also influence treatment adherence and the likelihood of therapy switching by patients.8
Consideration of these factors from an economic perspective is particularly important for formulary decision makers, who evaluate treatment costs and real-world utilization patterns to balance the clinical benefits, safety, and financial implications of a therapy. Assessing health care costs associated with various treatment options can provide insight to guide formulary decision-making.8
Efficacy and Safety Profiles of Biologic Agents
A comprehensive understanding of the efficacy and safety profiles of biologic agents is important to optimize patient outcomes in psoriasis management.
Efficacy
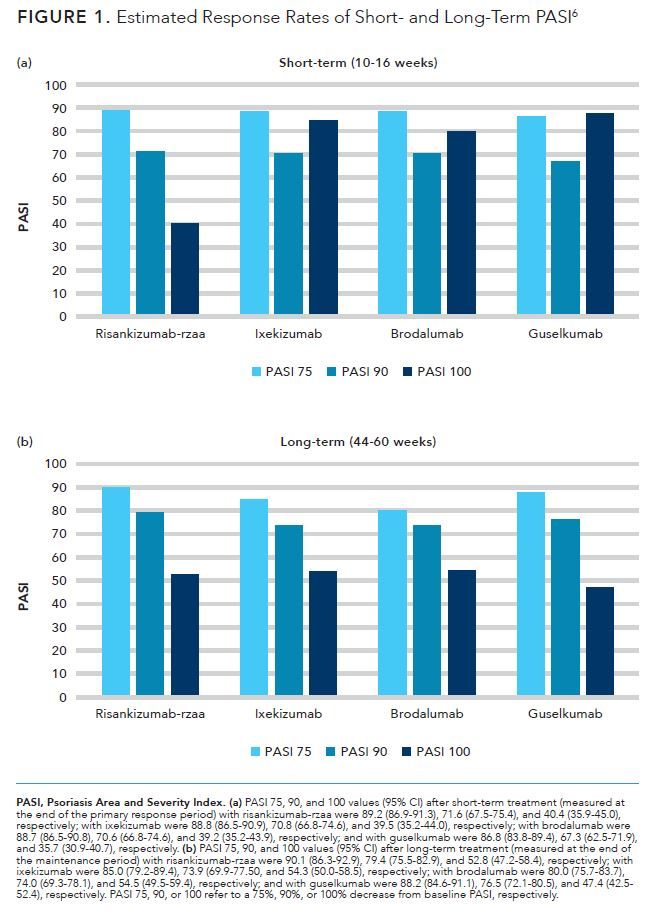
According to results of a meta-analysis of the short- and long-term efficacy of biologic agents involving use of IL-17 inhibitors (brodalumab, ixekizumab) and IL-23 inhibitors (guselkumab, risankizumab-rzaa), the highest Psoriasis Area and Severity Index (PASI) response rates were noted from 10 to 16 weeks and from 44 to 60 weeks of administration compared with baseline PASI levels.6 The authors identified and reviewed randomized clinical trials of FDA- and EMA-approved treatments for adult patients with moderate to severe plaque psoriasis published through September 17, 2018 (Figure 1).6
As described in a review by Kim and colleagues in 2019, the majority of patients in clinical trials reached a 75% decrease in PASI score when using most currently available biologics.9 More than one-third of patients treated with available biologics, excluding those who received etanercept, experienced a 90% decrease in their PASI scores
(PASI 90) compared with baseline levels.9
Safety
Biologics approved for treating plaque psoriasis are associated with increased risks of hypersensitivity reactions and infection (including tuberculosis).7 For example, TNF-α inhibitors carry boxed warnings—the highest level of caution used by the FDA—for serious infection, lymphoma, and other malignancies.7 IL-17 inhibitors have been associated with an increased risk of mucocutaneous Candida infection and exacerbation of inflammatory bowel disease.7 Although use of IL-12/-23 inhibitors does not increase the rates of serious infection or malignancies compared with placebo, these treatments have led to slightly increased rates of upper respiratory tract infections and headache.1 Unlike treatment with other classes of biologics, use of IL-23 inhibitors is very safe and results in risks of adverse events (AEs) similar to those of placebo.7
According to a meta-analysis, use of tildrakizumab, certolizumab, etanercept, risankizumab, and guselkumab resulted in the lowest rates of AEs.10 In this benefit-risk assessment, the authors compared the risk of any AE versus achievement of a PASI 90 (short-term analysis) and found that use of risankizumab or guselkumab had comparably low rates of AEs and comparably high rates of PASI 90.10
Factors Influencing Treatment Selection – Comorbidities and Safety Considerations
