- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
ASCO President Reviews Post-SGR Challenges for Oncologists
At the Patient-Centered Oncology Care 2015 meeting, held November 19-20, 2015, in Baltimore, Maryland, keynote speaker Julie M. Vose, MD, MBA, FASCO, president of the American Society of Clinical Oncology provided perspectives on the challenges faced by oncologists as the healthcare system transitions to define and incorporate value in the care delivered.
At the Patient-Centered Oncology Care 2015 meeting, hosted by The American Journal of Managed Care in Baltimore November 19-20, 2015, keynote speaker Julie M. Vose, MD, MBA, FASCO, president of the American Society of Clinical Oncology (ASCO) provided perspectives on the challenges faced by oncologists as the healthcare system transitions to define and incorporate value in the care delivered.
"Unfortunately, there is an administrative burden that physicians have to bear and so there’s not much time to spend with the patient,” she said, adding, “We have to take this back to the patient and physicians need to ensure that they are don’t just turn into data-entry operators,” hinting at the growing administrative burden faced by physicians.
Achieving the triple aim of better care, improved heath, and lower costs—all in a value-based manner—are a physician’s goals, “But how do we get there?” queried Dr Vose. She indicated that the answer is enveloped in multiple layers:
- We need to make sure evidence-based practices are followed
- Available resources should be efficiently used
- Quality measures and improvement are vital
- Practices need adequate support to avoid duplication of efforts and improve patient engagement to provide better care in a value-based manner
- Oncology is based on innovation and new treatments should be value-based.
Pointing to CMS’ emphasis on transitioning from the fee-for-service (FFS) to value-based care, Vose said that FFS drives volume without necessarily ensuring quality. “The administration has set an ambitious goal of at least 50% of all Medicare payments based on alternative payment models by 2018. I dont think this is possible by 2018 though,” she said.
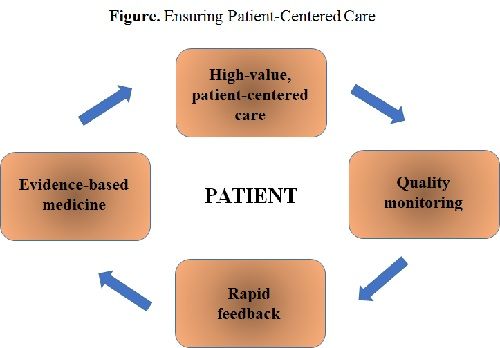
Dr Vose emphasized that patient care should achieve the highest-value level. “Cost and toxicity should be incorporated into the value proposition and we need to move beyond process measures and ensure outcomes improve with the value-based changes,” she added (Figure).
Most quality measures today are process-based, said Vose, and pointed to ASCO’s QOPI project that allows for performance measurement and feedback. In addition to process measures, QOPI site visits ensure meeting QOPI certification. Additionally, mentorship programs allow data exchange and further help dissipate the model, she said.
How has ASCO improved on these essential requirements?
It’s been a multi-pronged approach through the efficient use of Choosing Wisely; PracticeNet, a suite of services to allow value-based care and improve clinic practices; and team-based care, which is extremely important, especially with the increased need for oncologists as the rate of patients with cancer rises.
Dr Vose then explained that ASCO’s Value Framework has tried to incorporate all of these factors: shared decision-making, added benefit vs existing therapy, meeting individual patient goals and circumstances.
Dr Vose then talked about the Merit-Based Incentive Payment System (MIPS), which came into being after Medicare Authorization and CHIP Reauthorization Act or MACRA replaced the Sustainable Growth Rate (SGR), which was a big step forward, but has created new needs. While this would bring about a significant change and create a big opportunity to improve patient care. Physicians can use MIPs or alternative payment models—they are a new way to look at performance measurement. However, there’s public reporting via Physician Compare is a big change that physicians would have to adapt to. “However, although the SGR is gone, we are still cutting up one pie. The size of positive updates or bonuses depends on how many people get penalties for not performing. This is new. And scary,” Dr Vose added.
MIPS will significantly impact the physician payment program in terms of dollar cost, she said, in primarily 4 domains: resource use, quality reporting, HER, and clinical improvement activities. “The information will be collected beginning 2017 to be implement in 2019. We need tools to help with gap in care coordination that don’t currently exist,” Dr Vose added.
Oncologists, though, are feeling unprepared according to Dr Vose. “While the goals providers have been striving to meet are still the same, such as meeting national benchmarks for quality in the form of performance measures, making use of EHRs, continually improving our clinical care, and doing it in the most efficient way possible, challenges remain.” Measurement tools remain the major challenge.
“And MACRA comes at a time when there is already significant turbulence in the oncology practice community,” Dr Vose emphasized.
Oncologists face a lot of practice pressures, and they vary based on physician-owned community practices, academic, or health centers. “Smaller practices are our special concern; they are the backbone of the US oncology care delivery system. But the current trend is toward consolidation, which is modifying the face of oncology.”
Information overload is not helping oncologists either, whether it be clinical information or administrative adaptations with new rulings and requirements. “There are also administrative overloads; we know of a practice that had 8 different clinical pathways for each of the payers they worked with.”
Indicating that APMs can help achieve transformation, Vose said that ASCO’s patient-centered oncology payment model tries to match support with the work being done to avoid cost-shifting to patients. “It’s a big collaborative project and we plan to data-share to get feedback for improvement,” Dr Vose said.
How do we agree on improving on pathways and value measures?
While rapid-learning systems would improve efficiency of care, there are challenges that need to be met:
- Need new ways to test drugs per tumor’s molecular characteristics, eg, NCI-MATCH, TAPUR
- Learn from every patient (irrespective of trial participation)
- Harness data in powerful new ways.
“The patient needs to be the center of what we are doing: improve outcomes, reduce side effects and do this in a value-based manner. We need to harness our collective wisdom as we do this,” Dr Vose ended.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
