- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
ASCENT Trial: Optimizing TKI Therapy for EGFR-Mutant NSCLC Challenges
Investigators continue to seek more information on how to optimally integrate treatment with tyrosine kinase inhibitors (TKIs) into an established concurrent chemoradiotherapy regimen.
New data from the phase 2 ASCENT trial show there is still an unmet need to optimize induction and consolidation therapy with tyrosine kinase inhibitors (TKIs) for patients who have EGFR-mutant locally advanced non–small cell lung cancer (NSCLC), but that long-term disease control is possible, as is cure, following treatment with afatinib.
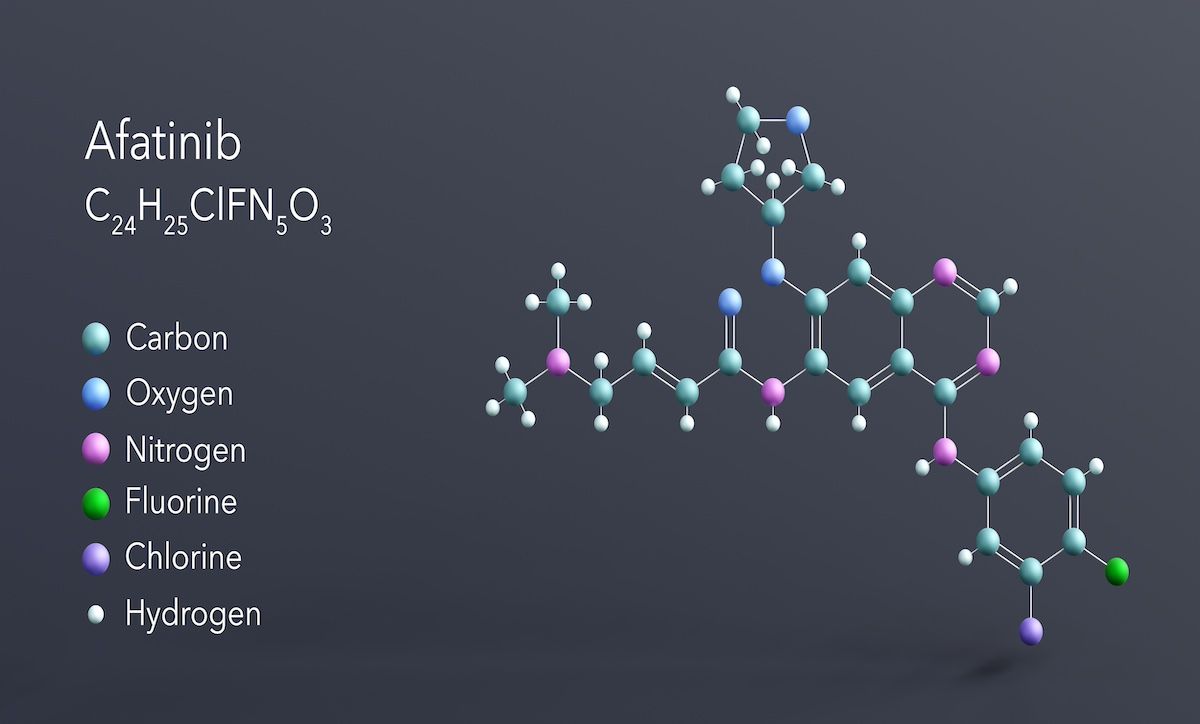
In ASCENT (NCT01553942), the kinase inhibitor afatinib was investigated for its efficacy and safety when administered with concurrent chemoradiotherapy (cCRT) in patients with locally advanced NSCLC; this study was completed in December 2021.1 Publishing their findings in The Oncologist, the study authors noted the findings from their current analysis are in sharp contrast to the overall established effective role of TKIs in early-stage and metastatic oncogene-driven NSCLC.2
All patients in their analysis (N = 19) had histologically confirmed, locally advanced stage III NSCLC, with an activating EGFR mutation confirmed with next-generation sequencing or a polymerase chain reaction–based assay. Induction treatment involved daily oral 40-mg afatinib for two 4-week cycles; if no disease progression, patients went on to received cCRT with preoperative (45-54 Gy) or definitive dosing (up to 72 Gy). Concurrent chemotherapy was intravenous 75-mg/m2 cisplatin plus 500-mg/m2 pemetrexed for 2 cycles if concurrent RT was preoperative or 4 cycles when concurrent RT was for being given for up to 4 weeks.