The impact of safety on treatment selection for moderate to severe psoriasis has been examined. The results of a phase 1 study showed that tildrakizumab use was well tolerated and that it significantly improved psoriasis symptoms.11 These effects were maintained according to results of phase 2b (NCT01225731)12 and phase 3 (reSURFACE 1 [NCT01722331] and reSURFACE 2 [NCT01729754]) trials.13 In a narrative review, 14 experts provided opinions on these results and concluded that tildrakizumab therapy resulted in a good safety profile when used in both theshort- and long-terms.14 Further, in terms of special populations, the experts considered use of tildrakizumab to be safe in women of childbearing potential (if use of IL-23 inhibitors was stopped as soon as pregnancy was detected), elderly patients, and those with psoriatic arthritis, inflammatory bowel disease, cardiovascular disease, or metabolic syndrome.14
Obesity influences the efficacy of therapies for psoriasis. In clinical trials, treatment responses were diminished in patients with a body weight of more than 100 kg, who comprise approximately 25% to 30% of participants. However, notable enhancements in the effectiveness of biologics were documented in individuals who were obese but who achieved weight loss reduction through dietary control.9
In a post-hoc analysis, 5-year data from the reSURFACE 1 and reSURFACE 2 multinational, double-blind, randomized, placebo-controlled phase 3 trials were analyzed to evaluate the efficacy and safety of tildrakizumab in patients who achieved at least 50% reductions in PASI scores.15 Results from the reSURFACE 1 trial involved 1) continuous use of 100 mg of tildrakizumab in 20 patients with MetS and 72 patients without MetS or 2) continuous use of 200 mg of tildrakizumab in 31 patients MetS and 83 patients without MetS. Likewise, results from the reSURFACE 2 trial involved 1) continuous use of 100 mg of tildrakizumab in 36 patients with MetS and 130 patients without MetS and 2) continuous use of 200 mg tildrakizumab in 22 patients with MetS and 130 patients without MetS. Patients were evaluated for up to 244 weeks of treatment.15 Safety analysis from 5 years of analysis showed that the safety profile was mostly consistent with that of tildrakizumab; common treatment-related AEs included serious infections/infestations and malignancies. The risks of AEs were similar between patients with and without MetS.15
Other comorbid conditions also influence the choice of treatment. Inhibitors of TNF-α and IL-17 have shown the strongest efficacy in patients with psoriatic arthritis. The results of 2 trials (PSUMMIT-1 [NCT01009086]16 and PSUMMIT-2 [NCT01077362]17) showed that 45 and 90 mg of ustekinumab were both effective in curbing joint damage progression in patients with active psoriatic arthritis, although not to the same extent as that seen with use of TNF blockers. In an extension study of 40 mg of ixekizumab given every 2 or 4 weeks, joint damage progression was minimal, showing results similar to those for adalimumab.9 Further, some biologics (eg, IL-12/23 and IL-23 inhibitors) are associated with increased risks of certain types of cancer in patients with specific gene mutations or polymorphisms.18 Patients with psoriasis may have an increased susceptibility to multiple sclerosis (MS) due to an excessively active immune system; individuals with MS or those with first-degree relatives affected by MS are advised against taking TNF-α inhibitors.19
Patient-Centric Approach to Treatment Selection
Shared Decision-Making
