- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
An Increase in Telehealth Utilization in the South From July to August 2021
The August telehealth growth coincided with the peak of the surge in COVID-19 cases driven by the Delta variant in the South.
Telehealth utilization in the South, measured as a percentage of all medical claim lines in that region, rose 12.9% from July to August 2021, increasing from 3.1% of medical claim lines in July to 3.5% in August (FIGURE 1). Telehealth utilization in August rose nationally (by 2.4%) and in all US census regions except the Midwest, but the growth in the South surpassed that in all other geographical areas. Reported by FAIR Health’s Monthly Telehealth Regional Tracker, the data represent the privately insured population, including Medicare Advantage and excluding Medicare Fee-for-Service and Medicaid.
FIGURE 1. Monthly Telehealth Regional Tracker, July versus August 2021, South
Source: FAIR Health
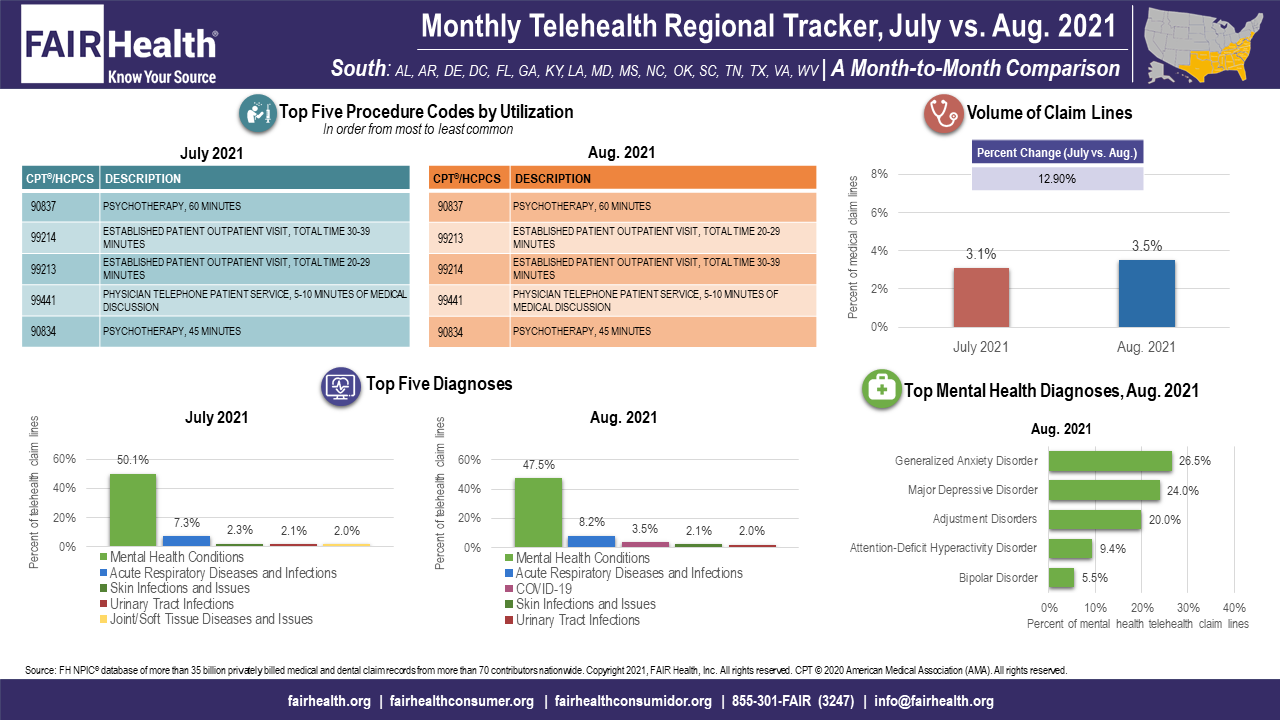
Nationally and in the South, the increase in August halted 2 months of decline in telehealth utilization, in June and July. The August telehealth growth coincided with the peak of the surge in COVID-19 cases driven by the Delta variant in the South. This may suggest that the increase in telehealth use has been propelled by patients and providers seeking a venue of care that reduced the risk of disease transmission.
COVID-19 itself joined the top 5 telehealth diagnoses nationally in August 2021, the first time it had done so since January 2021. While COVID-19 ranked at number 5 among telehealth diagnoses nationally in August, it ranked at number 3 in the South. The only region where it did not appear in the top 5 was the Northeast.
Mental health conditions remained the top-ranking telehealth diagnosis nationally and in every region, but from July to August 2021 this diagnosis declined in percentage share of all telehealth claim lines nationally and in every region (FIGURE 2). The decline, which had begun nationally from June to July, was greatest in the South, where mental health conditions’ share of telehealth claim lines fell from 50.1% in July to 47.5% in August. The decrease may have been related to having a greater share of nonmental health conditions, including COVID-19, move to telehealth because of the recent pandemic surge.