The primary end point was objective response rate and secondary end points were safety, conversion to operability following induction afatinib, progression-free survival (PFS), and overall survival (OS). Median patient age was 56 years (range, 34-75), 74% were female patients, 68% were White patients, 32% were Asian patients, 53% were former tobacco users, all had adenocarcinoma, exon 19 deletion was the most common EGFR mutation (58%), and the most common disease stage, per American Joint Committee on Cancer 7th Edition, was stage IIIb (T1-4 N2-3) in 58%.
Seven patients in this analysis completed a 2-year course of treatment with afatinib, with a median time on treatment of 1.73 years| Image Credit: Сергей Шиманович-stock.adobe.com
“This is the final report of the ASCENT study, which was designed in the pre-osimertinib era to assess whether afatinib, a second-generation, irreversible, pan-ERBB TKI could be safely incorporated both before and after trimodality therapy or definitive cCRT in patients with locally advanced EGFR-mutant lung adenocarcinoma,” the study authors wrote.
All patients underwent and completed 2-month afatinib induction, after which 10 patients went on to receive neoadjuvant cCRT and surgery and 7 patients received definitive cCRT. Two patients who were found to have metastatic disease did not receive cCRT. Among those who underwent surgery, the median radiation dose was 54 Gy and median chemotherapy cycles, 2, and among those receiving definitive cCRT, these were 66.6 Gy and 3, respectively.
Of the 7 patients who completed the planned 2 years of consolidation afatinib, median time on treatment was 1.73 years. The overall response rate to afatinib was 63% (95% CI, 38%-84%).
Following afatinib induction and cCRT, 10 patients had a lobectomy and nodal dissection, and among this group, there were 5 major pathologic responses and 1 pathologic complete response (a patient formerly diagnosed with unresectable disease). A second patient also though to initially have unresectable disease underwent surgery and had a major pathologic response.
The median follow-up was 5.04 years among the 8 of 19 patients who were alive at the time of the authors’ analysis. These patients also had a median PFS of 2.63 years and a median OS of 5.76 years. Three of these patients remain alive with no evidence of recurrence, with 1 stopping scans soon after stopping the trial protocol.
Of the 12 patients who received only consolidation afatinib, their median PFS was 2.9 months after stopping afatinib; 11 of the 12 experienced disease progression. Their reasons for treatment discontinuation were toxicity (n = 5) and completed the treatment course (n = 7).
Adverse events (AEs) were consistent with prior research. Common grade 3 AEs were diarrhea, nausea, vomiting, mucositis, febrile neutropenia, rash. and paronychia, and grade 2 AEs were pneumonitis and esophagitis. There were no grade 4/5 AEs.
As research has seen median survival for stage III NSCLC increase from 16 months to 47 months, from the late 1990s to today with immune checkpoint inhibition now a treatment option, the authors highlight that targeted treatment with TKIs has become a standard of care for metastatic oncogene-driven NSCLC—just without clinical trial data on their use against locally advanced disease.
“If targeted TKIs are rarely curative, how can they be most effectively combined with other treatment modalities to achieve cure? Are TKIs most effective in the neoadjuvant/induction setting or the adjuvant/consolidation setting?,” the authors asked. “ASCENT was not designed to test the independent contributions of induction vs consolidation TKI, but its findings nonetheless establish important starting points for future trial design.”
References
1. Afatinib sequenced with concurrent chemotherapy and radiation in EGFR-mutant non-small cell lung tumors: the ASCENT trial. ClinicalTrials.gov. Updated July 7, 2020. Accessed May 20, 2024. https://clinicaltrials.gov/study/NCT01553942
2. Chang AEB, Piper-Vallillo AJ, Mak RH, et al. The ASCENT trial: a phase 2 study of induction and consolidation afatinib and chemoradiation with or without surgery in stage III EGFR-mutant NSCLC. Oncologist. Published online May 18, 2024. doi:10.1093/oncolo/oyae107