Shared decision-making is an important aspect of psoriasis treatment. A cross-sectional, population-based study was conducted using data from the 2014-2017 and 2019 Medical Expenditure Panel Survey (MEPS) to evaluate the association between shared decision-making and whether patients were satisfied with their care for psoriasis.20 Around 42% of patients had high shared decision-making scores (score, ≥ 3.9 of 4); these patients showed 85% higher satisfaction with care compared with those having lower scores (P < .001).20
In another study, Florek and colleagues performed a systematic review to determine patient preferences and satisfaction, which are linked to achieving therapeutic goals and QOL improvements.21 Patient preferences were influenced by factors such as age, gender, comorbidities, cost, treatment duration, and prior treatments, with some patients prioritizing the treatment process (eg, accessibility and delivery). The primary outcomes evaluated included the likelihood of experiencing treatment benefits and the potential for AEs.21 Notably, the results showed that satisfaction with current therapies was low, but patients treated with biologics reported the highest satisfaction compared with those given phototherapy or oral or topical treatments.21
Treatments should be chosen based on the patient’s disease severity, impact on QOL, response to previous therapies, and presence of comorbidities (eg, psoriatic arthritis, Crohn disease, malignancy, obesity, cardiac diseases, congestive heart failure, multiple sclerosis, and lupus).22 Consideration is also required for special populations, such as women who are pregnant, pediatric patients, and those with chronic infections, HIV, or latent tuberculosis.23
Patient-reported outcomes and QOL improvements have also been examined. Health-related QOL (HRQOL) was evaluated in patients with psoriasis who were treated with biologics in the PSOriasis Treated with BIOlogics in REAL Life study, a large, multinational, observational study.25 With higher levels of skin clearance, HRQOL and reduction in psoriasis symptoms were significantly improved.25
Real-World Evidence and Patient Registry
Real-world data were used to examine patient-perceived treatment efficacy, patterns of medication use, health care resource use, and medication costs in patients with psoriasis using a dermatology-specific electronic health record from a US population.25 The multicenter, longitudinal, retrospective, observational cohort study included adults 18 years or older with psoriasis who visited participating dermatology practices from September 1, 2014, to September 1, 2015. Among the 2200 patients evaluated, treatment was considered effective by 73% of patients using biologics, 61% of those using phototherapy, and 57% of patients using oral systemic medications.25
Considerations for Payers and Health Systems
Cost and Reimbursement Considerations
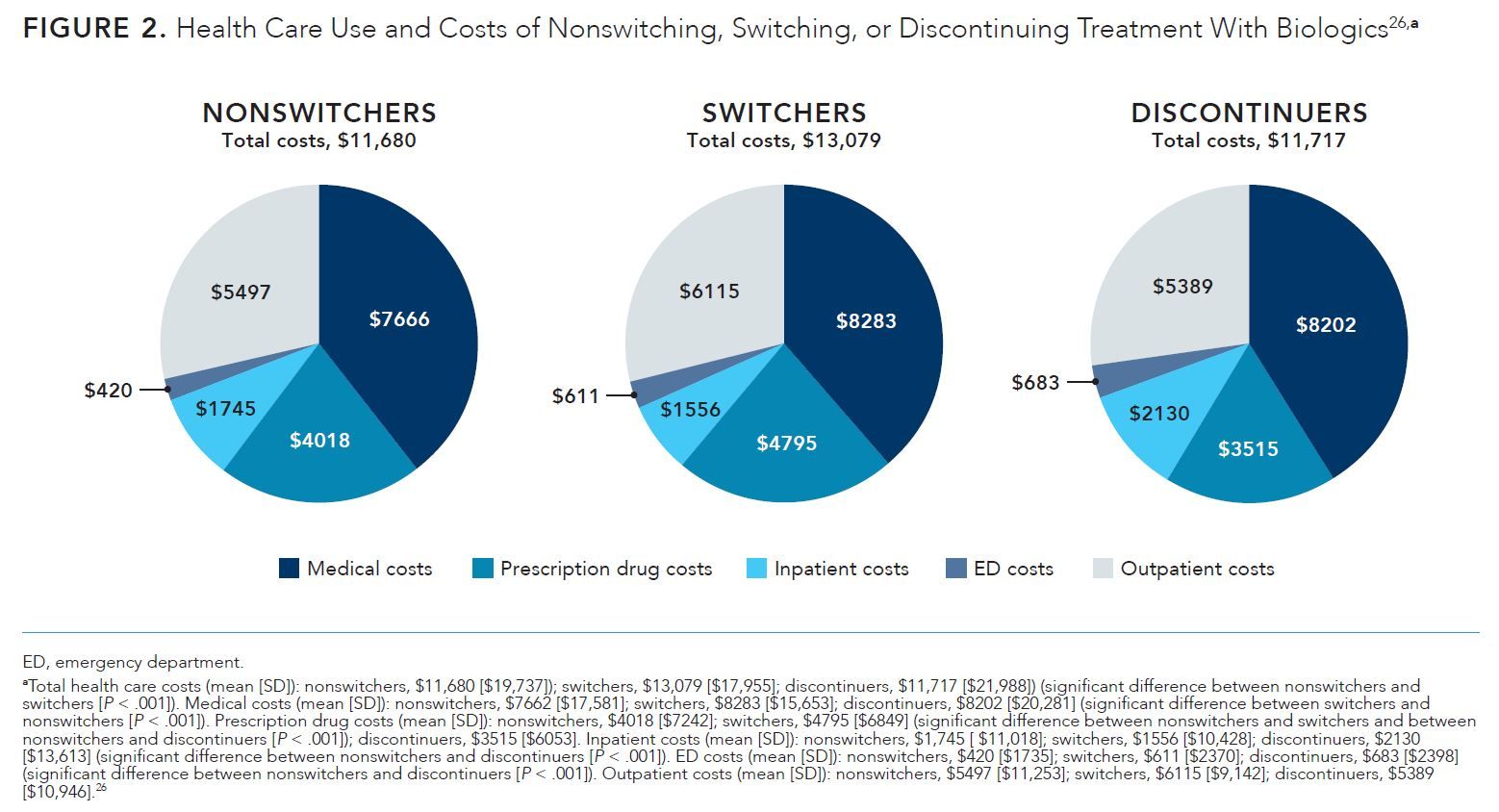
A study was performed to compare health care utilization use and costs of remaining, switching, or discontinuing treatment with biologics in patients with moderate to severe psoriasis compared with those for patients who remained on index therapy for 1 year.26 The study was a retrospective cohort analysis of Truven Health Analytics MarketScan Commercial Claims and Encounters Database and Medicare Supplemental and Coordination of Benefits Database from January 1, 2011, to June 30, 2016. Patients were evaluated as nonswitchers (remained on the index biologic for 1 year with no treatment gaps), switchers (had a prescription claim for a different biologic than the index biologic and switched therapies before reaching permissible treatment gaps [> 90 days for adalimumab, infliximab, and etanercept; > 120 day for ustekinumab]), or discontinuers (had prescription claim gaps during 1-year of follow-up [> 90 days for adalimumab, infliximab, and etanercept; > 120 days for ustekinumab]).26