FIGURE 2. Monthly Telehealth Regional Tracker, July versus August 2021, United States
FAIR Health
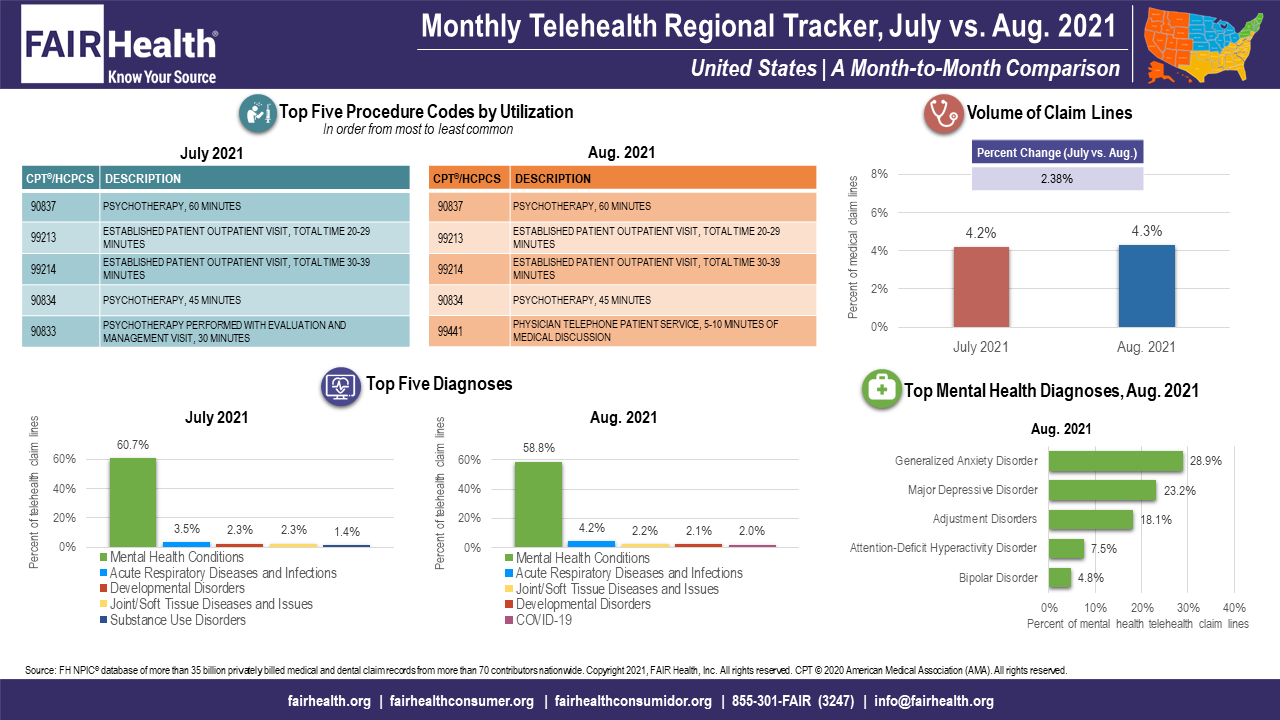
Among the top 5 mental health diagnoses, post-traumatic stress disorder (PTSD) appeared in August 2021 in the number 5 rank in the Northeast, displacing bipolar disorder. It was the first time in months that PTSD had ranked among the top 5 mental health diagnoses in any region but the Midwest, where it remained at number five in August.
Nationally in August 2021, CPT 99441, physician telephone patient service, 5 to 10 minutes of medical discussion, joined the top 5 telehealth procedure codes by utilization. Ranking at number 5, it displaced CPT 90833, psychotherapy performed with evaluation and management visit, 30 minutes.
About the Monthly Telehealth Regional Tracker
Launched in May 2020 as a free service, the Monthly Telehealth Regional Tracker uses FAIR Health data to track how telehealth is evolving from month to month. An interactive map of the four US census regions allows the user to view an infographic on telehealth in a specific month in the nation as a whole or in individual regions. Each infographic shows month-to-month changes in volume of telehealth claim lines, top five telehealth procedure codes and top five telehealth diagnoses (or diagnostic categories), along with that month’s top five granular diagnoses within the most common diagnostic category.
As the COVID-19 pandemic evolves, FAIR Health’s Monthly Telehealth Regional Tracker continues to shed light on changes in telehealth. This is one of many ways we pursue our healthcare transparency mission.
For the Monthly Telehealth Regional Tracker, click here.
About the Author
Robin Gelburd, JD, is the founding President of FAIR Health, a national, independent nonprofit organization that serves as a trusted leader in healthcare cost transparency, data analytics and benchmarks. FAIR Health possesses the nation’s largest collection of private healthcare claims data, which includes over 35 billion claim records and grows at a rate of over 2 billion claim records a year. Certified by the CMS as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D. Gelburd is a nationally recognized expert on healthcare policy and health literacy and transparency. Selected as one of Crain’s 2019 Notable Women in Health Care, she has been invited to speak to organizations and federal and state agencies across the country and world.
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