The authors evaluated data from 8710 patients, comprised of 5000 nonswitchers (57.4%), 1001 switchers (11.5%), and 2709 discontinuers (31.1%). The mean (SD) all-cause total health care costs were higher for switchers than for nonswitchers (Figure 2).26 Additionally, medical and prescription drug costs were higher for switchers than for nonswitchers. Finally, compared with nonswitchers, discontinuers showed lower prescription drug costs and higher inpatient and emergency department costs.26 The results revealed the financial impact of treatment switching, which can guide formulary decisions for payers. Policy administrators should consider the costs and benefits of therapy changes for patients and physicians, potentially leading to adjustments in formulary tiering. Patients with psoriasis on biologics should be more closely managed to address both clinical and economic challenges.26
Budget Impact and Cost-Effectiveness Assessments
Hendrix and colleagues evaluated the relative effectiveness and cost-effectiveness of using targeted therapies as initial treatments in patients with moderate to severe plaque psoriasis; this type of analysis can help to determine whether newer drugs should be prioritized and to direct prescribing and clinical guidelines decisions.27 The authors constructed a cost-effectiveness acceptability curve that depicted the likelihood of each drug having the greatest net monetary benefit at varying willingness-to-pay thresholds per quality-adjusted life year (QALY). The results showed that for initial therapy, more effective drugs (eg, brodalumab [7.173 QALYs], ixekizumab [7.208 QALYs]) had greater value compared with less cost-effective drugs (eg, apremilast [6.403 QALYs], etanercept [6.505 QALYs]).27 Apremilast and infliximab were considered cost-effective options at lower willingness-to-pay thresholds ($100,000), whereas brodalumab, ixekizumab, and secukinumab were optimal choices at higher willingness-to-pay levels ($150,000).27
Risk-Sharing Agreements and Value-Based Contracts
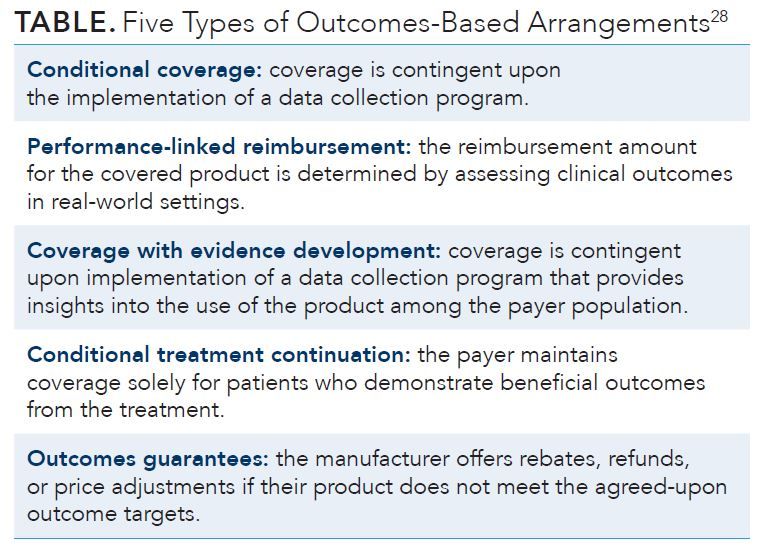
Reimbursement decisions are often made before the real-world value of a drug has been demonstrated.28 Financial risks are incurred by payers for drugs that may not be as effective as predicted, leading to “drug lag” (a delay in the availability of medications for patients before a health plan determines that the drug will be covered); drug companies must negotiate with payers to allow coverage and increase the market share.28 Performance-based risk-sharing arrangements can disperse the risk among both payers and drug manufacturers, which can decrease the time to which a drug is accepted for reimbursement and prevent resource waste (Table).28
PA and Step Therapy Requirements
Several policies mandate a step-edit approach for reimbursement, necessitating patients to demonstrate an inadequate response to topical and/or conventional systemic therapies before being eligible for biologic prescriptions.29,30 Implementing a step-therapy approach may result in undertreatment of patients with moderate to severe disease, limiting cost reduction.30 Poorer outcomes can lead to increased health care expenses because of worsening conditions and complications and the added resources required for utilization management (UM); however, the patient’s QOL should also be considered.31 In a study of claims data, 14% to 16% of patients had at least 1 claim that was rejected the first time they attempted to fill a prescription; also, the average time between the first and last attempts to fill a prescription before the patient gave up was 17 to 23 days (ie, patients do no persist in attempting to obtain medications if the prescription is not filled within 2.5-3.5 weeks).31 Delayed treatment through UM policies may have particularly negative effects on patients with psoriatic arthritis, given that delaying treatment by even 6 months can lead to damage to joints and long-term physical function.32
Treatment Sequencing Strategies
Treatment approaches for plaque psoriasis vary based upon factors such as the presence of psoriatic arthritis and severity of the disease, which is based on the affected body surface area (BSA).1 Mild psoriasis is typically defined as affecting up to 3% to 5% of the BSA; therapeutic recommendations include topical treatments (eg, corticosteroids, keratolytics, calcineurin inhibitors, vitamin D analogs, and/or targeted phototherapy).1 No consensus currently exists for the definition of moderate to severe psoriasis; the BSA for moderate psoriasis has been described as being both 3% to 10% and 5% to 10%.1 In contrast, psoriasis is typically considered severe when at least 10% of the BSA is affected.1 Treatments for moderate to severe psoriasis are largely systemic, involving biologics such as inhibitors for TNF-α, IL-17, and IL-12/-23 agents; oral medications such as methotrexate; and/or UVB/psoralen plus UVA phototherapy.1
Several effective and well-tolerated therapies for psoriasis exist, yet patients are often unsatisfied and undertreated, achieving suboptimal relief of symptoms or QOL improvements.33 This may occur when patients with mild to severe disease are treated by providers who are hesitant to switch or begin new systemic treatments.33 The reluctance to switch medications leads to many patients taking poorly tolerated medications for extended time periods, causing unnecessary escalation of symptoms.33
To optimize outcomes for patients, a prompt therapeutic change is recommended if at least an intermediate response is not achieved within 2 months or within the induction phase of biologics treatment.33 However, therapy alteration criteria are not well defined, and data on methods for switching therapies in routine clinical practice remain limited.33
Long-Term Monitoring Considerations
Nonadherence is the most common reason for nonresponse to medication. The rate of adherence to biologic therapy is better than that to oral therapy.34 Various strategies proposed to improve patient adherence include patient education (eg, written action plans, use of drawings, photographs, and videos), simplification of treatment regimens, reduction of treatment costs (eg, use of generic products), setting of early follow-up visits and short-term goals, and implementation of reminder programs (eg, emails, phone calls, text messages, and smartphone applications).34 Pharmaceutical manufacturers also provide patient education and support materials and have dedicated websites for these purposes.35,36
Future Perspectives and Emerging Therapies
Several biologic therapies are being studied as candidates for treating psoriasis. Therapies specific to plaque psoriasis that are currently being tested in phase 3 trials include deucravacitinib (POETYK PSO-3 [NCT04167462], POETYK PSO-4 [NCT03924427]) and bimekizumab (BE BRIGHT [NCT03598790], BE CONNECTED [NCT04718896]); sonelokimab has been tested in a 52-week, phase 2b study.37,38
Many of these targeted therapies use novel mechanisms of action. For example, deucravactinib is an oral selective TYK2 inhibitor; bimekizumab is a humanized immunoglobulin G1 antibody selective for IL-17A, IL-17F, and IL-17AF heterodimer; and sonelokimab is a trivalent camelid nanobody selective for IL-17A, IL-17F, and human serum albumin.37
Digital health and telemedicine also have impacted the management of psoriatic diseases. Telemedicine’s relatively recent emergence in health care has provided patients with a convenient and more accessible route of receiving treatment for psoriasis.39 Largely thanks to the COVID-19 pandemic, telemedicine use has drastically increased among dermatologists from less than 15% to over 95% following the pandemic.39 Although virtual medicine may seem less involved for patients, it allows an opportunity to take greater interest in their disease management, as they can provide physicians with self-taken images that can be used to assess their disease severity using PASI.39
Efficient teledermatology practices improve the dermatology QOL index as well as PASI and BSA scores compared with traditional in-person care.39 Telemedicine has made patient care more accessible. Barriers to care (eg, transportation, travel cost, distance, disability) are no longer a concern in such a system; telemedicine allows patients with psoriasis to receive care more expeditiously and to be more involved in their treatment, leading to improvements in QOL and treatment adherence.39
Conclusions
Plaque psoriasis presents a global health challenge, affecting millions worldwide and impacting public health. The connection of psoriasis with MetS underscores the intricacies of disease management. Recent treatment advances, particularly in the development of biologic agents, offer a transformative approach for patients and health care systems. The interplay between clinical efficacy, safety, and resource allocation necessitates a holistic approach to decision-making, aligning medical understanding with economic insights to optimize outcomes and overall well-being for those affected by plaque psoriasis.
References
- Armstrong AW, Read C. Pathophysiology, clinical presentation, and treatment of psoriasis: a review. JAMA. 2020;323(19):1945-1960. doi:10.1001/jama.2020.4006
- Armstrong AW, Mehta MD, Schupp CW, Gondo GC, Bell SJ, Griffiths CEM. Psoriasis prevalence in adults in the United States. JAMA Dermatol. 2021;157(8):940-946. doi:10.1001/jamadermatol.2021.2007
- Alwan W, Nestle FO. Pathogenesis and treatment of psoriasis: exploiting pathophysiological pathways for precision medicine. Clin Exp Rheumatol. 2015;33(5; suppl 93):S2-S6.
- Liu L, Cai XC, Sun XY, et al. Global prevalence of metabolic syndrome in patients with psoriasis in the past two decades: current evidence. J Eur Acad Dermatol Venereol. 2022;36(11):1969-1979. doi:10.1111/jdv.18296
- Merola JF, Kavanaugh A, Lebwohl MG, Gniadecki R, Wu JJ. Clinical efficacy and safety of psoriasis treatments in patients with concomitant metabolic syndrome: a narrative review. Dermatol Ther (Heidelb). 2022;12:2201-2216. doi:10.1007/s13555-022-00790-2
- Armstrong AW, Puig L, Joshi A, et al. Comparison of biologics and oral treatments for plaque psoriasis: a meta-analysis. JAMA Dermatol. 2020;156(3):258-269. doi:10.1001/jamadermatol.2019.4029
- Bagel J. Treatment strategies, management of comorbidities, and the role of IL-23 inhibitors in moderate to severe psoriasis. Am J Manag Care. 2021;27(27[10]; suppl):S203-S208. doi:10.37765/ajmc.2021.88675
- Kaplan DL, Ung BL, Pelletier C, Udeze C, Khilfeh I, Tian M. Switch rates and total cost of care associated with apremilast and biologic therapies in biologic-naïve patients with plaque psoriasis. Clinicoecon Outcomes Res. 2020;12:369-377. doi:10.2147/CEOR.S251775
- Kim HJ, Lebwohl MG. Biologics and psoriasis: the beat goes on. Dermatol Clin. 2019;37(1):29-36. doi:10.1016/j.det.2018.07.004
- Shear NH, Betts KA, Soliman AM, et al. Comparative efficacy and benefit-risk profile of biologics and oral treatment for moderate-to-severe plaque psoriasis: a network meta-analysis of clinical trial data. J Am Acad Dermatol. 2021;85(3):572-581. doi:10.1016/j.jaad.2021.02.057
- Kopp T, Riedl E, Bangert C, et al. Clinical improvement in psoriasis with specific targeting of interleukin-23. Nature. 2015;521(7551):222-226. doi:10.1038/nature14175
- Papp K, Thaçi D, Reich K, et al. Tildrakizumab (MK-3222), an anti-interleukin-23p19 monoclonal antibody, improves psoriasis in a phase IIb randomized placebo-controlled trial [published correction appears in Br J Dermatol. 2016 Jun;174(6):1426]. Br J Dermatol. 2015;173(4):930-939. doi:10.1111/bjd.13932
- Reich K, Papp KA, Blauvelt A, et al. Tildrakizumab versus placebo or etanercept for chronic plaque psoriasis (reSURFACE 1 and reSURFACE 2): results from two randomised controlled, phase 3 trials [published correction appears in Lancet. 2017 Jul 15;390(10091):230]. Lancet. 2017;390(10091):276-288. doi:10.1016/S0140-6736(17)31279-5
- Galluzzo M, Chiricozzi A, Cinotti E, et al. Tildrakizumab for treatment of moderate to severe psoriasis: an expert opinion of efficacy, safety, and use in special populations. Expert Opin Biol Ther. 2022;22(3):367-376. doi:10.1080/14712598.2022.1988566
- Fernandez AP, Dauden E, Gerdes S, et al. Tildrakizumab efficacy and safety in patients with psoriasis and concomitant metabolic syndrome: post hoc analysis of 5-year data from reSURFACE 1 and reSURFACE 2. J Eur Acad Dermatol Venereol. 2022;36(10):1774-1783. doi:10.1111/jdv.18167
- McInnes IB, Kavanaugh A, Gottlieb AB, et al. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet. 2013;382(9894):780-789. doi:10.1016/S0140-6736(13)60594-2
- Ritchlin C, Rahman P, Kavanaugh A, et al. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis. 2014;73(6):990-999. doi:10.1136/annrheumdis-2013-204655
- Ergen EN, Yusuf N. Inhibition of interleukin-12 and/or interleukin-23 for the treatment of psoriasis: what is the evidence for an effect on malignancy? Exp Dermatol. 2018;27(7):737-747. doi:10.1111/exd.13676
- Thatiparthi A, Martin A, Liu J, Egeberg A, Wu JJ. Biologic treatment algorithms for moderate-to-severe psoriasis with comorbid conditions and special populations: a review. Am J Clin Dermatol. 2021;22(4):425-442. doi:10.1007/s40257-021-00603-w
- Yee D, Kingston P, Lee K, et al. Shared decision-making and satisfaction with care in psoriasis patients: a population-based study in the United States. J Am Acad Dermatol. Published online April 1, 2023. doi:10.1016/j.jaad.2023.03.039
- Florek AG, Wang CJ, Armstrong AW. Treatment preferences and treatment satisfaction among psoriasis patients: a systematic review. Arch Dermatol Res. 2018;310(4):271-319. doi:10.1007/s00403-018-1808-x
- Kaushik SB, Lebwohl MG. Psoriasis: Which therapy for which patient: Psoriasis comorbidities and preferred systemic agents. J Am Acad Dermatol. 2019;80(1):27-40. doi:10.1016/j.jaad.2018.06.057
- Kaushik SB, Lebwohl MG. Psoriasis: Which therapy for which patient: focus on special populations and chronic infections. J Am Acad Dermatol. 2019;80(1):43-53. doi:10.1016/j.jaad.2018.06.056
- Lacour JP, Bewley A, Hammond E. et al. Association between patient- and physician-reported outcomes in patients with moderate-to-severe plaque psoriasis treated with biologics in real life (PSO-BIO-REAL). Dermatol Ther (Heidelb). 2020;10(5):1099-1109. doi:10.1007/s13555-020-00428-1
- Armstrong AW, Foster SA, Comer BS, et al. Real-world health outcomes in adults with moderate-to-severe psoriasis in the United States: a population study using electronic health records to examine patient-perceived treatment effectiveness, medication use, and healthcare resource utilization. BMC Dermatol. 2018;18(1):4. doi:10.1186/s12895-018-0072-2
- Feldman SR, Tian H, Wang X, Germino R. Health care utilization and cost associated with biologic treatment patterns among patients with moderate to severe psoriasis: analyses from a large U.S. claims database. J Manag Care Spec Pharm. 2019;25(4):479-488. doi:10.18553/jmcp.2018.18308
- Hendrix N, Ollendorf DA, Chapman RH. Cost-effectiveness of targeted pharmacotherapy for moderate to severe plaque psoriasis. J Manag Care Spec Pharm. 2018;24(12):1210-1217. doi:10.18553/jmcp.2018.24.12.1210
- Kim AE, Choi DH, Chang J, Kim SH. Performance-based risk-sharing arrangements (PBRSA): is it a solution to increasing bang for the buck for pharmaceutical reimbursement strategy for our nation and around the world? Clin Drug Investig. 2020;40(12):1107-1113. doi:10.1007/s40261-020-00972-w
- Stern D. Benefit design innovations to manage specialty pharmaceuticals. J Manag Care Pharm. 2008;14(4; suppl A):S12-S16. doi:10.18553/jmcp.2008.14.s4-a.12
- Feldman SR, Goffe B, Rice G. The challenge of managing psoriasis: unmet medical needs and stakeholder perspectives. Am Health Drug Benefits. 2016;9(9):504-513.
- Snow J, Feldman M, Kappel J. The impact of step-therapy policies on patients. Xcenda AmerisourceBergen. 2019. https://www.xcenda.com/-/media/assets/xcenda/english/content-assets/white-papers-issue-briefs-studies-pdf/impact-of-step-therapy-on-patients_final_1019.pdf
- Gondo G, Boles J, Stone P, Howard L, Bell SJ. Prevalence of utilization management policies among the psoriatic disease community: results from the 2019 National Psoriasis Foundation advocacy survey. J Psoriasis Psoriatic Arthritis. 2020;5(4):178-183. doi:10.1177/2475530320956602
- Kerdel F, Zaiac M. An evolution in switching therapy for psoriasis patients who fail to meet treatment goals. Dermatol Ther. 2015;28(6):390-403. doi:10.1111/dth.12267
- Eicher L, Knop M, Aszodi N, Senner S, French LE, Wollenberg A. A systematic review of factors influencing treatment adherence in chronic inflammatory skin disease - strategies for optimizing treatment outcome. J Eur Acad Dermatol Venereol. 2019;33(12):2253-2263. doi:10.1111/jdv.15913
- Patient education resources. Dermatology. Lilly. Updated August 2023. Accessed August 16, 2023. https://education.lillymedical.com/en-us/patient-education-resources/dermatology/psoriasis
- Psoriasis. Johnson & Johnson. Accessed August 16, 2023. https://www.jnj.com/tag/psoriasis
- Lin CP, Merola JF, Wallace EB. Current and emerging biologic and small molecule systemic treatment options for psoriasis and psoriatic arthritis. Curr Opin Pharmacol. 2022;67:102292. doi:10.1016/j.coph.2022.102292
- Papp KA, Weinberg MA, Morris A, Reich K. IL17A/F nanobody sonelokimab in patients with plaque psoriasis: a multicentre, randomised, placebo-controlled, phase 2b study [published correction appears in Lancet. 2021 Jun 5;397(10290):2150]. Lancet. 2021;397(10284):1564-1575. doi:10.1016/S0140-6736(21)00440-2
- Pelet Del Toro N, Yahia R, Feldman SR, et al. National Psoriasis Foundation Telemedicine Task Force guidance for management of psoriatic disease via telemedicine. JAAD Int. 2023;12:32-36. doi:10.1016/j.jdin.2023.02.018
